Abstract
The aim of this study was to evaluate patients with vocal fold polyps using laryngeal electromyography (LEMG) for the presence of vocal fold paresis and to compare transnasal fiberoptic and rigid stroboscopic findings between polyp patients with normal LEMG and with vocal fold paresis. Thirty-five patients with a vocal fold polyp underwent transnasal fiberoptic laryngoscopy, rigid laryngostroboscopy, and LEMG. The findings were compared between the LEMG-confirmed vocal fold paresis patients and the normal LEMG patients. LEMG resulted in a diagnosis of unilateral or bilateral vocal fold paresis in 17 of 35 patients (48.6 %). More men than women with vocal fold polyps had vocal fold paresis (p < 0.05). The vocal fold paresis group had higher presence of axial rotation and hypomobility of vocal folds, higher asymmetry of vertical height of vocal folds, and less presence of longitudinal stretch of vocal folds (p < 0.05). Medial–lateral compression of the false vocal folds and anterior–posterior approximation of the larynx did not show any difference between the groups. No significant difference was found in vibratory wave characteristics between the groups through rigid laryngostroboscopy. Vocal fold paresis was present in almost half of the patients with vocal fold polyps. Paresis can only be accurately diagnosed with LEMG. Transnasal fiberoptic laryngoscopic examination is helpful to recognize vocal fold paresis in vocal fold polyp patients, while stroboscopic examination is not useful to identify it in vocal fold polyp patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vocal fold polyps are benign, round, sessile or pedinculated lesions located on the free borders of the vocal folds. Several factors seem to influence the development of vocal fold polyps, such as vocal misuse or abuse, allergy, smoking, chronic infections of the upper airways, and laryngopharyngeal reflux [1–6].
Vocal fold paresis is a clinical condition involving partial paralysis of a vocal cord that requires greater clarification. The clinical presentation of vocal fold paresis may include subtle axial rotation of the posterior larynx, incomplete glottal closure, vibratory asymmetry, or prominent vocal fold hypomobility and bowing, depending on the laryngeal nerve involved and the degree of the neuromuscular deficit [7–9]. The wider use of laryngeal electromyography (LEMG) in clinical practice allows clinicians to more accurately identify vocal fold paresis.
There are very few reports which present paresis of one or more of the laryngeal nerves in the literature [9–14]. A detailed review of these retrospective case studies revealed that benign vocal fold lesions such as nodule, polyp, cyst, and granuloma were accompanied by paresis in some of the patients [10, 12, 13]. Comorbidity of vocal fold paresis with benign vocal fold lesions, such as a vocal fold polyp, can be especially important to achieve satisfactory treatment results. Because the presence of a vocal fold polyp is typically the prominent finding that requires treatment, an accompanying vocal fold paresis can easily be overlooked if it is not suspected as a result of clinical findings. This may result in an unsatisfactory voice outcome. The literature does not contain any study that evaluates the presence of vocal fold paresis accompanying vocal fold polyp or that tries to identify examination findings which could lead to a suspicion of comorbid vocal fold paresis.
The purposes of this study were to prospectively evaluate patients presenting with a vocal fold polyp using LEMG for a diagnosis of vocal fold paresis and also to identify transnasal fiberoptic and laryngostroboscopic findings that may help to differentiate vocal fold polyp patients with a normal LEMG from those with vocal fold paresis.
Methods
Institutional Review Board approval was obtained from our institution before the study commenced. Patients who had been diagnosed with a vocal fold polyp between October 2011 and November 2013 were asked to participate in this prospective study. The patients were informed about the study and their signed written consents were obtained. Exclusion criteria included age below 18 years, history of radiation therapy for neck, presence of complete immobility of the vocal fold (suggestive of paralysis or fixation), leukoplakia, and malignancy.
