Abstract
Recently, a new acoustic device, the so-called Sophono Alpha System, has been introduced into clinical practice. The aim of this study was to assess Sophono Alpha System hearing aids in ten patients suffering from recurrent chronic middle ear disease who underwent subtotal petrosectomy. Presence of mixed hearing loss with bone conduction thresholds better than or equal to 45 dB was present in each patient. Audiometric tests were performed before and after Sophono implantation and using a conventional bone conduction hearing aid (hearing glasses). Speech audiometry data (speech recognition threshold and word recognition score) were also collected. Speech recognition threshold in dB and percentage of word recognition score at 65 dB were subsequently calculated. After implantation and activation of the Sophono Alpha System, audiological data showed an average air conduction value of 42.1 dB. By comparing this data with the values of air conduction following subtotal petrosectomy, an average acoustic improvement of 29.7 dB could be calculated. The hearing results showed significantly better outcomes of Sophono Alpha System vs. conventional bone conduction aid. Indications to MRI use in patients undergoing Sophono Alpha System implantation are also provided.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, a new acoustic device, the so-called Sophono Alpha system (SAS), has been introduced into clinical practice [1, 2]. This is a bone-conduction system, implanted transcutaneously, devised for restoring conductive or mixed hearing loss with bone conduction thresholds better than or equal to 45 dB [1–3]. It consists of a behind-the-ear external digital audio processor and a subcutaneous magnetic implant, screwed to the skull [1, 2]. The SAS was first implanted in 2010 and since then it has been adopted in a series of over 100 patients [4].
To our knowledge, no investigation has been reported regarding its use in patients submitted to subtotal petrosectomy (SP). As is well known, this surgical technique induces a postoperative conductive hearing loss up to 50 or 60 dB [5]. SAS may be an optimal alternative to conventional bone conductive hearing aids and to the most widely used bone-anchored hearing aid system BAHA, in order to restore adequate hearing [6].
The aim of this study was to assess SAS hearing aids in patients suffering from recurrent chronic middle ear disease who had undergone SP. Its results in terms of hearing have been compared with those obtained using conventional hearing aids. Information about general, social and physical patient benefits after SAS implantation were carefully investigated using the validated Glasgow Benefit Inventory (GBI) [7, 8].
Materials and methods
This study comprises ten patients (3 men and 7 women; mean age 47.8 years; range 16–67; right ear and left ear equally affected) who had undergone subtotal petrosectomy (SP). As known, the SP technique requires the blind sac closure of the external auditory canal, obliteration of the eustachian tube with bone wax reinforced by a small piece of temporal muscle plus fibrin glue and the complete exenteration of all air cell tracts towards the otic capsule. Finally, the middle ear space is obliterated with abdominal fat and closed with a periosteal flap, thus completing the procedure while leaving cochlear and vestibular functions intact [5]. Whereas the indications for its use are more straightforward in an ear with unserviceable hearing, it does not represent the first option for the surgical treatment of chronic otitis media [5, 9, 10]. However, it is occasionally required in an ear with a good cochlear reserve due to the severity and recurrence of middle ear disease [10]. In our center, per year only 3.26 % of the patients with chronic otitis media underwent SP.
Table 1 gives an overview of patients’ characteristics in terms of etiology of the disease, indications for performing the SP and the history of traditional hearing aid use. Eight patients were affected by recurrent chronic otitis media. Cholesteatoma was diagnosed in only one patient. Finally, the last patient suffered from temporal bone encephalocele (Fig. 1) and had been unsuccessfully operated on in another hospital. We decided to perform subtotal petrosectomy as a first choice of treatment for the high risk of recurrent meningitis since the patient had presented a previous episode of meningitis 1 year earlier.
The average number of middle ear operations due to chronic otitis media ran up to 2.8.
At the time of the study, four patients used a conventional bone conduction hearing aid. None of the subjects had previously been implanted with other systems.
