Abstract
Azelastine was suggested as a supplementary choice of glucocorticoid for the control of moderate to severe allergic rhinitis (AR). However, the underlying mechanism has not been completely understood. In this study, primary cultured nasal epithelial cells and bronchial epithelial cells were stimulated with proinflammatory cytokines (IL-1β and IL-17A) and anti-inflammatory agents (azelastine and budesonide) in vitro. The expression of intercellular adhesion molecule 1 (ICAM-1) and mitogen-activated protein kinase phosphatase-1 (MKP-1) was examined using qPCR and ELISA, respectively. Moreover, the additive effects of azelastine and budesonide nasal spray on nasal ICAM-1 level and total nasal symptom scores were evaluated in six uncontrolled severe AR patients by budesonide nasal spray alone. We found azelastine significantly inhibited cytokine-induced ICAM-1 upregulation, which is reversed by MKP-1 silencing. Azelastine and budesonide additively increased MKP-1 expression and inhibited ICAM-1 expression in vitro. After treatment for two consecutive weeks, combined azelastine and budesonide nasal spray significantly decreased nasal ICAM-1 level and TNSS in six uncontrolled AR patients. Our findings suggested that azelastine is able to additively enhance the anti-inflammatory effect of budesonide by modulating MKP-1 expression, which may implicate in the treatment of uncontrolled severe AR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Allergic rhinitis (AR) is a very common disorder that is characterized by Th2-skewed eosinophilic inflammation and elevated levels of pro-inflammatory cytokines [1]. Currently, the recommended first-line treatment of AR patients with moderate to severe symptoms is use of nasal glucocorticoid and/or oral antihistamine which has been demonstrated to efficiently improve all nasal symptoms [2]. Despite optimal pharmacotherapy, it has been demonstrated that not all patients with moderate/severe AR are well controlled [1, 3]. Azelastine is a second-generation antihistamine which is topically administrated for AR patients to obtain higher local distribution. Compared with oral antihistamine treatments, a higher concentration of azelastine can enhance its anti-allergic and anti-inflammatory effects [4]. Recent studies have indicated that combined azelastine and glucocorticoid nasal spray may provide a substantial therapeutic benefit for seasonal AR patients [5, 6]. However, the underlying mechanism has not been well understood.
The inflammatory response in the nasal mucosa includes an immediate IgE-mediated mast cell response as well as a late phase response characterized by recruitment of eosinophils and on-going allergic inflammation. Induction of intercellular adhesion molecule 1 (ICAM-1) and subsequent migration of inflammatory cells such as eosinophils and neutrophils represented one critical step in the pathogenesis of AR [7]. Therefore, nasal ICAM-1 may be considered as the critical therapeutic target of AR patients [8]. To evaluate the additive effects of antihistamine and glucocorticoid on allergic response in AR patients, we examined the regulatory effects of azelastine and budesonide on ICAM-1 expression in cultured epithelial cells and uncontrolled severe AR patients. Moreover, mitogen-activated protein kinase phosphatase-1 (MKP-1), a glucocorticoid-inducible anti-inflammatory gene [9], was examined in cultured epithelial cells in the presence of proinflammatory cytokines, azelastine and budesonide.
Materials and methods
Subjects
This study was approved by the local ethical committee, and written informed consent was obtained from all the subjects. Fifteen moderate to severe adult patients with AR [visual analogue score (VAS) >3] which accorded with the standard criterion for AR issued by ARIA guideline were recruited in the study [1]. Eleven non-atopic patients undergoing septoplasty because of anatomical variations were considered as controls. The atopic status of the patients and control subjects was evaluated by allergen skin prick tests. None of the subjects used oral or nasal corticosteroids 4 weeks before sampling. All subjects were non-smokers and free from upper respiratory tract infection for 4 weeks preceding the study. The demographic data from the patients and normal controls enrolled in this study were listed in Table 1. For cell culture and histological analysis, nasal specimens were obtained from the anterior part of inferior turbinate under local anesthesia. Nasal specimen was fixed for immunohistochemical (IHC) staining and/or cell isolation and culture.