During the study period 35 patients diagnosed with a vocal fold polyp agreed to participate in this study. This included 13 (37.1 %) female and 22 (62.9 %) male. The mean age was 38.9 years (range 22–59 years). The mean time interval from the onset of symptoms to presentation at the clinic was 2 years (range 1 month–10 years). Three (8.6 %) patients had a giant polyp, 7 (20 %) patients had a contact lesion on the contralateral side, 2 (5.6 %) patients had bilateral Reinke’s edema in addition to a polyp, 2 (5.6 %) patients had contralateral vocal fold edema, and 1 (2.8 %) patient had sulcus vocalis on the same side as the polyp.
Patients were asked to complete the Glottal Function Index (GFI) and Reflux Symptom Index (RSI) [15, 16]. The GFI is a 4-item symptom index used to assess the four main symptoms of glottal dysfunction: effortful speaking, vocal pain after talking, vocal fatigue, and pitch breaks. The patient is asked to rate his/her voice symptoms during the past month on a scale from 0 (no problem) to 5 (severe problem). A score of 20 represents maximum symptom severity, and a total score greater than four is considered to be abnormal [15]. The RSI is a 9-item self-administered outcomes questionnaire for evaluating symptoms of laryngopharyngeal reflux. Each item is scored between 0 (no problem) and 5 (severe problem), with a maximum total score of 45. An RSI of greater than 13 is considered to indicate laryngopharyngeal reflux [16].
All patients underwent the following evaluations: (1) a complete medical history and review of systems; (2) transnasal fiberoptic laryngoscopy; (3) rigid laryngostroboscopy; and (4) LEMG.
The larynx was first visualized through a transnasal fiberoptic endoscope with illumination provided by the halogen light, then with a 70° transoral rigid endoscope (Karl Storz, Tuttlingen, Germany) attached to a CCD camera and Storz Pulsar Stroboscope (Karl Storz, Tuttlingen, Germany). All laryngoscopic examinations were made by the same otolaryngologist (S.A.) with the same protocol and later reviewed and rated by her on standard protocol sheets. The examination recordings were played back using the same equipment used for the original recording and viewed on the same monitor.
The transnasal fiberoptic examination included speech and nonspeech tasks for assessing glottal closure, supraglottic hyperfunction, and degree of abduction and adduction. Patients were asked to sniff repetitively, to alternate between a sniff and /i/ vowel repeatedly, to alternate between /i/ and /hi/ vowels repeatedly, and also to repeat the phrase /pa/-/ta/-/ka/. The glissando maneuver, from low to high tone and then from high to low tone, was performed to evaluate longitudinal stretching of the vocal cords and axial rotation. Supraglottic hyperfunction was assessed during counting from ‘1’ to ‘10’ and also during running speech [11, 17].
During transoral rigid laryngoscopy, patients were instructed to phonate /i/ vowel at low, modal, and high frequencies with a stroboscopic light (Pulsar Stroboscope, Karl Storz, Tuttlingen, Germany). Glottal closure configuration and vibratory wave characteristics (amplitude, symmetry, periodicity, and mucosal wave) were evaluated. The stroboscopic signs and rating categories are shown in Table 1. The ratings were based on visualization of the patients’ modal pitch, at comfortable loudness phonation according to the criteria found in Hirano’s book on videostroboscopy [18]. Amplitude of the vocal fold vibration, mucosal wave and vibratory behavior were rated separately for each vocal fold.
Laryngeal electromyography was performed within 2–3 weeks after the laryngoscopic examination. The needle electrodes were inserted by the otolaryngologist (S.A.), and the operation of the electromyography machine and interpretation of the signal were done by the neurologist (R.A.I.). The neurologist was blinded to the findings of the laryngoscopic examination in all cases. Electromyography was performed with a Nihon Kohden-Neuropack (Tokyo, Japan) MEB-5504K electromyography machine with 45 mm × 26 G concentric needle electrodes (Myoline®, Spes Medica, Genoa, Italy). Needle placement and position were confirmed with standard percutaneous laryngeal electromyographic techniques [19–21]. The left cricothyroid, right cricothyroid, left thyroarytenoid, and right thyroarytenoid muscles were evaluated routinely. Placement into the cricothyroid muscle was confirmed by the presence of increased recruitment during a high-pitched /i/ and less recruitment during a low-pitched /i/. Placement into the thyroarytenoid muscle was confirmed by the presence of recruitment during speech or sustained phonation of the vowel /i/, combined with the presence of silence during active inspiration and sniffing. Phonation was tested at moderate intensity (normal speaking level).