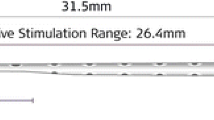
The Sophono Alpha System (SAS) consists of two parts, an implanted magnet and an external digital audio processor [1, 2]. Initially, two magnets hermetically sealed in a titanium case, are fixed to the temporal bone via a surgical procedure. A template is used to mark the site of the incision which is usually located 7.5 cm superiorly and posteriorly to the external auditory canal.
Despite the extended bone removal resulting from subtotal petrosectomy, the site of incision and placement of the SAS magnets remains unchanged in our patients.
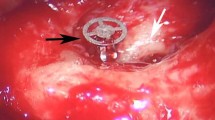
The periosteum is detached from the bone and the precise localization of the magnets is marked on the bone itself. Around the markers, two implant wells are drilled using a 4-mm diamond-cutting burr and the implant is positioned and secured with 5-mm titanium screws (Fig. 2). The skin is closed using resorbable sutures and covered with a pressure bandage for 24 h [1–4]. After 4 weeks, the external Sophono device is fitted and activated (Fig. 3). The latter consists of an audio processor with a bone conduction vibrator, mounted on an acrylic base plate on which 2 external magnets with 5 different grades of strength can be embedded. Each grade increases its strength by 0.53 N [1–4].
Only in one of the patients of our study, was the implanted magnet fixed to the temporal bone at the same time as SP was performed. In the other cases, the mean time between SP and application of the magnet was 29.8 months (range 6–62 months).
According to the manufacturer, the Sophono is designed for patients from 5 years of age or older with conductive hearing loss or mixed loss, if hearing thresholds are >45 dB hearing level [3]. All patients underwent SP having a conductive hearing loss of about 50–60 dB with normal or slightly reduced bone conduction, making them perfect candidates for this type of hearing aid.
All patients or their tutors gave their written informed consent for the above-mentioned operation, the activation of the Sophono processor and their inclusion in this study. All devices were CE marked (approved in European Union) and the prospective study was approved by the local ethics committee.
All patients underwent a clinical follow-up examination after SP and prosthesis implantation. Implant loss, wound healing and skin reactions were monitored. Information about general, social and physical patient benefit after SAS implantation were carefully investigated using the validated Glasgow Benefit Inventory. The GBI is a specific questionnaire designed to evaluate changes in health status after ear, nose, and throat (ENT) surgery [7, 8]. The GBI has been widely used in published literature to evaluate various ENT operations including placement and activation of hearing aids. Other advantage of the GBI is related to the mode of questionnaire administration, because it contains only 18 questions which assess how surgery has altered the quality of life of the person. The response to each question is based on a five-point Likert scale ranging from a severe/notable deterioration in health status toward a great improvement in health status. The average score was then calculated and transposed onto a benefit scale ranging from −100 (maximal negative benefit), to 0 (no benefit), to +100 (maximal benefit) [7, 8, 11].
The patients operated via SP had previously been evaluated with computed tomography (CT) and magnetic resonance imaging (MRI) at 6 months, 1 and 2 years. Since the Sophono titanium plate was considered not compatible with MRI [1] (potential middle ear artifacts), we opted to perform only CT scan to evaluate eventual subsequent disease recurrence afterwards (Fig. 4a, b).
Preoperative hearing tests with Sophono Alpha headband soft band were not performed. Such system is indicated for patients younger than 5, or for those wanting a non-implanted bone conduction hearing device [3].
Audiometry was performed before and after Sophono implantation, using the conventional bone conduction hearing aid. The pre-SOPHONO data were recorded in unaided conditions with headphones and plugging of the contralateral side. These included unaided pure-tone audiometry (frequencies ranging from 0.5 to 4 kHz) with measurement of air conduction, and bone conduction thresholds and speech audiometry, calculating the speech recognition threshold and the percentage of word recognition score at 65 dB. Aided data were measured in the sound field with the unoperated ear plugged and covered with an ear muff (attenuation 30 dB at 125 Hz; 50 dB at 2–4 kHz). Statistical analysis was performed using Student’s t test. A p value <0.05 was considered statistically significant.
Results
None of the patients studied had a history of ear infection following SP.