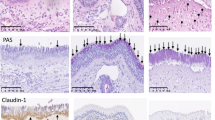
IHC staining
Nasal biopsies were collected from 15 AR patients and 11 normal controls as mentioned above. IHC staining was performed using the Envision method. A mouse anti-human ICAM-1 monoclonal antibody (Abcam, Cambridge, MA, USA) was used at a dilution of 1:100 according to the manufacturer’s instructions. The histological analyzes were performed by two blinded investigators who were aware of the clinical data. The staining intensities of 10 randomly selected areas (400×) on each section of the subjects were summed and averaged. The staining intensity of ICAM-1 was semiquantitatively scored as follows: none, 0; weak, 1; moderate, 2; strong, 3.
Cell culture and stimulation
For in vitro cell culture, primary NECs were randomly collected from four AR patients by means of enzymatic digestion. Collected NECs, as well as BECs (Lonza, Walkersville, MD, USA), were cultured in submersion cultures in BEGM medium (Lonza) until passaged. When 80–90 % confluence was reached, the epithelial cells were washed with PBS (37 °C, pH 7.4), and fresh media without hydrocortisone was added in the presence of different stimulators or PBS (control) for 0–24 h. These stimulators included recombinant cytokines such as human IL-1β (10 ng/mL), IL-17A (10 ng/mL) (all were purchased from R&D systems, Minneapolis, MN, USA), azelastine (0.1–1 %) and budesonide (10−7–10−5 M) (all were purchased from Sigma-aldrich, St. Louis, MO, USA). For RNA interference, MKP-1 siRNA (50 nmol/L) (Shanghai Genepharma Co., Ltd. Shanghai, China) was transfected into BECs with Lipofectamine 2000 reagent (Invitrogen, Rockville, MD, USA) according to the manufacturer’s protocol. After then, cell pellets and supernatants were collected for qPCR and ELISA, respectively.
qPCR
qPCR was performed as we previously reported [10]. The sequences of the primer were as follows: ICAM-1 forward: 5′-GCA AGA AGA TAG CCA ACC AAT G-3′; reverse: 5′-TGC CAG TTC CAC CCG TTC-3′; MKP-1 forward: 5′-CGA GGC CAT TGA CTT CAT AGA-3′; reverse: 5′-TCA TAA GGT AAG CAA GGC AGA T-3′; GAPDH forward: 5′-GAA GGT GAA GGT CGG AGT-3′; GAPDH reverse: 5′-GAA GAT GGT GAT GGG ATT TC-3′. All PCR reactions were performed in duplicate. Melting curve analysis was used to control for amplification specificity. Expression of target gene was expressed as fold increase or decrease relative to the expression of GAPDH, The mean value of the replicates for each sample was calculated and expressed as cycle threshold (C t). The amount of gene expression was then calculated as the difference (ΔC t) between the C t value of target gene and the C t value of GAPDH. Fold changes in target gene mRNA were determined as \( 2^{{ - \Delta \Delta C_{\text{t}} }} \).
ELISA
The levels of soluble ICAM-1 in the nasal secretions and supernatants of cultured epithelial cells were measured using ELISA. Commercially available ELISA kit of soluble ICAM-1 (R&D Systems, Minneapolis, MN) was used according to the manufacturer’s protocols. The detection limit for soluble ICAM-1 was 256 pg/mL. For convenient analysis, all values below the detectable limit were considered to be zero.
Nasal ICAM-1 examination
Six uncontrolled severe AR patients (VAS ≥5) after persistent administration of budesonide nasal spray (Rhinocort Aqua; AstraZeneca, Lund, Sweden) were specifically recruited after signing the written informed consent form. They were administrated with combined budesonide (Rhinocort Aqua) and azelastine nasal spray (Azep, MEDA Pharma GmbH & Co. Bad Homburg, Germany) for two consecutive weeks. The total nasal symptom scores (TNSS) were evaluated by VAS scale before and after treatment. The nasal secretions were collected before and after treatment as we described elsewhere [11], and the nasal ICAM-1 expression was determined by ELISA.