Three to five different sites were evaluated within each muscle. The placement of needle near individual motor units was confirmed with the characteristic crisp sound and fine biphasic motor unit potentials. The low-frequency filter was set at 20 Hz, and the high-frequency filter was set at 10 kHz. For insertional and spontaneous activity a sweep speed of 10 ms per division and gain of 50 µV per division were used. Motor unit action potential (MUAP) morphology, amplitude, duration, and recruitment were assessed at sweep speeds of 10–20 ms and at gains of 200–500 µV.
The analysis of EMG data included assessment of insertional activity, spontaneous activity, amplitude of MUAP, MUAP duration, MUAP morphology during volunteer muscle activity, and recruitment pattern. Presence of full recruitment and normal MUAP, absence of spontaneous activity and of reinnervation MUAPs or polyphasic MUAPs was defined as “Normal” LEMG (Fig. 1). The diagnosis of neuropathy (i.e., paresis) was confirmed when there was one or more of the following “abnormal” LEMG findings in the muscle: presence of decreased recruitment, increased MUAP duration and amplitude, polyphasic MUAPs, spontaneous activities such as fibrillation potentials, or positive sharp waves [13, 21–23] (Figs. 2, 3).
The transnasal fiberoptic evaluation and rigid stroboscopic examination findings were compared between the LEMG-confirmed vocal fold paresis patients (Polyp with Paresis Group) and the normal LEMG patients (Polyp with Normal LEMG Group).
Statistical analysis
The statistical data were conducted using Number Cruncher Statistical System (NCSS) 2007 (NCSS LLC, Kaysville, UT, USA) and Power Analysis and Sample Size (PASS) 2008 for Windows (NCSS LLC, Kaysville, UT, USA). Metric data are presented as mean ± SD. Descriptive statistics were calculated for numeric variables. The comparison of quantitative data was done using the Mann–Whitney U test. In qualitative analyses, Fisher’s exact test, Fisher–Freeman–Halton exact test, and Yates’ continuity correction test were used. A p value <0.05 was considered to be statistically significant.
Results
Laryngeal electromyography resulted in a diagnosis of unilateral or bilateral vocal fold paresis in 17(48.6 %) of the 35 patients with a vocal fold polyp. Unilateral neuropathic findings were found in 11(31.5 %) patients and bilateral findings in 6 (17.1 %) patients. Unilateral neuropathies included both “ipsilateral” (i.e., on the side of the vocal fold with a polyp) and “contralateral” (i.e., on the side of the vocal fold without a polyp) neuropathies.
Of the 11 patients with unilateral neuropathy, ipsilateral combined recurrent laryngeal nerve (RLN) neuropathy and superior laryngeal nerve (SLN) neuropathy were found in 5 (14.3 %) patients; ipsilateral SLN neuropathy in 3 (8.5 %) patients; contralateral RLN neuropathy in 2 (5.6 %) patients; and ipsilateral RLN neuropathy in 1 (2.8 %) patient. Neuropathy was found in three nerves in 5 (14.3 %) patients and in four nerves in 1 (2.8 %) patient. Table 2 summarizes the LEMG findings.
Comparison of the patients with vocal fold paresis and with normal LEMG revealed that more men than women with vocal fold polyps also had vocal fold paresis (p = 0.049; Table 3). The mean RSI of the patients with normal LEMG was significantly higher than that of the patients with vocal fold paresis (p = 0.024; Table 3). Other than these there were no differences in age, polyp side, duration of the symptoms, and GFI between the groups (p > 0.05).
