Abstract
Little is known on the role of the senses smell and taste in end-of-life care. The presented systematic literature analysis investigates the significance of smell and taste in palliative care. The online databases PubMed, CINAHL, MEDLINE, Deutsche Nationalbibliothek and British National Library were searched for English and German literature published between 1970 and April 2013 containing any kind of original data on the impact of smell and taste in patients in a palliative care situation. All retrieved publications were screened for relevance and full text was obtained for all articles identified as relevant. We integrated 13 papers for further analysis (explorative surveys 5, clinical trials 3, case studies 2, qualitative study 1, brief report 1, clinical report 1). Prevalence of smell and taste alterations in palliative care ranges between 60 and 86 %. Existing literature reflects the significance of smells and tastes in palliative care setting in two main streams—smell and taste alterations as symptoms and malodorous wounds. Prevalence of smell and taste alterations in palliative care is high. However, in palliative care literature concepts for the assessment and fostering of subjective significance of smell and taste and the individual impact of significant smells and tastes are predominantly neglected. Available instruments should be characterized, validated and adapted for the use for palliative care patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Palliative care is dedicated to improving the quality of life of people suffering from incurable diseases. Improving the quality of life implies alleviating symptoms, as well as supporting in case of psychological, social, nursing or spiritual problems. At the same time, it aims at employing individual resources and improving comfort and well being for patients and their families.
Beside many other environmental factors, smells and tastes may play important roles in this context. These senses are able to detect environmental olfactory or gustatory substances if incorporated through the nasopharyngeal space. For example, smelling and tasting are daily experiences during dietary intake. They hint at the significance of chemical senses on well being. Studies show the effect of aging on taste and smell [2] and the general suffering of patients with smell and taste disorders [12]. But little is known about the significance of smell and taste in end-of-life care for people suffering from incurable diseases irrespective of their age. To gain a broader insight into the field we performed a systematic literature review with a broad approach on general significance of smell and taste in palliative care.
Aim
The presented systematic literature review investigates the significance of smell and taste in palliative care.
Design and data sources
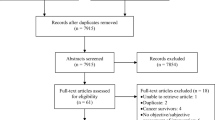
The online databases PubMed, CINAHL, MEDLINE, Deutsche Nationalbibliothek, and British National Library were searched for English and German literature containing original data published between 1970 and April 2013. The search process was guided by theory. Figure 1 presents an overview of the search strategy.
Literature selection
Search terms and combinations used are shown in Table 1. Not only A-level (randomized, controlled, prospective) studies were included because scientific literature with less evidence may as well contain important information about the significance of smell and taste in palliative care.
Exclusion criteria, such as results concerning cancer therapy induced chemosensory alterations as well as literature mentioning smell and taste or palliative care casually/marginal, are defined and listed in Table 2.
Data extraction
Information on general characteristics of the literature was collected, using a standardized extraction form. The research questions of the studies were extracted and allocated by issues, see Fig. 2.
Results
Articles identified
For the period under review the search retrieved 947 publications. Potential relevant literature (n = 74) identified by titles was included (Fig. 1). Hand searching in the articles’ references showed additional results (n = 10). Duplets (n = 9), literature not available or other languages than English or German (n = 6) as well as literature that did not match the inclusion criteria (n = 56) after searching the abstract were excluded. Literature which matched the criteria (n = 13) was included with no regard to the kind of literature. We identified 13 papers for further analysis (explorative surveys 5, clinical trials 3, case studies 2, qualitative study 1, brief report 1, clinical report 1). Table 3 shows the studies with research question, design, instruments and main results. In the five explorative surveys population varies from 15 to 192 patients. Of the controlled clinical trials one is a pilot RCT. One cross-sectional qualitative study was found.
Issues
The significance of taste and smell in palliative care found in literature first and foremost refers to smell and taste alterations as symptoms in palliative care patients and to malodorous wounds (Fig. 2). The results are reported in detail below.