No adverse skin reactions, abutment-related problems or implant losses occurred in any of the Sophono-implanted patients.
Two patients, who had initially been fitted with a strength 3 (1.6 N) magnet, subsequently preferred to change this with a strength 2 (1.06 N) magnet, because of the discomfort pressure and mild pain it caused.
Another four patients use magnets of similar strength. Only in one case magnet strength 5 (2.6 N) was used, while in the remaining three cases magnet strength 3 was chosen.
In eight patients the external digital audio processor positioned above and behind the ear was totally invisible because hidden within the patients’ hair. In the remaining two cases (males) the visibility of the prosthesis was well accepted and tolerated without psychological discomfort.
All of patients undergoing SAS implantation responded to the GBI questionnaire [7]. General, social and physical benefits were calculated by an average value of each individual questionnaires. General benefit score was calculated in +45.3 (range +20.8 to +75), while, the social benefit was +11.6 (range 0 to +33.3) with +44.9 (range +16.6 to +66.6) for the physical score. The substantial positive impact on patient’s general health status after SP was related to the absence of recurrent otological symptoms.
An overview of audiometric outcomes is listed in Tables 2 and 3. The data before SAS calculated on the mean hearing values of all auditory frequencies for each individual patient had a bone conduction average value of 28.9 dB. The AC mean showed a value of 71.8 dB.
After implantation and activation of the Sophono system audiological data showed an average AC value of 42.1 dB (lowest value 31.2, highest value 53.7 dB). By comparing this data with the values of AC following SP, an average acoustic improvement of 29.7 dB could be calculated, significantly better than the 18.2 dB obtained wearing the traditional bone conduction aid. Despite limited number of the patients comprised in the series analyzed, this result was statistically significant using an unpaired t test (p < 0.0001).
Preoperative SRT was 72.1 dB while WRS at 65 dB was found to be 3 %. After SAS implantation SRT and WRS at 65 dB were greatly increased, achieving mean values of 38 dB and 87.1 %, respectively (p < 0.001). Wearing the conventional bone conduction aids (hearing glasses) in which a vibrator is pressed against the skull, SRT showed mean values of 45 dB, while WRS presented mean values of 78 %, data substantially worse than those obtained by SAS (p < 0.01). Note that no correlation between auditory recovery and the different magnets strength applied was observed.
All of the patients reported better social integration and reduction of psychological discomfort linked to their increased hearing ability.
Discussion
Coker et al. [5] in 1985, first suggested subtotal petrosectomy as suitable treatment for revision surgery in the middle ear or mastoid in patients with chronic or recurrent infection and the related complications including cholesteatoma (primary and secondary). It does not represent the first surgical option for chronic otitis media treatment. However, SP is a valid option for difficult cases of chronic ear disease, since it prevents any possible recurrence or contamination between the external environment and the temporal bone, reducing the risk of meningitis [10]. Although this surgical technique may produce a conductive hearing loss as severe as 50 or 60 dB, it is the only surgical option whose aim is to give the patient, often plagued by chronic discharge, multiple previous surgical procedures, and unserviceable hearing a safe dry ear [5, 10]. There are cases, of recurrent chronic middle ear disease, where even the most experienced otologist is unable to prevent ongoing suppuration despite multiple revision surgeries and careful management of the patient. Therefore, only a meticulous eradication of disease and the creation of a stable cavity able to prevent recurrence can guarantee true therapeutic success in this type of patient.
The restoration of hearing function is a secondary, albeit important, goal [10]. All our patients complained of psychological discomfort due to recurrent middle ear infections, with an average number of middle ear operations due to chronic otitis media reaching 2.8.