Statistical analysis
For in vitro experiment, data were expressed as mean and the standard error of the mean (SEM), and were analyzed with one-way ANOVA and the paired Student’s t test. For tissue examination, data were expressed as the median and interquartile range (IQR), and were analyzed via nonparametric Mann–Whitney U test. A p value of less than 0.05 was considered statistically significant.
Results
Increased ICAM-1 expression in AR patients is associated with disease severity
To investigate the importance of ICAM-1 expression in AR patients, we firstly examined the immunoreactivity of ICAM-1 in AR and normal controls. As showed in Fig. 1, we found ICAM-1 was extensively distributed in nasal mucosa of AR patients. The intensity of ICAM-1 expression in AR patients was significantly upregulated compared to the normal controls (p < 0.05). Moreover, when correlated the immunoreactivity of ICAM-1 with the VAS score, we found the intensity of ICAM-1 expression in AR patients was significantly associated with disease severity (p < 0.05).
The expression of ICAM-1 in AR patients and normal controls. a Representative IHC staining of ICAM-1 was shown (×200); b intensity of ICAM-1 in nasal mucosa of AR patients was significantly increased compared to that in normal controls; c intensity of ICAM-1 in nasal mucosa of AR patients was significantly associated with disease severity. The data indicated the median (IQR) of AR patients and normal controls
Proinflammatory cytokines and azelastine inhibited ICAM-1 expression in vitro
To determine the effects of proinflammatory cytokines on ICAM-1 expression, we firstly examined the mRNA and protein expression of ICAM-1 in response to IL-1β (10 ng/mL) and IL-17A (10 ng/mL) in primary cultured NECs. As showed in Fig. 2a, b, we found both IL-1β and IL-17A significantly increased mRNA and protein expression of ICAM-1 in primary cultured NECs (p < 0.01). Next, we tested the effects of azelastine (0.1 %) on cytokine-induced ICAM-1 upregulation in primary cultured NECs. Consequently, we found azelastine significantly inhibited cytokine-induced ICAM-1 mRNA and protein expression in primary cultured NECs (p < 0.01) (Fig. 2c, d).
The mRNA and protein expression of ICAM-1 in cultured NECs. Proinflammatory cytokines IL-1β (10 ng/mL) and IL-17A (10 ng/mL) significantly increased mRNA and protein expression of ICAM-1 in primary cultured NECs (a, b), which can be significantly inhibited by azelastine (0.1 %) (c, d). The mRNA and protein levels of ICAM-1 were determined by qPCR (6 h) and ELISA (24 h), respectively. The data indicated the means (SEM) of three independent experiments
MKP-1is required for Azelastine inhibited- ICAM-1 expression in vitro
To further evaluate the possible mechanism underlying ICAM-1 inhibition in azelastine-treated airway epithelial cells, we then examined MKP-1 mRNA expression in cultured NECs and BECs in response to cytokine and azelastine administration. When adding cytokine alone, we found neither IL-1β nor IL-17A significantly changed MKP-1 mRNA expression in cultured NECs and BECs (data not shown). In the presence of IL-1β or IL-17A, we found azelastine significantly increased MKP-1 mRNA expression in cultured NECs and BECs, in a dose-dependent manner (p < 0.01) (Fig. 3a, b). Conversely, when adding siRNA to specifically knock down MKP-1 expression (nearly 65 % knockdown of MKP-1 expression comparing to mock control, data not shown), we found added MKP-1 siRNA significantly abolished azelastine inhibition on ICAM-1 mRNA expression in cultured BECs (p < 0.01) (Fig. 2c). These findings suggested azelastine modulates ICAM-1 expression in epithelial cells through a MKP-1-dependent manner.