Smell and taste alterations as burdening symptoms
Smell and taste alterations are perceived as burdening symptoms in palliative care. Studies describe the occurrence of smell and taste alterations in palliative care patients for different population groups and show a range from 60 to 86 % [1, 3, 13, 14, 17, 24]. For details, see Table 4. Data about smell and taste alterations are collected either by self-assessments of the patient or by psychophysical measurements on the status of smell and taste functions. The distinction between orthonasal and retronasal smelling and the ability to taste are often not specified in everyday life [11]. Self-assessment tests do not discern between gustatory function and retronasal smelling. Table 4 shows that the ability to taste is tested with the Henkin’s 3-drop or other dilution tests in two studies [14, 17]. Orthonasal and retronasal smelling were not distinguished in any of the studies. The ability to smell is tested with Sniffin’ Sticks and odors in bottles in two studies [17, 24]. Taste alterations belong besides dry mouth to the most frequently encountered self-reported symptoms of the oral cavity in palliative care patients [1, 7, 13]. Some studies try to characterize chemosensory alterations in palliative care patients [3, 7, 14]. Brisbois et al. [3] divide perceived taste and smell changes of palliative care patients into those who are characterized by stronger sensation, weaker sensation and mixed types of changes. Hutton et al. [13] distinguish groups of patients with mild, moderate and severe chemosensory complaints. Subjective chemosensory alterations are often described by patients as bad taste in the mouth, taste distortion, loss of all food tastes, decreased sensitivity for sweet and altered bitter sensation, and heightened sensitivity to odors [13]. Most of these subjective smell and taste alterations can be confirmed with psychophysical tests [14] but vice versa not all persons with evidence of altered olfactory function were aware of it [24]. Psychophysical measures showed frequently decreased sensitivity for sweet and significantly lower gustatory detection thresholds for bitter, salt and sour tastes in patients with advanced cancer than in controls [7, 14, 17]. Microbiological findings of yeasts for 72 patients of 101 patients at a palliative care unit compared to 37 % of working population from unpublished data cited in [1] show remarkable high incidence of candida in palliative care patients. Taste alterations go together with a positive culture result of candida in 78 % of the cases [1].
Taste alterations were associated with weight loss and anorexia [3, 5, 7, 14]. Complex taste alterations frequently go together with patient-reported food aversions and food odors aversions [7, 14].
No significant coincidence between chemosensory alterations or patient-reported food aversions and kind of cancer, gender or the symptom nausea was found [3, 7]. This study results suggest the occurrence of taste alterations, unattached from tumor therapy [3, 13, 24], being part of the process of cancer diseases [17]. Increased smell sensitivity is as well reported and measured by patients with advanced cancer [3, 13, 17]. Weak statistical significant correlation between the olfactory function and the use of opioids (p = 0.02), benzodiazepine (p = 0.03) and tricyclic antidepressant (p = 0.01) was reported by Yakirevitch et al. [24]; Alt-Epping et al. [1] did not find significant correlations in patients treated with opioids or lorazepam. A pilot study indicates that delta-9-tetrahydrocannabinol (THC) relieves chemosensory alterations of patients with cancer diseases [4]. Patients with chemosensory alterations estimated their quality of life lower than patients without chemosensory alterations [3, 13, 17].
Wound malodor
Wound malodor may distress patients, families and professional caregivers concerning psychological aspects, body image and quality of life [8]. Not healing the wound but improving the patient’s quality of life is often defined as the primary aim for many patients in a palliative care situation suffering from an ulcerated, malodorous tumor [15]. Possible causes of wound malodor, benefits of activated charcoal dressings and other methods and material for management and containment of malodor for wounds in palliative care are described in the literature in case studies and clinical reports [8, 15]. The two case studies describe psychological as well as physiological aspects of malodorous wounds and the multidisciplinary palliative care approach. West’s [21] case study illustrates exemplarily the difficulties of managing wound odors for a patient with various dressings and the patients distress with the wound itself, the odors and the fact that it seemed impossible to find an adequate solution. In the described case, self-management strategies using aftershaves or aromatized oils had failed to comfort the patient. Psychological distress and alterations of well being and comfort were met with psychological support. Strategies like opening the window, change clothing and bedding helped the patient. Oral metronidazole for odor control and systematic antibiotic therapy for suspected infection brought benefit. All treatments aimed to improve the quality of life of the patient. As soon as the malodor was under control, the aromatherapy was used with benefit. The patient’s wife felt stressed and received practical and emotional support from team members; the nurses were distressed due to the complex situation. The impact of the management of malodors wounds in palliative care on caregivers was examined in a qualitative study [22]. Isolation of patients and altered body image challenged the nurses the most.
Discussion
This is—to the best of our knowledge—the first systematic analysis of the literature addressing the role of the senses taste and smell in patients in a hospice or palliative care situation. The number of publications we found was rather small. This is surprising as it appears to be in contrast to the high occurrence of the problem, as 60–86 % of the population under review suffers from taste and smell alterations. Above that alteration in that field are found to be burdening. Epidemiological studies about the prevalence of symptoms due to chemosensory alteration in end-of-life care patients are not available as they are for other population groups [16]. The focused population of end-of-life care patients is an inhomogeneous patient group. Chemosensory alterations associated with neurodegenerative disease [9] and chemosensory dysfunctions caused by cancer localization and age-related changes [2] may be relevant for patients receiving palliative care.