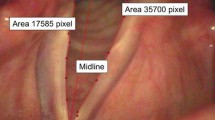
The distributions of transnasal fiberoptic laryngoscopic examination findings of the groups are displayed in Table 4. All the patients in the Polyp with Paresis Group had medial–lateral compression of the false vocal folds while 22.2 % (4/18) of the patients in the Polyp with Normal LEMG Group revealed no medial–lateral compression of the false vocal folds, but the difference between the distribution of medial–lateral compression of the groups was not found to be statistically significant (p = 0.098). The distribution of anterior–posterior approximation of the larynx also did not show any difference between the groups (p = 0.621). The presence of axial rotation, asymmetry of vertical height of vocal folds, hypomobility of vocal folds, and presence of longitudinal stretch of vocal folds were the findings that showed statistically significant differences between the groups (Table 4). The Polyp with Paresis Group had a higher presence of axial rotation (ipsilateral or contralateral), higher asymmetry of vertical height of vocal folds, more patients with hypomobility of vocal fold (ipsilateral or contralateral), and fewer patients with presence of longitudinal stretch of the vocal folds (p < 0.05).
Laryngeal electromyography revealed one patient who presented ipsilateral vocal fold fatigue with paresis on the same side. LEMG also revealed a patient with contralateral recurrent laryngeal nerve neuropathy who showed bowing of the contralateral vocal fold. That patient also revealed hypomobility of the contralateral vocal fold and axial rotation to the contralateral side, as well as medial–lateral compression and anterior–posterior approximation in the fiberoptic examination. The other patient with contralateral vocal fold paresis had only medial–lateral compression of the false vocal folds and anterior–posterior approximation of the larynx.
In 12 (70.6 %, 12/17) patients of the Polyp with Paresis Group there was at least one of the fiberoptic examination findings other than medial–lateral compression of the false vocal folds and anterior–posterior approximation of the larynx. Five (29.4 %, 5/17) of the Polyp with Paresis Group exhibited only supraglottic hyperfunction and did not have any other fiberoptic examination findings giving rise to a suspicion of paresis.
Transoral rigid stroboscopic evaluation showed no significant differences between the groups in distribution of glottal closure configuration or of any vibratory wave characteristics including amplitude, mucosal wave, vibratory behavior, phase symmetry, and periodicity (p > 0.05) (Table 5).
Discussion
Vocal fold paresis is incomplete paralysis in which some gross vocal fold mobility is preserved. Many inexplicable patient symptoms and indefinite laryngoscopic examination findings have been associated with mild neurologic deficit of the vocal folds [7]. Subtle laryngeal asymmetries observed with laryngoscopic examination may be defined as paresis, but LEMG is used to confirm the diagnosis [7, 11, 14].
In a study by Heman-Ackah and Batory, 33 patients had benign vocal fold lesions, such as a polyp, cyst, edema, granuloma etc., in 61 patients with clinically defined vocal fold hypomobility. But the confirmation of vocal fold paresis with LEMG was not done in this study [12]. The coexistence of vocal fold mucosal lesions was found in 11 of 19 patients with clinical- and LEMG-confirmed vocal fold paresis in the case series of Heman-Ackah and Barr [13]. Dursun et al. [10] reported that vocal fold mucosal lesions such as polyp, cyst, nodule, etc. were observed in 27.7 % of 126 patients with LEMG-confirmed superior laryngeal nerve paresis or paralysis.
In our prospective study 48.6 % (17) of 35 patients with a vocal fold polyp revealed vocal fold paresis with LEMG and 31.5 % of patients (11 patients, including 6 bilateral paresis and 5 unilateral SLN and RLN paresis) showed paresis of more than one laryngeal nerve. There is no other study available in the literature which investigated the presence of vocal fold paresis in vocal fold polyps.
Actually the incidence of vocal fold paresis has not been well demonstrated, but the few reports from tertiary laryngology practices suggest that vocal fold paresis is not common. Merati et al. [8] reported 29 patients of vocal fold paresis in a year. Heman-Ackah and Barr [13] identified 19 patients over a 13-month period. Simpson et al. [14] presented 13 patients of paresis over 4 years and Koufman et al. [11] reported 50 patients over 4 years. It should be emphasized that all these data are from retrospective chart reviews. Taking into account these studies, the considerably high percentage of incidence of vocal fold paresis in patients with a vocal fold polyp in our study is noteworthy. Not all the patients with a vocal fold polyp agreed to participate in the LEMG study because of apprehension of the procedure, so we may have had patient selection bias on the part of the potential participants. It is possible that more patients with vocal fold polyp and comorbid vocal fold paresis agreed to have a LEMG study resulting in a higher incidence of vocal cord paresis in our study. Our results suggest that further study of vocal fold paresis and its association with vocal fold polyps is essential.