The mRNA expression of MKP-1 in cultured NECs and BECs. In the presence of IL-1β (10 ng/mL) and IL-17A(10 ng/mL), azelastine significantly increased MKP-1 mRNA expression in cultured NECs and BECs in a dose-dependent manner (a, b), and silencing MKP-1 with siRNA significantly abolished azelastine inhibition on ICAM-1 mRNA expression in cultured BECs (c, d). The mRNA level of ICAM-1 was determined by qPCR (6 h). The data indicated the means (SEM) of three independent experiments
Azelastine and budesonide synergistically modulated MKP-1-mediated ICAM-1 expression in vitro
To comparably evaluate the effects of glucocorticoid on MKP-1-modulated ICAM-1 expression in airway epithelial cells, we then examined cytokine-induced MKP-1 and ICAM-1 expression in the presence of budesonide. Consequently, we found budesonide alone significantly increased MKP-1 mRNA expression and inhibited ICAM-1 mRNA expression in cultured NECs, in a dose-dependent manner (p < 0.01) (Fig. 4a, b). Both azelastine and budesonide significantly increased MKP-1 mRNA expression in cultured NECs in the presence of IL-1β (p < 0.01), but only azelastine significantly increased MKP-1 mRNA expression in cultured NECs (p < 0.01) in the presence of IL-17A (Fig. 4c, d). When adding two agents simultaneously, we found azelastine and budesonide additively increased MKP-1 mRNA expression in cultured NECs in the presence of IL-1β or IL-17A (Fig. 4c, d).
Synergistic effects of azelastine and budesonide on MKP-1 mRNA expression in cultured NECs. a, b Budesonide alone significantly increased MKP-1 mRNA expression and inhibited ICAM-1 mRNA expression in cultured NECs, in a dose-dependent manner; c, d in the presence of IL-1β and IL-17A, azelastine (0.1 %) and budesonide (10−7 M) Synergistically increased MKP-1 mRNA expression in cultured NECs. The mRNA level of MKP-1 was determined by qPCR (6 h). The data indicated the means (SEM) of three independent experiments
Azelastine and budesonide synergistically modulated MKP-1-mediated ICAM-1 expression in vitro
To further validate the in vitro data, we next examined ICAM-1 expression in AR patients and evaluated the additive effects of azelastine and budesonide on ICAM-1 expression and nasal symptom in six uncontrolled severe AR patients to budesonide nasal spray alone. The six AR patients were instructed to use combined azelastine and budesonide nasal spray for two consecutive weeks. Consequently, combined azelastine and budesonide nasal spray was found to significantly inhibit ICAM-1 expression in nasal mucosa of AR patients when compared to budesonide alone (baseline value) (p < 0.05) (Fig. 5a). Accordingly, combined azelastine and budesonide nasal spray significantly improved total nasal symptom scores compared to budesonide alone (baseline value) in 6 severe AR patients (p < 0.05) (Fig. 5b). These findings suggested azelastine is able to enhance anti-inflammatory activity of budesonide and improve nasal symptom in uncontrolled severe AR patients.
Synergistically effects of azelastine and budesonide nasal spray on nasal ICAM-1 expression and total nasal symptom scores in six severe AR patients after 2 weeks treatment. a Compared to budesonide alone, combined azelastine and budesonide nasal spray significantly inhibited ICAM-1 expression in nasal mucosa of AR patients; b accordingly, combined azelastine and budesonide nasal spray significantly improved total nasal symptom scores compared to baseline value (budesonide alone) in six severe AR patients. The data indicated the median (IQR) of six AR patients
Discussion
Although there are growing evidences suggest combined antihistamine and nasal glucocorticoid are more efficacious in the treatment of moderate to severe AR [1], the molecular mechanism underlying the add-on effect of antihistamine on glucocorticoid therapy has been largely unknown. In the present study, we provided the first evidence that azelastine, an antihistamine that administrated topically, is able to inhibit cytokine-induced ICAM-1 upregulation in a MKP-1-dependent manner in cultured epithelial cells. Moreover, azelastine is shown to enhance budesonide efficacy by means of MKP-1 induction and ICAM-1 suppression in vitro and ex vivo. These findings therefore, expand our understanding on the pathogenesis of AR and contribute to designing optimal therapeutical strategy.
