Abstract
Polysomnography is currently considered as the gold standard for the diagnosis of obstructive sleep apnea syndrome (OSAS). But high expense and the backlog of the sleep centers have resulted in a search for an alternative method of diagnosis. The aim of this study is to assess the efficacy and reliability of Watch PAT as an alternate option in OSAS diagnosis. The patients have worn a Watch PAT® 200 device in the sleep laboratory during a standard polysomnography. The correlation in REM and Non-REM AHI scores, sleep periods and the mean O2 saturation percentage between Watch PAT and PSG sleep studies were assessed. There was a statistically significant very strong correlation between PSG and Watch PAT AHI scores (Spearman’s rho = 0.802 p < 0.001). The mean recording time with PSG and Watch PAT was 463.06 ± 37.08 and 469.33 ± 72.81 min, respectively, and there was no statistically significant difference (p = 0.068). However, there was a statistically significant difference between two methods regarding the average sleep time and REM sleep period. No statistically significant difference was revealed in the mean O2 saturation percentage (p < 0.001). Watch PAT is an efficient device and is considered to be an adjunctive diagnostic method for PSG in diagnosis of OSAS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea syndrome (OSAS) which is diagnosed with polysomnography (PSG) is increasing the incidence of cardiovascular and neurocognitive diseases susceptibility in the population as result of the repetitive apnea, hypopnea and arousal episodes occurring during sleep. The prevalence is not known exactly due to the lack of sufficient polysomnographic studies, however, it is estimated to be between 1 and 5 %. The incidence is similar with the diseases such as diabetes mellitus and asthma bronchioles. Underlying mechanism in OSAS is considered to be the upper airway collapse emerging during sleep. Although the risk factors for the emergence and severity of the disease are being known in general, the pathophysiology of this obstruction is still not clearly explained [1, 2].
OSAS diagnosis is made with recording respiratory events during sleep and/or with clinical findings. Gold standard diagnostic method for OSAS is in-laboratory PSG [2, 3]. However, the disadvantages of overnight PSG, such as high cost, backlog of the sleep centers, and the need of qualified personnel, resulted in a number of attempts to develop a new method which could be applied more easily with a better patient compliance, hereby allowing the screening of a greater number of population [4].
Watch PAT 200® (Itamar Medical Ltd., Caesarea, Israel) is one of the devices which has been developed for this purpose. It is a portable instrument capable of measuring four channels which is classified in the 3rd category according to the American Sleep Disorders Association (ASDA) criteria for diagnostic methods. Apnea/hypopneas happening during sleep are recorded by observing the peripheral arterial tone (PAT) and oxygen saturation.
PAT is a physiological signal that reflects the vascular changes caused by the alterations in the autonomic nervous system. It can be followed by measuring the arterial pulsatile volume changes at the fingertip. The respiratory difficulties such as apnea and hypopneas are accompanied by an increase in heart rate, blood pressure, and sympathetic activation. This sympathetic activity increment causes peripheral vasoconstriction [5]. Vasoconstriction in arteries of the finger tip which is reflecting the sympathetic activity is measured as an attenuation in the PAT signal amplitude. The reason for fingertip preference is the presence of rich arteriovenous anastomoses and high blood flow exchange rate (1–100 ccm/100 g/s) in this region [6].
In this study, we aimed to evaluate the efficacy and reliability of Watch PAT device in OSAS diagnosis.
Materials and methods
Study design
This study was simultaneously performed on the subjects whom required PSG test with the preliminary diagnosis of OSAS. The Watch PAT 200® device has been provided by Gazi University within scientific research project. The study has taken place in Atatürk Thoracic Diseases and Thoracic Surgery Training and Research Hospital Sleep Disorders Center between November 2009 and May 2010.
The subjects whom were being suspected of having obstructive sleep apnea were enrolled in the study. Exclusion criteria from the study were experiencing non-sinus cardiac arrhythmia in the last 3 years, having peripheral vasculopathy, neuropathy, severe lymphatic disease or finger deformities, usage of α adrenergic receptor blocker or being addicted to alcohol or to any drug. Primarily the patients have completed a standard questionnaire form (Epworth sleepiness scale) targeting OSAS diagnosis, subsequently they have undergone a through physical examination and their body mass indexes were calculated.