A bone conduction hearing aid represents a viable option for a conductive or mixed hearing loss subsequent to SP. These hearing aids are very effective in improving hearing capabilities, but their cosmetic appearance and the discomfort due to pressure on the skull are not always acceptable to patients [12]. This adverse effect can be overcome by the use of an implantable prosthesis. Bone-anchored hearing aids (BAHA) are still today the most widely used bone conduction implants in patients with chronic otitis media, congenital aural atresia or, in the case of repeated surgery, when ossiculoplasty is not feasible due to absent or insufficient middle ear ventilation [13, 14]. In the recent clinical series, a 23.9 % rate of complications was reported [15], most of which were secondary to the abutment of the sound processor or adverse skin reactions [14–16]. These findings may represent an unacceptable condition in some of these patients with a long history of otorrhea who have undergone a relevant number of surgical procedures. However, it must be remembered that no adverse effects of MRI study in patients with BAHA system have been previously reported [4, 6].
Other possible options are middle ear implants. Linder et al. [17] tested the efficacy of the Vibrant Soundbridge device by directly stimulating the round window membrane of five patients undergoing subtotal petrosectomy due to chronic otitis media. The aided postoperative measures revealed that all patients had a remarkable gain of 40 dB in their hearing level, calculated considering the differences between the preoperative air conduction (AC) thresholds and the postoperative aided AC thresholds. All patients were able to obtain 95 and 100 % correct speech discrimination scores at 70–80 dB after proper adjustments. Despite the excellent hearing recovery, the risk of bone conduction threshold worsening as a result of inner ear damage following extensive drilling and placement of the floating mass transducer, must always be considered before choosing this type of implant [17–19]. In the Linder study [17], three patients, presented a temporary threshold shift of <5 dB in the low frequencies. In five patients there was a persistent worsening of bone conduction at 2 kHz ranging from 10 to 30 dB, with preservation of inner ear function at the other frequencies. One patient presented an additional impairment of 15 dB at 4 kHz. Moreover, MRI scans are not compatible with VSB implantation due to the dangerous acoustic trauma and the risk of implant demagnetization and dislocation [17]. The efficacy of VSB after subtotal petrosectomy was also evaluated in another clinical study reported in the literature [18], showing a functional gain of 75 % between postoperative speech perception and the postoperative VSB-aided condition at 65 dB SPL. Unfortunately, in this series too, one patient with preoperative mixed HL, developed an additional HL after a round window application of the VSB device.
In 2010, Sophono Alpha 1, another bone conduction implantable device, was introduced [1, 2, 4]. This implant is a magnetically coupled bone conduction hearing system based on transcutaneous energy transfer TM technology [1, 2]. The system has many advantages compared with BAHA. It is implanted in a simple single-stage procedure, not requiring removal of hair follicles and daily cleaning of wound site. Further, there is no percutaneous abutment with its relative social stigma.
Myrthe et al. [6] compared BAHA and SAS hearing level recovery in 12 patients with congenital unilateral atresia. They found BAHA thresholds to be 5–10 dB better than those of SAS, especially at the high frequencies. Again, the speech reception threshold was 8 dB better for BAHA than Sophono. Although they stated that Sophono users demonstrated poorer aided thresholds, compared to BAHA users, the limited number of patients analyzed should be emphasized. Myrthe et al. [6] confirmed the absence of skin complications related to SAS, whereas they reported a loss of the BAHA implant in one case out of six patients examined.
Alternative treatment to SP in patients with recurrent middle ear disease may be canal wall down mastoidectomy with mastoid obliteration. The materials used in mastoid obliteration usually include the musculoperiosteal flap, bone pate, bone chip, cartilage, fat tissue or more recently nonreabsorbable materials such as methacrylate or hydroxyapatite. However, despite what is expected, the obliterative method has some limitations that includes: the resorption of the organic material employed to obliterate the cavity, difficulty in recognizing cholesteatoma recurrence behind the obliteration, and infection [20–24]. In this surgical technique, the recurrences were estimated between 12 and 16 %.
Few studies dealing with auditory recovery via prosthetic devices have been reported in the literature [25, 26].