Since increased ICAM-1 expression is responsible for the persistent cellular recruitment and inflammation, nasal ICAM-1 levels have been proposed as a hallmark for clinical severity and follow-up evaluation in AR patients [12]. For example, Gorska-Ciebiada et al. [13] reported the serum and nasal ICAM-1 levels were significantly lower in mild AR patients than in moderate to severe AR patients, demonstrating a correlation of ICAM-1 level and AR severity. Klaewsongkram et al. [14] showed nasal ICAM-1 expression significantly correlates with infiltration of eosinophils and neutrophils in nasal mucosa of AR patients. The expression of ICAM-1 in nasal mucosa as the hallmark of persistent inflammation has been well documented. Previous studies showed environmental stimulus (e.g., virus, allergen) and cytokines (e.g., IFN-γ, TNF-α) can increase ICAM-1 expression in AR patients [15]. In this study, we found the intensity of ICAM-1 expression in AR patients was significantly upregulated compared to the normal controls. Moreover, when correlated the immunoreactivity of ICAM-1 with the VAS score, we found the intensity of ICAM-1 expression in AR patients was significantly associated with disease severity, suggesting ICAM-1 may be regarded as the therapeutic target for the management of AR. Consistently, we found ICAM-1 expression was significantly increased in cultured epithelial cells in response to proinflammatory cytokines IL-1β and IL-17A. Moreover, we showed that azelastine is able to significantly inhibit ICAM-1 upregulation in vitro. Interestingly, we found the inhibition of ICAM-1 in epithelial cells is MKP-1-dependent by siRNA transfection. This finding provides us a novel pharmacological mechanism underlying the anti-inflammatory effect of azelastine.
MKP-1, an archetypical member of MAPK phosphatases family, functions as a vital negative regulator in the innate immune system. It localizes to the nucleus through its N terminus and preferentially dephosphorylates activated p38 and JNK relative to ERK in vitro [16]. Recently, Manetsch et al. found dexamethasone is able to activate MKP-1 transcription in airway smooth muscle cells via a cis-acting glucocorticoid-responsive region located between −1,380 and −1,266 bp of the MKP-1 promoter [17]. Additionally, dexamethasone exerted anti-inflammatory effects has been demonstrated to be through MKP-1-dependent mechanisms [18]. These findings suggested increased MKP-1 expression in response to azelastine may exert addictive effect of glucocorticoid by increasing the sensitivity of glucocorticoid in the treatment of uncontrolled severe AR patients.
Although current ARIA guidelines recommend the combination of antihistamine and nasal glucocorticoid for the treatment of AR, the efficacy of antihistamine and nasal glucocorticoid therapy remains controversial. Some studies failed to demonstrate significant improvement when using the combination of fluticasone with cetirizine and mometasone with deloratadine [19–22]. In contrast to oral antihistamine, nasal antihistamine therapy represents an effective mode of drug delivery in AR and non-AR patients and its effect has been shown on many mediators (e.g., histamines, cytokines, chemokines and eosinophils) at clinically relevant concentrations [4]. Previously, azelastine nasal spray is found to be effective to patients with seasonal AR who do not respond to oral antihistamine. For example, LaForce et al. [23] showed azelastine nasal spray is effective monotherapy for seasonal AR patients who remain symptomatic after treatment with fexofenadine. Unlike to oral antihistamine, azelastine nasal spray and fluticasone nasal spray in combination may provide a substantial therapeutic benefit for patients with seasonal AR compared with therapy with either agent alone [5, 6, 24].