Written informed consent was obtained from the individuals who have agreed to participate in the study and they were given an appointment for the sleep laboratory on different days. They were warned not to take alcohol, not to use any sedative drugs and to be awake in the afternoon of the test day. In the sleep laboratory, they have worn a Watch PAT® 200 device during a standard polysomnography. All the patients have been observed overnight. At the end of the test, two instruments were simultaneously closed and the results were recorded. The study was terminated after 30 patients have been completed. Polysomnographic records were interpreted according to the relevant experts whom were not informed about the outcome of Watch PAT. In 2007 American Academy of Sleep Medicine (AASM) guideline has been accepted as a criterion for the diagnosis of OSAS. The individuals with an AHI score >15 and those with an AHI score between 5 and 15 with the accompanying symptoms (daytime sleepiness, etc.) were diagnosed as OSAS.
Polysomnography
A standard PSG was performed with 44-channel compumedics E series® device. The recorded polysomnographic data included four-channel electroencephalography (EEG-C4A1, C3A2, 02A1, 01A2), electrooculography (EOG), electrocardiography (EKG), chin and leg electromyography (EMG), thoracoabdominal movements, body position, oronasal air flow and oxygen saturation (sO2) with pulse oximetry. Polysomnographic data were evaluated and scored by the physicians in charge of the institution. Apnea and hypopnea index (AHI) was calculated by dividing the total number of apnea and hypopnea events by the total sleep time. Sleep was staged according to the standard criteria. An apnea was defined as complete cessation for at least 10 s and hypopnea is scored if airflow was reduced by 50 % or a lesser extent in association with a desaturation of at least 3 % or an arousal.
Watch PAT 200
In the sleep laboratory, all the patients have worn a Watch PAT 200® device during a standard polysomnography. As shown in Fig. 1, it consists of five parts: PAT probe, snoring sensor, pulse oximetry sensor, actigraphy (embedded in the tool) and body position sensor. PAT signal, oximetry, oxygen saturation measured by finger-mounted probe and the data coming from motion sensor (actigraphy) in the device are all continuously recorded digitally on the SD card which is located in the device. Oximetry probe was applied on the finger tip with a special disposable band to transmit blood oxygen saturation to the recorder device through a pulse oximetry module. Snoring sensor was fixed on the trachea with the help of a special double-sided tape to measure snoring intensity in dB unit. Body position sensor was placed on the patient’s chest region by means of a special double-sided tape to perceive body position in five different configurations (standing, supine, right, left, sitting). After sleep test, all these data were automatically transferred to the computer and these data were analyzed and reported with zzzPAT® software.
Outcome measures
The data derived from PSG were; recording time duration, sleep and awake time duration, sleep efficiency, REM/Non-REM (stage 1, 2, 3) stages of sleep, awake sO2 and minimum sO2 levels, AHI, positional AHI and REM/Non-REM AHI values and the mean heart rate. Recording time duration, sleep and awake time duration, awake, minimum and mean sO2 levels, AHI, positional AHI and REM/Non-REM AHI values, RDI and ODI values were automatically calculated with Watch PAT.
Statistical analysis
The statistical analysis was performed using SPSS version 15.0 (Chicago, Illinois) statistical software package. The descriptive statistics were presented as mean ± standard deviation (SD) and median (min, max). Continuous variables were tested by Kolmogorov–Smirnov test, histograms and P–P test for normality. The parameters were compared by Wilcoxon Signed Rank test. Spearman’s Correlation test was used to test the correlations between these variables. Bland–Altman diagrams were also used to illustrate the difference between two methods; PSG and Watch PAT. In all the tests p < 0.05 was considered to be statistically significant.