Recently, conventional hearing aid tolerance after revision and obliteration of canal wall down mastoidectomy cavities was evaluated [25]. Among 20 subjects analyzed, 7 patients (35 %) had at least 1 temporary period of hearing aid non-use due to excessive otorrhea that required ototopical therapy. Hearing aid use was permanently abandoned in favor of bone-anchored hearing implant in three patients (15 %). In the remaining ten cases (50 %), there was no documented period of hearing aid non-use. George et al. [26] evaluated hearing rehabilitation in six patients who underwent combined BAHA and mastoid obliteration and observed a vast improvement and good sound localization. Another option is offered by the Bonebridge (BB), a new bone-conduction implant system. It consists of an external part, the audio processor, and a subcutaneous implant. It has been designed for adult patients with conductive or mixed hearing loss who do not achieve adequate benefit with conventional hearing aids and are not good candidates for reconstructive middle ear surgery [26–30].
Bonebridge as SAS allows the skin to remain intact overcomes some related issues to percutaneous abutment with audiological outcomes comparable to those of percutaneous BAHA as reported by Huber et al. [28]. First case reports of BB implantation was reported by Lassaletta et al. [29] in April 2013 in a 62-year-old female with a history of bilateral chronic otitis media and hearing loss. Aided thresholds demonstrate a significant benefit, with an improvement from 68 to 26 dB, and speech discrimination score at 65 dB improved from 0 to 85 % 6 months following surgery. Subsequently Manrique et al. [27] reported the use of Bonebridge (BB) in five patients four of whom had conductive/mixed hearing loss due to chronic otitis media. The preoperative PTA average was 66.87 ± 6.3 and 31.25 ± 6.7 dB HL afterward. The 35.62 ± 12.09 improvement was statistically significant (p = 0.0). Barbara et al. [30] in a recent paper calculated an average improvement of the SRT with the BB in comparison to the unaided condition in 36.25 dB. Mastoid pathology or the presence of a previous canal wall down technique may be contraindications for placement of this transcutaneous bone-conduction hearing device in the mastoid area [29]. Finally, it should be remembered that BB leads to extensive artifacts of the neurocranium in MRI [31].
As far as we know, no study concerning the use of SAS in SP patients has previously been reported in the English language literature.
We examined the impact of surgery and subsequent prosthesis implantation on the general, physical and social status of patients by validated GBI. A significant value of +45.3 in the general benefit score was reported by this specific questionnaire.
Arunachalam in 2001 [11] employed the validated Glasgow Benefit Inventory to quantify the changes in life quality of 60 patients receiving treatment with BAHA, reporting a general benefit score of +34 (range +27 to +48). Social benefit was +21 (range +12 to +37) with only +10 (range +2 to +26) for the physical score. Recently, de Wolf et al. [7] evaluated 134 adult patients using BAHA reported a value of +30 in the general benefit with social and physical benefits calculated to be +13 and +7, respectively. In our series, the best results, especially in terms of general and physical benefits were related to the absence of recurrent middle ear infections subsequent to SP, and no percutaneous abutment in SAS.
Our series showed a good patient compliance of the SAS: there were no cases of adverse skin effects, implant revision or implant loss; thus, confirming the data previously described elsewhere [1, 2, 6]. Although four of our candidates to this study declined the SAS implantation for esthetic reasons, none of the patients in the whole group evaluated complained of cosmetic discomfort. This is due to the characteristics of the external device which can easily be hidden by the patients’ hair.
In our study, preoperative hearing test with Sophono Alpha headband were not performed. The system is indicated for patients younger than 5 or those wanting a non-implanted bone conduction hearing device [3]. All our patients were perfectly within the hearing range indicated for Sophono Alpha System implantation. Furthermore, each of them gave consent to placement of the SAS subcutaneous magnet.
After SAS implantation, postoperative mean hearing and mean percentage of SRT and WRS at 65 dB intensity improved significantly. The comparison of hearing results between conventional bone conduction hearing aids (hearing glasses) and SAS demonstrated an improvement of 18.2 vs. 29.7 dB, respectively. These data are slightly inferior to those reported by Linder et al. [17] and substantially analogous to those reported in the study of Verhaert et al. [18]. In our series, four patients complained of severe discomfort due to unilateral hearing ability after SP. After SAS system implantation, this condition completely disappeared in three cases and decreased in the other one.