Psychophysical tested taste and smell alterations in palliative care patients are no indication for treatment itself. Patients’ subjective sensations about their chemosensory functions, perceived alterations and changes should be in the focus. The comparison of psychophysical tests and self-assessments of chemosensory functions, not only in the palliative care context, shows that smell and taste alterations are assessed more frequently than they are subjectively sensed/perceived [16, 24]. For end-of-life care patients who report burdening smell- and taste-associated symptoms, some authors suggest combined methods to get detailed information about taste and smell capabilities to enhance possibilities to find appropriate solutions [5]. To palliate symptoms due to chemosensory alterations, attention on possible causes like high coincidence of candida infection [1] and side effects of medication [1, 24] might help in treatment. The literature-searching method excluded patients with cancer in an earlier stage and patients being in cancer therapy like chemotherapy or radiation. Nevertheless, many patients receiving palliative care are likely to be affected as well by chemosensory consequences of chemo- or radiotherapy or possibly of long-term effects. If sensory complaints result from damaged sensory receptors, the treatment differs from cases where learned food aversion because of chemotherapy intervention is in focus [19]. Effects of chemosensory alterations on the dietary intake of palliative care patients are only relevant if the limited nutritional intake and taste sensation influence the patient’s quality of life. The nutritional status and calories intake standards usually do not play a dominant role in terminally ill and dying patients. However, subjective smell and taste alterations and food aversions could be symptoms itself, and on the other hand, effective treatment could regain food enjoyment and well being.
Management of taste and smell disturbance in palliative care could refer to strategies of other patient groups [18, 23] who perceive chemosensory alterations and feasibility of other innovative treatment approaches, e.g. olfactory training to prevent olfactory deterioration [20] should be analyzed for end-of-life care patients as well. Self-management strategies of patients in end-of-life care should, similar to patients in chemotherapeutical treatment [18], be studied to use the experience for palliative care and counseling.
Increased smell sensations are described as smell alterations in palliative care patients and should be taken into account in palliative care. Food odors could provoke food aversions and cause nausea. Caregivers should be sensible about increased smell sensations. Odors seem to have more impact in palliative care in their negative manifestation, for example, malodors in wound management. Treatment and management of malodorous wounds are part of comprehensive palliative care with the aim to prevent or reduce psychological and social suffering. Surprisingly, the research results did not explicitly address aromatherapy interventions while aromatherapy is discussed in palliative care context.
Overall smells and tastes in palliative care are secondarily mentioned in the context of enhancing enjoyment, pleasure and well being. Smells and tastes are rarely seen as resources. Smells and tastes could be significant for well being and quality of life, even for patients who complain about smell and taste alterations and for patient with malodorous wounds. The environmental factors smell and taste stand out due to their individual subjective significance in ecological, cultural and biographical regard and could act as resources in these contexts [10]. Daily smells and tastes frequently have autobiographical significance, function as environmental composition, convey confidence and evoke remembrances and even in situations of restricted physical condition could enhance well being, awareness and quality of life.
Limitations
The review is restricted due to the small amount of identifiable papers and the limited quality of the evidence. Above that as the population in focus was the palliative care patients, the results cannot be generalized for patients in earlier stages of diseases. More research is urgently needed, but—despite the mentioned limitations—this systematic literature review may foster more rigorous research not only on the role of the senses smell and taste in end-of-life care, in terms of assessment, but also about smells and tastes as a resource in comfort care.
Conclusions
Most studies found in this review describe their study population with regard to chemosensory function, nutritional aspects and quality of life. To date, there is little evidence for useful and adequate alleviation of chemosensory dysfunction and alterations in palliative care but many clinical approaches.
The investigation of appropriate treatment approaches to improve smell and taste alterations is relevant in palliative care context if the chemosensory complaints are identified as burden and distress for the patient negatively influencing their quality of life. A systematic search process seems to be necessary to identify existing instruments used for chemosensory complaints assessments [23] and significance [6]. The available instruments should be characterized, validated and adapted for the use for palliative care patients. They should avoid additional burden, be simple and well structured and take into account the concepts of care like Basale Stimulation® and others. So far palliative care seems to neglect concepts for the assessment and fostering of subjective significance of smell and taste and the individual impact of significant smells and tastes. Individual taste and smell biographies and appropriate interventions allow using them as resources.