Results
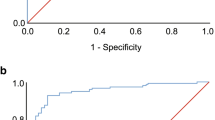
Five women (16.7 %) and 25 men (83.3 %), a total of 30 subjects were included in the study with the ages ranging between 28 and 70 (mean 49.2 ± 9.6). The mean BMI was 29.6 ± 4.4 kg/m2. According to PSG, the AHI scores revealed were, respectively, <5 in two individuals (6.6 %), between 5 and 15 in three patients (10 %) and >15 in the remaining 25 patients (83.3 %). The mean sleep efficiency of the patients was 94.6 % (min: 52 % max: 99.9 %). All the patients except the one with AHI score <5 were diagnosed with OSAS with the symptoms accompanying. However, one of the cases with an AHI score <5 was reported to be >5 according to Watch PAT [positive predictive value (PPV): 0.96]. Primarily overnight AHI score which is preferred in the classification and diagnosis of OSAS was compared between two diagnostic methods. There was a statistically significant very strong correlation between PSG and Watch PAT AHI scores (Spearman’s rho = 0.802 p < 0.001) The agreement between two methods was also illustrated with Bland–Altman spot in Fig. 2. The AHI difference for only one subject (3.3 %) exceeded the limits of agreement as shown in Fig. 2b (meaning Watch PAT AHI was greater than the PSG AHI by more than 1.96 SD from the mean). The mean AHI scores detected by PSG and Watch PAT were 33.5 ± 24.6 and 35.5 ± 26.8, respectively. The difference between two methods based on this variable was observed not to be statistically significant (p = 0.428) as shown in Table 1.
The REM and Non-REM period AHI scores were also compared between PSG and Watch PAT. A high agreement was found between REM (Spearman’s rho = 0.741 p < 0.001) and Non-REM AHI scores (Spearman’s rho = 0.607 p < 0.001). The difference between two methods based on these two variables was observed not to be statistically significant (p = 0.075 and 0.436, respectively) as shown in Table 1.
The comparison of sleep periods was shown in Table 2. The mean recording time with PSG and Watch PAT® was 463.1 ± 37.1 (min: 372.1 max: 539.0) and 469.3 ± 72.8 min (min: 226.0 max: 595.0), respectively, and there was no statistically significant difference (p = 0.068) with high agreement (Spearman’s rho = 0.553 p = 0.002). However, the average sleep time in PSG and Watch PAT was 437.3 (278.5–507.5; SD: 54.6) and 400.9 (216.0–559.0; SD: 76.5) minutes, respectively, and there was a statistically significant difference between two methods (p = 0.016) with statistically low agreement (Spearman’s rho = 0.246 p = 0.19). There was a low agreement between PSG and Watch PAT regarding the REM sleep period, too (Spearman’s rho = 0.249 p = 0.184). However, the mean percentage of REM sleep duration compared to the total sleep duration was 15.9 % (0.7–25.7 SD: 6.1) in PSG whereas it was 21.3 % (4.2–36 SD: 8.5) in Watch PAT®, and there was not a statistically significant difference based on REM sleep duration percentage (p < 0.001).
The mean O2 saturation percentage in PSG and Watch PAT® was 93.1 and 92.6 %, respectively, and statistically significant difference was not found out (p < 0.001).
Discussion
The main purpose of this study was to determine the diagnostic efficacy of Watch PAT in OSAS diagnosis. It is one of the portable devices proposed as an adjunct or alternative method to gold standard method PSG. Therefore, the study has concurrently done in the patients sent to sleep laboratory for PSG test with the preliminary diagnosis of OSAS. There was a high agreement between PSG and Watch PAT® based on AHI scores and we did not observe significant difference between these two ways of assessment (p < 0.001) (Table 1) as consistent with the previous studies.
Bar et al. [7] compared Watch PAT with PSG in 102 (78 male, 24 female) patients with OSAS diagnosis. One group has undergone a concurrent polysomnography and Watch PAT study in the sleep laboratory and the other group has been tested only with Watch PAT device attached at home. According to RDI results, the patients were classified to be between the scores of 0–10, 11–30, 31–50, and >50. At the end of this study high correlation was observed between PSG RDI and Watch PAT® RDI scores. Furthermore, high correlation coefficients were observed between Watch PAT scores obtained in the sleep laboratory and at home. In their opinion inability of the device to distinguish central apnea from obstructive apnea was supposed to be a ignorable disadvantage because of the low incidence of central apnea and the similar treatment options in both pathologies. Ayas et al. [8] have shown a high correlation between PSG and Watch PAT by comparing the AHI values obtained with these two methods. Also in this study of 30 cases the BMI (31.0 ± 7.6 kg/m2) and age (48 ± 14.8) averages were similar to our subjects.
The mainstay of Watch PAT device is measuring PAT signal at the fingers. Grote et al. [6] have shown high correlation of PAT probe with the vasoconstriction of the arteries located in the fingers after giving α sympathomimetics. O’Donnell et al. [10] showed parallel decrease in PAT signals along with the increasing airway obstruction in the patients and named this situation as the dose–response answer in their study. So, PAT signal seems to be a reliable data to predict the presence of apnea and hypopneas.
