Abstract
The Swedish National Registry for Tonsil Surgery has been operational since 1997. All ENT clinics in Sweden are encouraged to submit data for all patients scheduled for tonsil surgery. Preoperatively, age, gender and indication are recorded. Postoperatively, method (tonsillectomy or tonsillotomy), technique, and perioperative complications are recorded. Postoperative bleedings, pain, infections, and symptom relief are assessed through questionnaires. An earlier report from this registry showed that tonsillotomy had become more common than tonsillectomy in children with tonsil-related upper airway obstruction. The aim of this study was to categorize which instruments were used for tonsillotomy in Sweden and to compare their outcome and complication rate. All children 2–18 years, reported to the registry from March 2009 until September 2012, who underwent tonsillotomy on the indication upper airway obstruction, were included in the study. 1,676 patients were identified. In 1,602 cases (96 %), a radiofrequency instrument was used. The postoperative bleeding rate was low (1.2 %) and the degree of symptom relief was high (95.1 %). Three different radiofrequency instruments (ArthroCare Coblation®, Ellman Surgitron®, and Sutter CURIS®) were used in 96 % of the patients. There were no significant differences in the number of postoperative bleedings, postoperative infections or symptom relief between the instruments. The only difference found was in the number of days on analgesics, where more days were registered after use of Coblation®. In Sweden, radiofrequency tonsillotomy is the dominant surgical technique used for tonsil hypertrophy causing upper airway obstruction in children. There are no significant differences in outcome between the different radiofrequency instruments except for number of days on analgesics after surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A quality assurance system for tonsil surgery, in the form of a national register, has been operational in Sweden since 1997. There are several aims for this registry: one is to describe the current practice and trends in Swedish tonsil surgery, a second is to provide outcome data to facilitate quality improvement and to work for increased patient safety, and a third is to provide a complement to randomized studies to evaluate outcome and complications of tonsil surgery. One strength of a national registry is that large amounts of data can be gathered in a relatively short time.
All ENT clinics in Sweden are encouraged to record all patients planned for tonsil surgery in the registry. In 2012, the registry had a completeness of 75 % (the proportion of patients registered) and a coverage of 78 % (the proportion of participating ENT clinics).
Several reports based on data from The National Tonsil Surgery Register in Sweden have been published previously. In 2011, our group reported a decreased risk for primary bleeding after tonsil surgery between 1997 and 2008 that at least in part could be explained by a shift from tonsillectomy to tonsillotomy [1]. In 2012, we reported that the most common indication for tonsil surgery in Sweden between 1997 and 2008 was upper airway obstruction (50 %) followed by recurrent tonsillitis (35 %) and that >92 % of the patients (regardless of indication for surgery) reported a high degree of symptom relief 6 months after surgery [2]. In 2013, we could report that tonsillotomy showed lower rates of both early and late postoperative bleedings compared to tonsillectomy with comparable rates of symptom relief [3] and also that tonsillotomy had replaced tonsillectomy as the most commonly performed tonsil surgery in children with tonsil-related upper airway obstruction [3].
A preliminary analysis of registry data has indicated that an overwhelming majority of tonsillotomies are performed with radiofrequency instruments. Common for all radiofrequency-based techniques is that the energy delivered by the instrument (usually a probe, sling, or needle) simultaneously divides tissues and coagulates blood vessels with a minimal amount of thermal damage to the surrounding tissues compared to conventional electrosurgical devices [4–6]. Since there is less damage to the remaining tissues, faster healing with less pain can be expected over the postoperative period. When performing tonsillotomy with radiofrequency, there is also reduced risk for postoperative bleeding since tonsil tissue is left in the tonsillar bed with less risk to damage feeding blood vessels. Although the use of radiofrequency instruments in tonsil surgery seems to have spread rapidly in Sweden and elsewhere, no inventory of which radiofrequency instruments are actually in use has been published thus far. Furthermore, there are no reports that compare outcome and complication rates after tonsil surgery between different radiofrequency instruments in pediatric populations.
The aim of this paper is to describe the prevalence of use of radiofrequency instruments for pediatric tonsillotomy on the indication upper airway obstruction/snoring in Sweden between 2009 and 2012. Additional aims are to compare rates of early and late bleedings, postoperative pain, postoperative infections, and self-rated symptom relief 6 months after surgery in relation to which radiofrequency instrument is used for surgery.