Based on our findings, we postulated this local delivery with its unique pharmacologic profile of adding MKP-1 expression may be the reason that azelastine is so effective at relieving symptoms of AR. To test our hypothesis, we comparably evaluate the effects of azelastine and glucocorticoid on MKP-1-modulated ICAM-1 expression in cultured airway epithelial cells. As expected, we found both azelastine and budesonide significantly increased MKP-1 mRNA expression in cultured NECs in the presence of IL-1β. However, in the presence of IL-17A, azelastine but not budesonide significantly increased MKP-1 mRNA expression in cultured NECs. The relative insensitivity of budesonide to IL-17A-induced inflammation may be ascribed to the property of IL-17A on glucocorticoid-mediated signaling pathway. For example, McKinley et al. [25] demonstrated that Th17 cell-mediated airway inflammation and airway hyperresponsiveness are steroid resistant in asthmatic mice model, indicating a potential role for Th17 cells in steroid-resistant asthma. In addition, our group and Vazquez-Tello et al. [26] showed Th17 cells are able to induce glucocorticoid receptor-β expression in epithelial cells of AR and asthma [10], which may account for the relative insensitivity of glucocorticoid in uncontrolled AR.
Several factors are proposed to be responsible for the severe AR patients who do not respond well to medication. Of them, inadequate medication and relative insensitivity of glucocorticoid may be the major reasons for lack of control in some severe AR patients [3]. Previously, we have shown IL-17A level is associated with AR severity and relative glucocorticoid insensitivity [10]. Considering IL-17A is able to affect clinical efficacy of glucocorticoid, more efficacious therapies for the management of AR are thus required. In this study, the interesting finding is that azelastine and budesonide can synergistically increase MKP-1 mRNA expression in the presence of IL-17A in vitro, which may implicate in the treatment of severe AR who didn’t respond well to glucocorticoid. To further validate the synergistic effects of azelastine and budesonide ex vivo, we specifically enrolled six uncontrolled severe AR patients to budesonide nasal spray alone. As a result, we found combined azelastine and budesonide nasal spray significantly inhibited ICAM-1 expression, as well as TNSS compared to budesonide alone (baseline value). Our study is thus very important for we can observe synergistic effects of azelastine and budesonide in the presence of IL-17A, which may be helpful to improve the clinical efficacy of uncontrolled severe AR.
Conclusion
Our findings suggested that azelastine is able to additively enhance the anti-inflammatory effect of glucocorticoid by modulating MKP-1 expression, which may implicate in the treatment of uncontrolled severe AR.
References
Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, Zuberbier T, Baena-Cagnani CE, Canonica GW, van Weel C, Agache I, Aït-Khaled N, Bachert C, Blaiss MS, Bonini S, Boulet LP, Bousquet PJ, Camargos P, Carlsen KH, Chen Y, Custovic A, Dahl R, Demoly P, Douagui H, Durham SR, van Wijk RG, Kalayci O, Kaliner MA, Kim YY, Kowalski ML, Kuna P, Le LT, Lemiere C, Li J, Lockey RF, Mavale-Manuel S, Meltzer EO, Mohammad Y, Mullol J, Naclerio R, O’Hehir RE, Ohta K, Ouedraogo S, Palkonen S, Papadopoulos N, Passalacqua G, Pawankar R, Popov TA, Rabe KF, Rosado-Pinto J, Scadding GK, Simons FE, Toskala E, Valovirta E, van Cauwenberge P, Wang DY, Wickman