Oxygen desaturation is suggested to be one of the most important parameters associated with complications in OSAS. For this reason, the patients were followed up for oxygen saturation during night with both polysomnography and Watch PAT device in the study. The average sO2 percentage was 93.1 % with PSG where as it was 92.6 % with Watch PAT, and the difference observed between these two values was not statistically significant (p < 0.001). This finding supports the reliability of Watch PAT® in oxygen saturation monitorization. Pitson and Stradling [11] have shown the decreased peripheric oxygen saturation and the simultaneous activation of the sympathetic system during this apnea–hypopnea periods. Schnall et al. [12] observed high correlation between the total number of apnea–hypopneas revealed by polysomnography and with the changes detected by PAT that is emerging due to the increased sympathetic nervous system activity.
Except two individuals with AHI scores <5, all the remaining patients included in the study have been diagnosed with OSAS according to both PSG and Watch PAT data. Only one of these two individuals was falsely diagnosed with OSAS according to Watch PAT (PPV:0.96). With this study group we cannot make any comment for negative predictive value of Watch PAT in OSAS diagnosis. Nevertheless, Watch PAT has been found to be a reliable, portable device in the diagnosis of OSAS as compatible with the findings of earlier studies [7, 8].
Male/female ratio was found to be fivefold in the study group. However, OSAS is estimated to affect approximately 4 % of adult men and 2 % of adult women in the population [13]. It may be attributed to the small number (30) of the sample size. In addition, the atypical symptoms such as insomnia, restless leg and depression that women are suffering make them less likely to be referred for the evaluation of sleep disordered breathing [14].
One of the objectives of the sleep studies is to identify the sleep stages and to determine the relationship between respiratory events and these stages. In our study, a strong correlation revealed within PSG and Watch PAT based on REM/Non-REM AHI scores (p < 0.001). According to this finding Watch PAT may be used in the diagnosis of sleep period associated OSAS such as REM-dependent OSAS which is getting more attention and highlighted each passing day. Hedner and colleagues have shown good agreement between PSG and Watch PAT in detecting REM sleep periods previously [15].
However, sleep/awake times and the duration of REM sleep periods of the patients were significantly different between PSG and Watch PAT (p < 0.05) in our study. This situation may conflict with the hypothesis above. Increased sympathetic activity results in PAT signal attenuation which in turn helps to identify REM sleep [16]. Longer REM sleep durations recorded with Watch PAT thus may be related to sympathetic activity increment occurring due to different physiological alterations. The mean sleep efficiency of the patients was 94.6. There was a patient with a sleep efficiency of 52 % in whom the AHI scores obtained with PSG and Watch PAT were 35.5 and 17.7, respectively. Thus, it may be better to include the individuals with insufficient sleep durations in another study to examine whether Watch PAT is capable of perception the different sleep periods.
Ceylan and his colleagues [17] came up with a similar finding in their study. They have shown that Non-REM 1 and 2 sleep stages were found to be compatible with PSG, but compliance was not found in Non-REM stages 3 and 4. Watch PAT REM sleep periods were shown to be in low agreement with PSG.
One of the most important points of this study is performing the sleep test only in the sleep laboratory. This may conflict with the main objective of the device, availability to perform the test at the individual’s home setting. However, there are other researchers in the literature already confirming the reliability of the assessment carried out at home environment, therefore, we did not see a necessity to evaluate this issue again [7]. Also, we aimed to overcome a possible ‘first night effect’ difference between PSG and Watch PAT by this way.
First night effect, one of the issues mentioned for the sleep studies is considered as the changing in the quality of the sleep due to the different test days as well as to the personal analyzing the test. It is especially encountered in the sleep laboratory PSG tests. Lewendowski and colleagues [18] compared the polysomnographic records of 118 patients in the course of diagnosis and 1 month later. AHI levels varied slightly between the two groups, but the difference was not significant. Many researchers agree that this problem can be eliminated with portable devices [7, 9].