Materials and methods
The National Tonsil Register in Sweden collects data through four questionnaires (preoperatively, postoperatively, 30 days after surgery, and 6 months after surgery). Age, sex, social security number, and indication for surgery are recorded in the first questionnaire. The second questionnaire records surgical method (i.e., tonsillectomy or tonsillotomy), surgical instrument (cold steel, radiofrequency diathermy scissors, ultrascission, laser, or other), and which kind of apparatus was used, and postoperative bleedings occurring during hospital stay. The first and second questionnaires are filled in by the surgeon. The third questionnaire (which is mailed to the patient 30 days after surgery) contains several questions of which the following are relevant to this study: “Was your child readmitted to hospital because of bleeding from the throat?”, “How many days did your child take painkillers?”, and “Did your child receive antibiotics because of an infection?”. The fourth questionnaire (mailed to the patient 6 months after surgery) records data on symptom relief. A multiple-choice question is used: “My symptoms are gone”, “My symptoms are almost gone”, “My symptoms remain”, and “My symptoms have worsened”.
Data for this study were retrieved from the registry in December 2012. Only data collected after the registry was revised in March 2009 were used. All patients aged 2–18 years that underwent tonsillotomy because of tonsil-related upper airway obstruction/snoring were included. In order to allow at least 6 weeks for all questionnaires to be gathered and registered, only patients operated through September 2012 and May 2012 were used in the analysis of data gathered in the 30-day and 6-month questionnaires, respectively.
Cases where adenoidectomy was performed simultaneously were not included, since only adenoidectomy as a procedure is recorded in the registry while the instrument used is not. Another reason to exclude the combined procedure of tonsil and adenoid surgery is that it in many cases is impossible to determine the origin of a postoperative bleeding (i.e., tonsillar bed or epipharynx). In this study, bleedings that occurred during hospital stay are defined as “early” and bleedings that occurred after discharge are defined as “late”. Concerning early bleedings, only those that required any kind of intervention (pharmaceutical treatment, surgery or blood transfusion) are recorded. Late bleedings are those that resulted in readmission to hospital. Postoperative infection is defined as infections treated with antibiotics within the first month after surgery. Postoperative pain is measured by the number of days that the patient used analgesics.
Statistical analysis
Results for categorical variables, including dichotomous variables, are described with number and percentages. Continuous variables are described with mean. Fisher’s exact test was used for comparison between two groups for dichotomous variables and the Mantel–Haenszel χ 2 was used for ordered categorical variables. The Mann–Whitney U test was used for comparison of continuous variables between the two groups. All the tests were two-tailed and conducted at the 1 % significance level. Statistical analysis was performed using SAS version 9.2.
Results
A total of 1,676 tonsillotomy patients were registered from March 2009 through September 2012. Of these, 96 % (1602) were operated with a radiofrequency instrument.
Ambulatory surgery was used in more than 75 % of the cases. The proportion of ambulatory surgeries in relation to radiofrequency instrument was comparable.
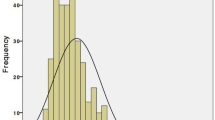
Mean age at surgery was 7.2 years (boys, 6.6 years; girls, 7.9 years) and median age was 6 years (boys 5 years, girls 6 years). There was no significant difference in age distribution between the children operated with different radiofrequency instruments. A slight majority (53 %) of the patients were male.
The response rate was 78 % for the 30-day questionnaire and 51 % for the 6-month questionnaire.
Four different RF instruments were identified: ArthroCare Coblation®, Sutter CURIS®, Ellman Surgitron®, and Olympus Celon (Table 1). Only one clinic reported use of more than one radiofrequency instrument.
According to the description given by the manufacturers of the function of the instruments, the Ellman Surgitron® and the Sutter CURIS® devices are similar. Both instruments use a “monopolar” sling or needlelike device to deliver RF energy (>4.0 MHz) that excite electrolytes in the tissues to cut and coagulate [4, 6]. Therefore, the Ellman Surgitron® and the Sutter CURIS® instruments were grouped together in the further analysis. The ArthroCare Coblation® instrument is somewhat different since it uses radiofrequency energy to excite electrolytes in a saline solution delivered at the tip of a probe to divide tissue and coagulate vessels [5]. Since the Olympus Celon device was used in ~1 % of the surgeries, patients operated with this instrument were excluded from further analysis.
Data on early and late postoperative bleedings, postoperative infections, and use of analgesics are shown for each radiofrequency instrument in Table 2. There was no significant difference between the different surgical devices with respect to bleeding or postoperative infections or symptom relief. The number of days on analgesics differed with a mean of 1 day more for ArthroCare Coblation® in relation to the other options.