A final consideration regards the possibility of following up these patients using MRI. Initial SAS studies reported the non-compatibility of this system with MRI, which is an important consideration prior to its placement [1, 2, 6]. However, a recent study described by Nospes et al. [32] states that SAS is approved for 0.2, 1.0 or 1.5 T and, in exceptional circumstances, 3 T MRI.
Obviously the possibility of artifacts cannot be ignored. As expected, the region within 5 cm below the implant cannot be effectively shown by MRI while the area more than 10 cm away does not seem to be significantly affected by artifacts [1–3, 32]. Therefore, all our SP patients were monitored for the risk of recurrent otitis and cholesteatoma using CT scan. A further study is underway to evaluate MRI findings in these SAS-implanted patients.
Conclusion
-
1.
Our preliminary results in a group of SP patients implanted with SAS are encouraging.
-
2.
The transcutaneous implantation prevents an adverse skin reaction. This is essential to reduce the social and psychological discomfort of patients with a long history of middle ear and mastoid infections and multiple surgical procedures.
-
3.
The hearing results showed significantly better outcomes of SAS vs. conventional bone hearing aids (hearing glasses) both in terms of pure-tone and speech audiometry.
-
4.
Esthetically, the prosthesis was well accepted and tolerated with minimal or no psychological discomfort.
-
5.
SAS is compatible with MRI study, however, it is not advisable to monitor patients with recurrent otitis media due to possible artifacts to the middle ear area.
References
Siegert R (2011) Partially implantable bone conduction hearing aids without a percutaneous abutment (Otomag): technique and preliminary clinical results. Adv Otorhinolaryngol 71:41–46
Siegert R (2010) Magnetic coupling of partially implantable bone conduction hearing aids without open implants. Laryngorhinootologie 89:346–351
Sophono, Inc. Dutch physicians manual: 1-20
Mulla O, Agada F, Reilly PG (2012) Introducing the Sophono Alpha 1 abutment free bone conduction hearing system. Clin Otolaryngol 37:168–169
Coker NJ, Jenkins HA, Fisch U (1986) Obliteration of the middle ear and mastoid cleft in subtotal petrosectomy: indications, technique, and results. Ann Otol Rhinol Laryngol 95:5–11
Hol MK, Nelissen RC, Agterberg MJ, Cremers CW, Snik AF (2013) Comparison between a new implantable transcutaneous bone conductor and percutaneous bone-conduction hearing implant. Otol Neurotol 34:1071–1075
de Wolf MJ, Shival ML, Hol MK, Mylanus EA, Cremers CW, Snik AF (2010) Benefit and quality of life in older bone-anchored hearing aid users. Otol Neurotol 31:766–772
Gillett D, Fairley JW, Chandrashaker TS, Bean A, Gonzalez J (2006) Bone-anchored hearing aids: results of the first eight years of a programme in a district general hospital, assessed by the Glasgow benefit inventory. J Laryngol Otol 120:537–542
Magliulo G, Iannella G, Ciniglio Appiani M, Re M, de Vincentiis M. Subtotal petrosectomy and cerebrospinal fluid leakage in unilateral anacusis. JNLS-B (In press)
Sanna M, Dispenza F, Flanagan S, De Stefano A, Falcioni M (2008) Management of chronic otitis by middle ear obliteration with blind sac closure of the external auditory canal. Otol Neurotol 29:19–22
Arunachalam PS, Kilby D, Meikle D, Davison T, Johnson IJ (2001) Bone-anchored hearing aid quality of life assessed by Glasgow Benefit Inventory. Laryngoscope 111:1260–1263
McNeill C, Flint D, Fagan P (2004) Conventional behind-the-ear hearing aids after subtotal petrosectomy with blind sac closure. Otolaryngol Head Neck Surg 131:926–929