Conclusion
Currently, the gold standard method for the diagnosis of OSAS is the PSG performed in the sleep laboratories. However, the limited number of sleep laboratories and PSG has resulted in a search for an alternative method of diagnosis. Therefore, in our study, we have evaluated the efficacy of Watch PAT 200® device which is considered to be an alternative or adjunctive diagnostic method for PSG in diagnosis of OSAS.
In the light of our findings, OSAS can be diagnosed securely with Watch PAT device in the laboratory. However, the accuracy of Watch PAT in determining the separate stages of sleep (REM and Non-REM) needs to be evaluated with further studies.
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep disordered breathing among middle-aged adults. N Engl J Med 328(17):1230–1235
Bennett JA, Kinnear WJ (1999) Sleep on the cheap: the role of overnight oximetry in the diagnosis of sleep apnoea hypopnoea syndrome. Thorax 54(11):958–959
Young T, Evans L, Finn L, Palta M (1997) Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle aged men and women. Sleep 20(9):705–706
American Academy of Sleep Medicine (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurements techniques in clinical research; the report of an American Academy of Sleep Medicine Task Force. Sleep 22(5):667–689
Pang KP, Gourin CG, Terris DJ (2007) A comparison of polysomnography and the WatchPAT in the diagnosis of obstructive sleep apnea. Otolaryngol Head Neck Surg 137(4):665–668
Grote LB, Hedner J, Ding Z (2001) Alteration of digital pulse amplitude reflects alpha adrenoceptor mediated constriction of the digital vascular bed. Sleep 24(Suppl):A79
Bar A, Pillar G, Dvir I, Sheffy J, Schnall RP, Lavie P (2003) Evaluation of a portable device based on peripheral arterial tone for unattended home sleep studies. Chest 123(3):695–703
Ayas NT, Pittman S, MacDonald M, White DP (2003) Assessment of a wrist-worn device in the detection of OSA. Sleep Med 4(5):435–442
Cirignotta F, Mondini S, Geradi R, Mostacci B, Sancisi E (2001) Unreliability of automatic scoring of MESAM 4 in assessing patients with complicated obstructive sleep apnea syndrome. Chest 119(5):1387–1392
O’Donnell CP, Allan L, Atkinson P, Schwartz AR (2002) The effect of upper airway obstruction and arousal on peripheral arterial tonometry in obstructive sleep apnea. Am J Respir Crit Care Med 166(7):965–971
Pitson DJ, Stradling JR (1998) Autonomic markers of arousal during sleep in patients undergoing investigation for obstructive sleep apnea, their relationship to EEG arousals, respiratory events and subjective sleepiness. J Sleep Res 7(1):53–59
Schnall RP, Slitner A, Sheffy J, Kedar R, Lavie P (1999) Periodic, profound peripheral vasoconstriction: a new marker of obstructive sleep apnea. Sleep 22(7):939–946
Young T, Peppard PE, Gottlieb DJ (2002) Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 165(9):1217–1239
Valipour A (2012) Gender-related differences in the obstructive sleep apnea syndrome. Pneumologie 66(10):584–588
Hedner J, White DP, Malhotra A, Herscovici S, Pittman SD, Zou D et al (2011) Sleep staging based on autonomic signals: a multi-center validation study. J Clin Sleep Med 7(3):301–306
Lavie P, Schnall RP, Sheffy J, Shlitner A (2000) Peripheral vasoconstriction during REM sleep detected by a new plethysmographic method. Nat Med 6(6):606
Ceylan T, Fırat H, Kuran G, Ardıç S, Bilgin E, Celenk F (2012) Quick diagnosis in obstructive sleep apnea syndrome: watchPAT-200. Iran Red Crescent Med J 14(8):475–478
Lewendowski DJ, Zack N, Rao S, Wong K, Gendreau M, Kranzler J et al (2009) Assessment of the test-retest reliability of laboratory polysomnography. Sleep Breath 13(2):163–167
Acknowledgements
We thank Dr. F. Nur Aksakal from Gazi University Public Health Department for her assistance in statistical analysis. This study was supported by Gazi University Scientific Research Projects Department with the code number 01/2009–31.
Conflict of interest
There is no conflict of interest within the authors of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Körkuyu, E., Düzlü, M., Karamert, R. et al. The efficacy of Watch PAT in obstructive sleep apnea syndrome diagnosis. Eur Arch Otorhinolaryngol 272, 111–116 (2015). https://doi.org/10.1007/s00405-014-3097-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3097-0