Patients with vocal fold paresis may generate asymmetrical excessive muscular forces to achieve glottal closure which may lead to trauma to the vocal folds. This may be a contributing factor for polyp development in some patients with vocal fold paresis, or for recurrence of the lesion after excision. It has been stated that underlying “hypofunctional” glottal disorder sometimes demonstrates as “hyperfunctional” compensation [11, 17]. Thus, LEMG is an essential procedure to test neuromuscular integrity in these patients. Koufman and Belafsky [24] proposed that midfold localized Reinke’s edema or pseudocysts are a consequence of underlying paresis. Increased sheering trauma from effortful glottic closure is their hypothesized mechanism responsible for these lesions. It should be kept in mind that patients with voice disorders often have more than one underlying disorder, and each problem should be identified and corrected for a better voice outcome [11, 25].
Laryngopharyngeal reflux has been reported to be associated with vocal fold polyps as a causative factor [3, 6]. In our study RSI was found to be lower in the patients with vocal fold paresis than the patients with normal LEMG. It was reported that there is a slight predominance of vocal fold polyps in women [5]. Contrarily, we found that more men than women with vocal fold polyps accompanied vocal fold paresis in our study. These may suggest that clinicians should be more attentive to the possibility of coexisting vocal fold paresis with vocal fold polyps in men and in patients who have few symptoms for laryngopharyngeal reflux.
The neurolaryngeal examination of the larynx is performed best using transnasal fiberoptic laryngoscopy under continous light as subtleties can be observed easily. Presence of axial rotation, asymmetry in vocal cord longitudinal stretch, hypomobility, fatigue or bowing of vocal fold, and asymmetry of vertical height of vocal folds are findings that support the clinical suspicion of vocal fold paresis [12, 17, 25]. Our study also confirms that these laryngoscopic findings are observed significantly more in vocal fold polyp patients with vocal fold paresis than in vocal fold polyp patients with normal LEMG (p < 0.05). More than 70 % of the vocal fold polyp patients with LEMG-confirmed paresis revealed at least one of these fiberoptic examination findings in our study.
Another laryngeal finding which may suggest clinical suspicion of vocal fold paresis is supraglottic hyperfunction, such as medial–lateral compression of false vocal folds or supraglottic anterior–posterior approximation. These supraglottic hyperfunction patterns may result from an attempt to compensate the underlying glottal insufficiency [11, 25, 26]. But the presence of a vocal fold polyp complicates the situation as benign vocal fold lesions usually exhibit some supraglottic hyperfunction [27]. In our study, patients with vocal fold paresis and with normal LEMG did not reveal any difference in medial–lateral compression of false vocal folds or in anterior–posterior approximation. It thus can be concluded that supraglottic hyperfunction may not help to differentiate the presence of vocal fold paresis in vocal fold polyp patients. In fact, approximately 30 % (5/17) of the patients with LEMG-confirmed paresis exhibited only supraglottic hyperfunction during their fiberoptic examination.
In the setting of no readily apparent differences in vocal fold mobility, it can be difficult to recognize vocal fold paresis. Asymmetry of vibration, and incomplete glottal closure during laryngostroboscopic examination were reported to be associated with vocal fold paresis in this situation [9, 14]. But the presence of vibratory asymmetry is a common finding in patients with a vocal fold polyp [4, 28]. In our study vocal fold polyp patients with paresis and with normal LEMG showed a similar distribution of stroboscopic findings including vibratory characteristics and glottal closure pattern (p > 0.05). Our study suggests that laryngostroboscopic examination does not help to identify paresis in vocal fold polyp patients.