M, Yawn BP, Yorgancioglu A, Yusuf OM, Zar H, Annesi-Maesano I, Bateman ED, Ben Kheder A, Boakye DA, Bouchard J, Burney P, Busse WW, Chan-Yeung M, Chavannes NH, Chuchalin A, Dolen WK, Emuzyte R, Grouse L, Humbert M, Jackson C, Johnston SL, Keith PK, Kemp JP, Klossek JM, Larenas-Linnemann D, Lipworth B, Malo JL, Marshall GD, Naspitz C, Nekam K, Niggemann B, Nizankowska-Mogilnicka E, Okamoto Y, Orru MP, Potter P, Price D, Stoloff SW, Vandenplas O, Viegi G, Williams D, World Health Organization, GA(2)LEN, AllerGen (2008) Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy 63(Suppl 86):8–160
Greiner AN, Hellings PW, Rotiroti G, Scadding GK (2011) Allergic rhinitis. Lancet 378:2112–2122
Hellings PW, Fokkens WJ, Akdis C, Bachert C, Cingi C, Dietz de Loos D, Gevaert P, Hox V, Kalogjera L, Lund V, Mullol J, Papadopoulos NG, Passalacqua G, Rondón C, Scadding G, Timmermans M, Toskala E, Zhang N, Bousquet J (2013) Uncontrolled allergic rhinitis and chronic rhinosinusitis: where do we stand today? Allergy 68:1–7
Hernandez-Trujillo V (2009) Antihistamines treatment for allergic rhinitis: different routes, different mechanisms? Allergy Asthma Proc 30:584–588
Carr W, Bernstein J, Lieberman P, Meltzer E, Bachert C, Price D, Munzel U, Bousquet J (2012) A novel intranasal therapy of azelastine with fluticasone for the treatment of allergic rhinitis. J Allergy Clin Immunol 129:1282–1289
Ratner PH, Hampel F, Van Bavel J, Amar NJ, Daftary P, Wheeler W, Sacks H (2008) Combination therapy with azelastine hydrochloride nasal spray and fluticasone propionate nasal spray in the treatment of patients with seasonal allergic rhinitis. Ann Allergy Asthma Immunol 100:74–81
Rosenwasser LJ (2011) Current understanding of the pathophysiology of allergic rhinitis. Immunol Allergy Clin North Am 31:433–439
Ciebiada M, Barylski M, Gorska Ciebiada M (2013) Nasal eosinophilia and serum soluble intercellular adhesion molecule 1 in patients with allergic rhinitis treated with montelukast alone or in combination with desloratadine or levocetirizine. Am J Rhinol Allergy 27:e58–e62
Wang X, Liu Y (2007) Regulation of innate immune response by MAP kinase phosphatase-1. Cell Signal 19:1372–1382
Tang H, Wang H, Bai J, Ding M, Liu W, Xia W, Luo Q, Xu G, Li H, Fang J (2012) Sensitivity of MUC5AC to topical corticosteroid is negatively associated with interleukin-17A in patients with allergic rhinitis. Am J Rhinol Allergy 26:359–364
Luo Q, Chen F, Liu W, Li Z, Xu R, Fan Y, Chen R, Xu Y, Liu Z, Xu G, Fu Q, Zuo K, Shi J, Li H (2011) Evaluation of long-term clarithromycin treatment in adult Chinese Patients with chronic rhinosinusitis without nasal polyps. ORL J Otorhinolaryngol Relat Spec 73:206–211
Matsui T, Asakura K, Shirasaki H, Kataura A, Himi T (2000) Relationship between infiltrating cells and adhesion molecules in the nasal mucosa of patients with allergic rhinitis. Acta Otolaryngol 120:973–980
Gorska-Ciebiada M, Ciebiada M, Gorska MM, Gorski P, Grzelewska-Rzymowska I (2006) Intercellular adhesion molecule 1 and tumor necrosis factor alpha in asthma and persistent allergic rhinitis: relationship with disease severity. Ann Allergy Asthma Immunol 97:66–72
Klaewsongkram J, Ruxrungtham K, Wannakrairot P, Ruangvejvorachai P, Phanupak P (2003) Eosinophil count in nasal mucosa is more suitable than the number of ICAM-1-positive nasal epithelial cells to evaluate the severity of house dust mite-sensitive allergic rhinitis: a clinical correlation study. Int Arch Allergy Immunol 132:68–75