Discussion
Data from the National Tonsil Surgery Register in Sweden provides unique opportunities to study aspects of tonsil surgery. The high coverage, including 75 % of all tonsil surgery procedures performed in Sweden, guarantees highly representative and rapidly accumulating amounts of data. The current practice for tonsil surgery changes over time. New techniques and instruments for tonsil surgery are introduced, sometimes with unknown effects on outcome and efficacy. The architecture of the National Tonsil Surgery Register in Sweden provides data well suited not only for detection of changes in clinical practice, but also for comparison of outcome between different techniques and instruments used for tonsil surgery.
One obvious limitation of registry data is the lack of randomization. However, the registry mirrors everyday clinical practice where decisions are made in accordance with the preferences of doctors and patients as well as the facilities and traditions of the clinic. Since only one clinic reported use of more than one type of radiofrequency instrument, the factor that determines which radiofrequency instrument that will be used at surgery is the catchment area of the given ENT clinic. Since the registry covers operations performed in all parts of Sweden, there is no reason to expect any systematic differences between the groups used in this study.
In a recently published editorial on tonsillotomy by Windfuhr and Werner [7], the authors suggest that intratonsillar procedures should be classified as either tonsillotomy (Class 1) or subtotal/intracapsular/partial tonsillectomy (Class 2). In Class 1 procedures, anatomical landmarks (anterior and posterior pillars) are used to decide how much tissue should be removed. In Class 2 procedures the aim is to remove most of the tonsil tissue (~90 %), with preservation of a rim of tissue along the inner surface of the capsule. In our material, most surgeries performed with Ellman Surgitron® or Sutter CURIS® would be classified as Class 1 according to Windfuhr since the original description of the method by Hultcrantz and Ericsson [8] and Hultcrantz [9] clearly describes the advantage of lessened risk for bleeding by keeping out of the pouch. When ArthroCare Coblation® is used, it is most often Class 2 that is performed; perhaps not with the purpose of removing 90 %, but intended to excavate the tonsil pouch as much as possible. However, the data in the registry do not allow for differentiation between Class 1 and 2 procedures. All radiofrequency instruments identified in our material can be used for both Class 1 and Class 2 procedures and the registry only has two options for the registration of surgical procedure: tonsillectomy or tonsillotomy. On the other hand, the significant difference in number of days on analgesics shown between ArthroCare Coblation® and the other options might be explained by the use of Class 1 with Ellman Surgitron® and Sutter CURIS® and Class 2 surgery with ArthroCare Coblation®, since Class 1 maintains a greater distance to the pain-sensitive tissues in the fossae and also results in a smaller surface area to heal.
In Sweden, data for the last decade have shown an increasing trend toward tonsillotomy and away from tonsillectomy [3]; tonsillotomy has now become the most frequently used surgical procedure in children with upper airway obstructive symptoms due to tonsil hypertrophy [3]. The current analysis has shown that radiofrequency-based techniques are used in 96 % of tonsillotomies performed and that instruments from three manufacturers (ArthroCare Coblation®, Ellman Surgitron®, and Sutter CURIS®) are used in more than 95 % of these operations. It is notable that microdebriders, which have been used in several studies on intratonsillar procedures [7], were not used for tonsillotomy in Sweden during 2009–2012.
The rate of both early (0.5 %) and late (1.2 %) bleedings in the present material is low with no significant differences between radiofrequency instruments. There were no differences between the radiofrequency instruments for either the number of postoperative infections (as measured by the number of antibiotic treatments) or the degree of symptom relief 6 months after surgery. A clear majority of the patients, >95 %, reported complete or almost complete symptom relief after tonsil surgery. As mentioned earlier, the only statistically significant difference found between the groups was the number of days on analgesics, with the Ellman Surgitron®/Sutter CURIS® group having 1 day shorter use than the ArthroCare Coblation® group. These results need to be replicated by other studies before one can draw any conclusions. However, the difference may be of great importance, both for the individual that experiences less pain and society with potentially less absence from school or work.