References
Alt-Epping B, Nejad RK, Jung K et al (2012) Symptoms of the oral cavity and their association with local microbiological and clinical findings—a prospective survey in palliative care. Support Care Cancer 20:531–537
Boyce JM, Shone GR (2006) Effects of aging on smell and taste. Postgrad Med J 82:239–241
Brisbois TD, De Kock IH, Watanabe SM et al (2011) Characterization of chemosensory alterations in advanced cancer reveals specific chemosensory phenotypes impacting dietary intake and quality of life. J Pain Symptom Manag 41:673–683
Brisbois TD, De Kock IH, Watanabe SM et al (2011) Delta-9-tetrahydrocannabinol may palliate altered chemosensory perception in cancer patients: results of a randomized, double-blind, placebo-controlled pilot trial. Ann Oncol 22:2086–2093
Brisbois TD, Hutton JL, Baracos VE et al (2006) Taste and smell abnormalities as an independent cause of failure of food intake in patients with advanced cancer—an argument for the application of sensory science. J Palliat Care 22:111–114
Croy I, Buschhüter D, Seo H et al (2010) Individual significance of olfaction: development of a questionnaire. Eur Arch Otorhinolaryngol Head Neck 267:67–71
Dewys WD, Walters K (1975) Abnormalities of taste sensation in cancer patients. Cancer 36:1888–1896
Gethin G (2011) Management of malodour in palliative wound care. Br J Commun Nurs 16:6
Hatt H (2007) Geschmack und Geruch. In: Schmidt RF, Lang F (eds) Physiologie des Menschen. Springer Medizin Verlag Heidelberg, Berlin, Heidelberg, pp 422–436
Heckel M, Rester D, Seeberger B (2012) Und den Geschmack habe ich heute auch noch auf der Zunge. Geruch und Geschmack im Lebensverlauf—Ein qualitatives Experiment. Forum Qual Sozialforschung 13:art. 3
Heilmann S, Strehle G, Rosenheim K et al (2002) Clinical assessment of retronasal olfactory function. Arch Otolaryngol Head Neck Surg 128:414–418
Hummel T, Landis BN, Huttenbrink KB (2011) Smell and taste disorders. GMS Curr Top Otorhinolaryngol Head Neck Surg 10:doc04
Hutton JL, Baracos VE, Wismer WV (2007) Chemosensory dysfunction is a primary factor in the evolution of declining nutritional status and quality of life in patients with advanced cancer. J Pain Symptom Manag 33:156–165
Mahmoud FA, Aktas A, Walsh D et al (2011) A pilot study of taste changes among hospice inpatients with advanced cancer. Am J Hosp Palliat Care 28:487–492
Morris C (2008) Wound odour: principles of management and the use of ClinicSorb. Br J Nurs 17(6):38–42
Murphy C, Schubert CR, Cruickshanks KJ et al (2002) Prevalence of olfactory impairment in older adults. J Am Med Assoc (JAMA) 288:2307–2312
Pattison R (1999) Alteration in taste perception and its relationship with nutritional status and quality of life in patients with advanced cancer. Queen Margaret University College, Edinburgh, UK
Rehwaldt M, Wickham R, Purl S et al (2009) Self-care strategies to cope with taste changes after chemotherapy. Oncol Nurs Forum 36:E47–E56
Schiffman SS (2007) Critical illness and changes in sensory perception. Proc Nutr Soc 66:331–345
Schriever VA, Lehmann S, Prange J et al (2014) Preventing olfactory deterioration: olfactory training may be of help in older people. J Am Geriatr Soc 62:384–386
West D (2007) A palliative approach to the management of malodour from malignant fungating tumours. Int J Palliat Nurs 13:137–142
Wilkes LM, Boxer E, White K (2003) The hidden side of nursing: why caring for patients with malignant malodorous wounds is so difficult. J Wound Care 12:76–80
Wismer WV (2008) Assessing alterations in taste and their impact on cancer care. Curr Opin Support Palliat Care 2:282–287
Yakirevitch A, Bercovici M, Migirov L et al (2006) Olfactory function in oncologic hospice patients. J Palliat Med 9:57–60
Acknowledgments
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflict of interests to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heckel, M., Stiel, S. & Ostgathe, C. Smell and taste in palliative care: a systematic analysis of literature. Eur Arch Otorhinolaryngol 272, 279–288 (2015). https://doi.org/10.1007/s00405-014-3016-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3016-4