Canonica GW, Compalati E (2009) Minimal persistent inflammation in allergic rhinitis: implications for current treatment strategies. Clin Exp Immunol 158:260–271
Wancket LM, Frazier WJ, Liu Y (2012) Mitogen-activated protein kinase phosphatase (MKP)-1 in immunology, physiology, and disease. Life Sci 90:237–248
Quante T, Ng YC, Ramsay EE, Henness S, Allen JC, Parmentier J, Ge Q, Ammit AJ (2008) Corticosteroids reduce IL-6 in ASM cells via up-regulation of MKP-1. Am J Respir Cell Mol Biol 39:208–217
Wang X, Nelin LD, Kuhlman JR, Meng X, Welty SE, Liu Y (2008) The role of MAP kinase phosphatase-1 in the protective mechanism of dexamethasone against endotoxemia. Life Sci 83:671–680
Anolik R, Mometasone Furoate Nasal Spray With Loratadine Study Group (2008) Clinical benefits of combination treatment with mometasone furoate nasal spray and loratadine vs monotherapy with mometasone furoate in the treatment of seasonal allergic rhinitis. Ann Allergy Asthma Immunol 100:264–271
Di Lorenzo G, Pacor ML, Pellitteri ME, Morici G, Di Gregoli A, Lo Bianco C, Ditta V, Martinelli N, Candore G, Mansueto P, Rini GB, Corrocher R, Caruso C (2004) Randomized placebo-controlled trial comparing fluticasone aqueous nasal spray in mono-therapy, fluticasone plus cetirizine, fluticasone plus montelukast and cetirizine plus montelukast for seasonal allergic rhinitis. Clin Exp Allergy 34:259–267
Pinar E, Eryigit O, Oncel S, Calli C, Yilmaz O, Yuksel H (2008) Efficacy of nasal corticosteroids alone or combined with antihistamines or montelukast in treatment of allergic rhinitis. Auris Nasus Larynx 35:61–66
Barnes ML, Ward JH, Fardon TC, Lipworth BJ (2006) Effects of levocetirizine as add-on therapy to fluticasone in seasonal allergic rhinitis. Clin Exp Allergy 36:676–684
LaForce CF, Corren J, Wheeler WJ, Berger WE, Rhinitis Study Group (2004) Efficacy of azelastine nasal spray in seasonal allergic rhinitis patients who remain symptomatic after treatment with fexofenadine. Ann Allergy Asthma Immunol 93:154–159
Meltzer EO, LaForce C, Ratner P, Price D, Ginsberg D, Carr W (2012) MP29-02 (a novel intranasal formulation of azelastine hydrochloride and fluticasone propionate) in the treatment of seasonal allergic rhinitis: a randomized, double-blind, placebo-controlled trial of efficacy and safety. Allergy Asthma Proc 33:324–332
McKinley L, Alcorn JF, Peterson A, Dupont RB, Kapadia S, Logar A, Henry A, Irvin CG, Piganelli JD, Ray A, Kolls JK (2008) TH17 cells mediate steroid-resistant airway inflammation and airway hyperresponsiveness in mice. J Immunol 181:4089–4097
Vazquez-Tello A, Semlali A, Chakir J, Martin JG, Leung DY, Eidelman DH, Hamid Q (2010) Induction of glucocorticoid receptor-beta expression in epithelial cells of asthmatic airways by T-helper type 17 cytokines. Clin Exp Allergy 40:1312–1322
Acknowledgments
This study was supported by the National Natural Science Fund of China (No. 81260156, 81271054, 81371071) and grants from the Ministry of Hygiene (No. 201202005, 2014BAI07B04).
Conflict of interest
No conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding authors
Additional information
X. Luo and R. Ma have contributed equally to this study.
Rights and permissions
About this article
Cite this article
Luo, X., Ma, R., Wu, X. et al. Azelastine enhances the clinical efficacy of glucocorticoid by modulating MKP-1 expression in allergic rhinitis. Eur Arch Otorhinolaryngol 272, 1165–1173 (2015). https://doi.org/10.1007/s00405-014-3191-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3191-3