Dun CA, Faber HT, de Wolf MJ, Cremers CW, Hol MK (2011) An overview of different systems: the bone-anchored hearing aid. Adv Otorhinolaryngol 71:22–31
Fontaine N, Hemar P, Schultz P, Charpiot A, Debry C (2014) BAHA implant: Implantation technique and complications. Eur Ann Otorhinolaryngol Head Neck Dis 131:69–74
Hobson JC, Roper AJ, Andrew R, Rothera MP, Hill P, Green KM (2010) Complications of bone-anchored hearing aid implantation. J Laryngol Otol 124:132–136
Dun CA, Faber HT, de Wolf MJ, Mylanus EA, Cremers CW, Hol MK (2012) Assessment of more than 1,000 implanted percutaneous bone conduction devices: skin reactions and implant survival. Otol Neurotol 33:192–198
Linder T, Schlegel C, DeMin N, van der Westhuizen S (2009) Active middle ear implants in patients undergoing subtotal petrosectomy: new application for the Vibrant Soundbridge device and its implication for lateral cranium base surgery. Otol Neurotol 30:41–47
Verhaert N, Mojallal H, Schwab B (2013) Indications and outcome of subtotal petrosectomy for active middle ear implants. Eur Arch Otorhinolaryngol 270:1243–1248
Ihler F, Köhler S, Meyer AC, Blum J, Strenzke N, Matthias C, Canis M (2014) Mastoid cavity obliteration and vibrant soundbridge implantation for patients with mixed hearing loss. Laryngoscope 124:531–537
Magliulo G, Ronzoni R, Vingolo GM, Cristofari P (1992) Reconstruction of old radical cavities. Am J Otol 13:288–291
Magliulo G, D’Amico R, Forino M (2001) Reconstruction of the posterior auditory canal with hydroxyapatite-coated titanium. J Otolaryngol 30:330–333
Kang MK, Ahn JK, Gu TW, Han CS (2009) Epitympanoplasty with mastoid obliteration technique: a long-term study of results. Otolaryngol Head Neck Surg 140:687–691
Zhang X, Chen Y, Liu Q, Han Z, Xu A, Ding Y (2005) Long-term results analysis of mastoidectomy for chronic otitis media. Lin Chuang Er Bi Yan Hou Ke Za Zhi 19:870–872
Lee WS, Choi JY, Song MH et al (2005) Mastoid and epitympanic obliteration in canal wall up mastoidectomy for prevention of retraction pocket. Otol Neurotol 26:1107–1111
Gluth MB, Friedman AB, Atcherson SR, Dornhoffer JL (2013) Hearing aid tolerance after revision and obliteration of canal wall down mastoidectomy cavities. Otol Neurotol 34:711–714
George A, Coulson C, Ross E, De R (2012) Single-stage BAHA and mastoid obliteration. Int J Otolaryngol 2012:765271
Manrique M, Sanhueza I, Manrique R, de Abajo J (2014) A new bone conduction implant: surgical technique and results. Otol Neurotol 35:216–220
Huber AM, Sim JH, Xie YZ et al (2013) The Bonebridge: preclinical evaluation of a new transcutaneously-activated bone anchored hearing device. Hear Res 301:93–99
Lassaletta L, Sanchez-Cuadrado I, Muñoz E, Gavilan J (2014) Retrosigmoid implantation of an active bone conduction stimulator in a patient with chronic otitis media. Auris Nasus Larynx 41:84–87
Barbara M, Perotti M, Gioia B, Volpini L, Monini S (2013) Transcutaneous bone-conduction hearing device: audiological and surgical aspects in a first series of patients with mixed hearing loss. Acta Otolaryngol 133:1058–1064
Steinmetz C, Mader I, Arndt S et al. (2014) MRI artefacts after Bonebridge implantation. Eur Arch Otorhinolaryngol (Epub ahead of print)
Nospes S, Mann W, Keilmann A (2013) Magnetic resonance imaging in patients with magnetic hearing implants: overview and procedural management. Radiologe 53(11):1026–1032
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Magliulo, G., Turchetta, R., Iannella, G. et al. Sophono Alpha System and subtotal petrosectomy with external auditory canal blind sac closure. Eur Arch Otorhinolaryngol 272, 2183–2190 (2015). https://doi.org/10.1007/s00405-014-3123-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3123-2