As concluded by Windfuhr and Werner [7], comparisons between tonsillotomy studies are complicated by the heterogeneity in study design, available raw data, and outcome measures. This is indeed true for studies that report bleeding rates and other data on complications and outcome variables in relation to a specific surgical instrument. One limitation of such studies is that they have in general included relatively small numbers of patients [10]. Even though our study is comparatively large, the statistical power is low due to the low rate of complications and the small differences between groups. For example, one of the main issues after tonsil surgery is the late postoperative bleeding. Assuming that the rates of late bleedings in our material are “the true rates”, 5,500 subjects would be needed in each group to give 80 % power to the conclusion that there is no statistically significant differences in late postoperative bleedings between the groups used. Even though we have a comparatively large number of subjects in the present study, the lack of power is still a limitation. Therefore, both the interpretation of the results and comparisons with other studies should be made with caution.
Even keeping the power question in mind, some comparisons with other studies can be made: in a systematic review of randomized controlled trials of pediatric tonsillotomy published by Walton et al. 2012 [10], data for postoperative bleedings after tonsillotomy were reported. Concerning postoperative bleeding, an “early” bleeding rate of 3/699 (0.4 %) and a “late” bleeding rate of 5/699 (0.7 %) were reported for tonsillotomy in general, rates which in general are comparable to our results. To our knowledge, thus far the present study is the largest on outcome after tonsillotomy in relation to specific radiofrequency instrument and may therefore serve as a measure for future studies.
There are several other instruments also available for tonsillotomy such as diathermy scissors, cold steel, electrocautery, and microdebriders. A tonsillotomy always leaves some amount of tonsil tissue in the pouch. How much tissue is left may affect both the efficacy and the risk for recurrent growth of tonsil tissue. The instrument that is used and the shape of the tonsils as well as the preference and skill of the surgeon may all affect how much tonsil tissue will be left. At the least, our data, including as it does, operations performed by surgeons with varying experience and skills, does not indicate that the radiofrequency instrument per se affects the results. With regard to recurrence, our data cannot thus far distinguish between differences in recurrence rate, but as the registry grows this analysis will be possible.
Conclusions
Nearly all pediatric tonsillotomies in Sweden are performed with a radiofrequency instrument. Instruments from three different manufacturers are used in 96 % of the operations. All radiofrequency tonsillotomies show low rates for both early and late postoperative bleedings and high rates of symptom relief 6 months after surgery. Our study could not find any differences in outcome or complications in relation to different radiofrequency equipment except for number of days on analgesics. Further studies are recommended to evaluate that difference.
References
Hessén Söderman AC et al (2011) Reduced risk of primary postoperative hemorrhage after tonsil surgery in Sweden: results from the National Tonsil Surgery Register in Sweden covering more than 10 years and 54,696 operations. Laryngoscope 121(11):2322–2326
Stalfors J et al (2012) Tonsil surgery efficiently relieves symptoms: analysis of 54,696 patients in the National Tonsil Surgery Register in Sweden. Acta Otolaryngol 132(5):533–539
Hultcrantz E et al (2012) Paradigm shift in Sweden from tonsillectomy to tonsillotomy for children with upper airway obstructive symptoms due to tonsillar hypertrophy. Eur Arch Otorhinolaryngol 270(9):2531–2536
CURIS®––Microsurgical Radiofrequency Generator. http://www.sutter-med.de/products/radiofrequency-generators/curis/technologie. Accessed 17 July 2013
Coblation® In Brief. http://www.arthrocare.com/our_technology/ot_coblation_explained.htm. Accessed 17 July 2013
The clinical significance of 4.0 MHz http://www.ellman.com/PDF/Press%20release/CC09021BVFa%20Why%204.0%20MHz%20Single.pdf Accessed 17 July 2013
Windfuhr JP, Werner JA (2013) Tonsillotomy: it’s time to clarify the facts. Eur Arch Otorhinolaryngol Aug 22 [Epub ahead of print]
Hultcrantz E, Ericsson E (2004) Pediatric tonsillotomy with the radiofrequency technique: less morbidity and pain. Laryngoscope 114(5):871–877
Hultcrantz E (2007) Surgical treatment of children with obstructive sleep apnea. In: Kountakis S, Önerci M (eds) Rhinologic and sleep apnea surgical techniques. Springer, Berlin, Heidelberg, pp 380–389
Walton J et al (2012) Systematic review of randomized controlled trials comparing intracapsular tonsillectomy with total tonsillectomy in a pediatric population. Arch Otolaryngol Head Neck Surg 138(3):243–249
Conflict of interest
The authors have no financial disclosures for this article. The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sunnergren, O., Hemlin, C., Ericsson, E. et al. Radiofrequency tonsillotomy in Sweden 2009–2012. Eur Arch Otorhinolaryngol 271, 1823–1827 (2014). https://doi.org/10.1007/s00405-013-2867-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-013-2867-4