One of the limitations of our study is small sample size. Further study including more patients would be worthwhile to support our results. Second, the LEMGs and laryngoscopic examinations in our study were performed by the same neurologist and the same otolaryngologist. As both interpretation of LEMG findings and evaluation of laryngoscopic examinations are subjective in nature, having additional reviewers would have strengthened our study. To overcome the subjectivity problem in LEMG, another alternative would have been using a quantitative LEMG analysis [29]. Finally, it should be kept in mind that vocal fold paresis is not a single clinical condition but is more like different conditions lying along a spectrum, depending on the laryngeal nerve or nerves involved and the degree of the neuromuscular deficit. As a result, laryngoscopic examination findings can be expected to occur in a spectrum as well. This was not taken into account in our study when comparing examination findings. The evaluation of different subgroups of paresis could be the subject of future studies.
Conclusion
When dealing with patients who have been diagnosed with a vocal fold polyp, the possibility of coexisting vocal fold paresis should be kept in mind. LEMG confirmed the diagnosis of unilateral or bilateral vocal fold paresis in almost half of the patients with a vocal fold polyp. Vocal fold paresis accompanied vocal fold polyp more in men and in patients with few symptoms of laryngopharyngeal reflux. More than 70 % of the vocal fold polyp patients with LEMG-confirmed paresis had at least one of the transnasal fiberoptic examination findings, i.e., the presence of axial rotation, asymmetry in vocal cord longitudinal stretch, hypomobility, fatigue or bowing of vocal fold, and asymmetry of vertical height of vocal folds. Supraglottic hyperfunction did not help to differentiate the presence of vocal fold paresis in vocal fold polyp patients. Stroboscopic examination was not useful to identify paresis in vocal fold polyp patients.
It should be emphasized that vocal fold paresis can only be accurately diagnosed with LEMG even when laryngoscopic examination suggests the presence of it. Further research is needed to clarify the relationship between vocal fold paresis and vocal fold polyps and to determine the clinical significance of LEMG in patients with vocal fold polyps.
References
Dikkers FG, Nikkels PGJ (1995) Benign lesions of the vocal folds: histopathology and phonotrauma. Ann Otol Rhinol Laryngol 104:698–703
Marcotullio D, Magliulo G, Pietrunti S, Suriano M (2002) Exudative laryngeal diseases of Reinke’s space: a clinicohistopathological framing. J Otolaryngol 31:376–380
Koufman JA, Amin MR, Panetti M (2000) Prevalence of reflux in 113 consecutive patients with laryngeal and voice disorders. Otolaryngol Head Neck Surg 123:385–388
Johns MM (2003) Update on the etiology, diagnosis, and treatment of vocal fold nodules, polyps, and cysts. Curr Opin Otolaryngol Head Neck Surg 11:456–461
Martins RH, Defaveri J, Domingues MA, de Albuquerque e Silva R (2011) Vocal polyps: clinical, morphological, and immunohistochemical aspects. J Voice 25(1):98–106
Chung JH, Tae K, Lee YS, Jeong JH, Cho SH, Kim KR, Park CW, Han DS (2009) The significance of laryngopharyngeal reflux in benign vocal mucosal lesions. Otolaryngol Head Neck Surg 141(3):369–373
Sulica L, Blitzer A (2007) Vocal fold paresis: evidence and controversies. Curr Opin Otolaryngol Head Neck Surg 15:159–162
Merati AL, Shemirami N, Smith TL, Toohill RJ (2006) Changing trends in the nature of vocal fold motion impairment. Am J Otolaryngol 27:106–108
Simpson CB, May LS, Green JK, Eller RL, Jackson CE (2011) Vibratory asymmetry in mobile vocal folds: is it predictive of vocal fold paresis? Ann Otol Rhinol Laryngol 120:239–242
Dursun G, Sataloff RT, Spiegel JR, Mandel S, Heuer RJ, Rosen DC (1996) Superior laryngeal nerve paresis and paralysis. J Voice 10:206–211
Koufman JA, Postma GN, Cummins MM, Blalock PD (2000) Vocal fold paresis. Otolaryngol Head Neck Surg 122:537–541
Heman-Ackah YD, Batory M (2003) Determining the etiology of mild vocal fold hypomobility. J Voice 17:579–588
Heman-Ackah YD, Barr A (2006) Mild vocal fold paresis: understanding clinical presentation and electromyographic findings. J Voice 20:269–281
Simpson CB, Cheung EJ, Jackson CJ (2009) Vocal fold paresis: clinical and electrophysiologic features in a tertiary laryngology practice. J Voice 23:396–398
Bach KK, Belafsky PC, Wasylik K, Postma GN, Koufman JA (2005) Validity and reliability of the Glottal Function Index. Arch Otolaryngol Head Neck Surg 131(11):961–964
Belafsky PC, Postma GN, Koufman JA (2001) Validity and reliability of the Reflux Symptom Index (RSI). Laryngoscope 111:1313–1317
Rubin AD, Praneetvatakul V, Heman-Ackah Y, Moyer CA, Mandel S, Sataloff RT (2005) Repetitive phonatory tasks for identifying vocal fold paresis. J Voice 19:679–686
Hirano M, Bless DM (1993) Videostroboscopic examination of the larynx. Singular Publishing, San Diego
Koufman JA, Walker FO (1998) Laryngeal electromyography in clinical practice: indications, techniques, and interpretation. Phonoscope 1:57–70
Sataloff RT, Mandel S, Manon-Espaillat R, Heman-Ackah YD, Abaza M (2003) Basic aspects of the electrodiagnostic evaluation. In: Sataloff RT, Korovin GS (eds) Laryngeal electromyography. Delmar Learning, Clifton Park, pp 8–58
Sataloff RT, Mandel S, Manon-Espaillat R, Heman-Ackah YD, Abaza M (2003) Laryngeal electromyography. In: Sataloff RT, Korovin GS (eds) Laryngeal electromyography. Delmar Learning, Clifton Park, pp 59–85
Yin SS, Qiu WW, Stucker FJ (1997) Major patterns of laryngeal electromyography and their clinical application. Laryngoscope 107:126–136
Koufman JA, Postma GN, Whang CS, Rees CJ, Amin MR, Belafsky PC, Johnson PE, Connolly KM, Walker FO (2001) Diagnostic laryngeal electromyography: the Wake Forest experience 1995–1999. Otolaryngol Head Neck Surg 124(6):603–606
Koufman JA, Belafsky PC (2001) Unilateral or localized Reinke’s edema (pseudocyst) as a manifestation of vocal cord paresis: the paresis podule. Laryngoscope 111:576–580
Altman KW (2005) Laryngeal asymmetry on indirect laryngoscopy in a asymptomatic patient should be evaluated with electromyography. Arch Otolaryngol Head Neck Surg 131(4):356–359
Belafsky PC, Postma GN, Reulbach TR, Holland BW, Koufman JA (2002) Muscle tension dysphonia as a sign of underlying glottal insufficiency. Otolaryngol Head Neck Surg 127(5):448–451
Altman KW, Atkinson C, Lazarus C (2005) Current and emerging concepts in muscle tension dysphonia: a 30-month review. J Voice 19(2):261–267
Colton RH, Woo P, Brewer DW, Griffin B, Casper J (1995) Stroboscopic signs associated with benign lesions of the vocal folds. J Voice 9(3):312–325
Statham MM, Rosen CA, Nandedkar SD, Munin MC (2010) Quantitative laryngeal electromyography: turns and amplitude analysis. Laryngoscope 120(10):2036–2041
Acknowledgments
The authors wish to thank Daniel B. Magraw from Johns Hopkins University for editorial assistance in the preparation of this manuscript.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akbulut, S., Inan, R.A., Altintas, H. et al. Vocal fold paresis accompanying vocal fold polyps. Eur Arch Otorhinolaryngol 272, 149–157 (2015). https://doi.org/10.1007/s00405-014-3227-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3227-8