Abstract
Tinnitus has been found to be modulated by stress and is also closely related to the emotional state and the limbic system. In the present study, we evaluated the diagnostic and clinical values of several stress hormones in a large number of tinnitus patients. This study included 344 patients with sensorineural tinnitus and 87 normal controls. A questionnaire about tinnitus was administered to the participants, and blood levels of norepinephrine (NE), epinephrine (Epi), a metabolite of serotonin (5-hydroxyindoleacetic acid, 5-HIAA) and cortisol were compared between groups. In results, the mean values of Beck’s depression inventory (BDI), Brief Encounter Psychosocial Instrument (BEPSI), NE, and 5-HIAA levels were higher in the tinnitus group, although there was no statistical significance. But, the proportion of participants with elevated 5-HIAA was significantly higher in the tinnitus group (21.8 vs. 8.0 %, P < 0.05), and the 5-HIAA level significantly correlated with the duration of tinnitus, NE and cortisol. Elevated stress-related hormones, as well as hearing loss, BDI, and BEPSI were the most related factors with tinnitus in multiple regression test with age adjustment. However, levels of stress-related hormones did not correlate with subjective measures including BDI, BEPSI and severity of tinnitus. In conclusion, blood stress hormones seemed to have some diagnostic and clinical value in patients with tinnitus, and serotonin is supposed to be the most important hormone in tinnitus. Further studies about the values of stress and stress hormones in tinnitus patients may lead to new approaches regarding diagnosis and clinical management of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tinnitus is a ringing or buzzing sound in the ears or head, which cannot be attributed to an external source. For an estimated 5–15 % of the population, tinnitus can become chronic and detrimental to the quality of life. The proportion of affected individuals is increasing with the expanding proportion of aged individuals [1]. Despite the high prevalence of tinnitus, there is little consensus regarding its neurophysiological etiology. Recently, several mechanisms involving brain plasticity have been proposed and most researchers agree that tinnitus can be linked to changes at one or more points along the peripheral and central auditory pathways [2–4].
The severity of tinnitus is reported by sufferers to be exacerbated by stress [5]. Two major systems mediate most components of the stress response [6]. The first is the hypothalamic-pituitary-adrenal (HPA) pathway, which stimulates the adrenal cortex to release glucocorticoids such as cortisol and corticosterone into the blood [7]. The second is the sympathetic-adrenomedullary system, which influences the stress response by two different pathways working in parallel. One pathway contains nerve endings that trigger the release of epinephrine (Epi) from adrenal medulla chromaffin cells into the bloodstream. The other pathway comprises sympathetic nerve endings that supply essentially every organ in the body with norepinephrine (NE) [8]. Under stress, the synthesis and release of serotonin (5-hydroxytryptamine, 5-HT) also increases in various brain areas, and activation of the HPA axis plays a role in this process [9, 10]. 5-HT transmission is related to a large variety of brain functions, forms a major modulatory network within the sensory system, and controls filtering of auditory information [11]; therefore, 5-HT dysfunction is presumably involved in tinnitus development. In the present study, we measured plasma levels of stress-related hormones such as cortisol, Epi, NE, and metabolites of serotonin (5-Hydroxyindoleacetic acid, 5-HIAA) in tinnitus patients and evaluated their clinical significance.
Until now, there have been few reports exploring the link between tinnitus and stress-related hormones despite well-established theoretical suggestions [12, 13]. In Meniere’s disease and sudden deafness with tinnitus, there are supports that exacerbation of symptoms is preceded by episodes of stress, or is linked with higher levels of stress hormones or are associated with higher number and greater stressfulness of events [14, 15]. Recently, a study displayed a reduced cortisol response to psychosocial stress of tinnitus sufferers, in comparison with healthy controls, and the authors suggests an anomaly of the HPA axis in tinnitus suffers [16]. These studies suggest that stress levels may modulate tinnitus.
Other hormones related to sympathetic fibers have been found to affect afferent activity in the cochlea. [17] Following the provocation of emotional stress in guinea pigs, plasma catecholamines increased and there was a slight elevation of the compound action potential (CAP) threshold and a decrease in the input/output function [18]. Noise exposure is known to be a stressor associated with increased plasma NE in awake animals [19].
In relation to 5-HT, which is a major modulator of sensory systems, it has been shown, in rats, that 5-HT activation in sensory neurons increases with age, and several authors have suggested that the perception of tinnitus could be linked to 5-HT dysfunction at one or more levels in the central nervous system [20].
Despite theoretical and experimental suggestions of a link between tinnitus and stress hormones, there are very few studies that measure stress hormones in tinnitus sufferers. Clinically, we have previously observed significantly elevated stress scores in tinnitus sufferers, as compared to normal controls [21]. In this study, we evaluated the diagnostic and clinical values of several stress hormones in a large number of tinnitus patients.
Materials and methods
A total of 344 participants with tinnitus were evaluated by means of history, physical examination, audiological study, and questionnaires between January 2010 and December 2010 (tinnitus group). All the patients in this group had sensorineural tinnitus. Patients who had middle ear disease or retrocochlear lesions were excluded. Healthy people (n = 89) who did not have tinnitus were also included as a control group.
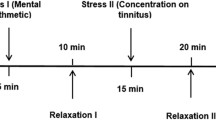
In the tinnitus group, tinnitus questionnaires, including a visual analog scale (VAS) of tinnitus annoyance, awareness, loudness and effect on life and Tinnitus Handicap Inventory (THI) suggested by Newman [22], were completed; an audiological evaluation with pure tone averages (PTA) was conducted, and the results were averaged for standard speech frequencies at 500–1,000–2,000 Hz. The stress levels of the patients with tinnitus and control participants were evaluated using the Korean version of the Brief Encounter Psychosocial Instrument (K-BEPSI) [23], which includes five items that are scored 1–5. Symptoms of depression using Beck’s depression inventory (BDI) [24], which was applied to Korean language, were also assessed in both tinnitus and control participants. The stress hormones that we measured in the blood were NE, Epi, 5-HIAA, and cortisol. Catecholamine 2F (NE and Epi) levels were measured by a commercially available Bio Rad PCAT Kit (CA, USA). 5-HIAA, a metabolite of 5-HT, was determined by specific ELISA using a commercial kit from Wakosil (Wakosil-II; Osaka, Japan). Cortisol was measured by specific radioimmunoassay using a kit from Beckman Coulter (Cortisol RIA kit; Shizuoka, Japan). Blood sampling was conducted between 9 and 11 a.m. and our reference levels of these hormones are as follows: Epi <120 pg/ml, NE between 100 and 410 pg/mL, 5-HIAA beween 1.8 and 6.1 ng/mL, and cortisol (in the morning) between 9.41 and 26.06 μg/dl. We compared clinical and psychological features as well as stress hormone levels between the tinnitus group and the normal controls. For statistical and descriptive analysis, Student t tests, Chi-square test, partial correlation test, and multiple logistic regression tests were performed using an SAS program (version9.3, Cary, NC, USA). This study was approved by the institutional review board of Seoul St. Mary’s Hospital (KC11RISI0252).
Results
The mean age of tinnitus sufferers was rather higher than that of the control group (53.8 ± 14.2 vs. 49.5 ± 11.8 years; P < 0.05). The male to female ratio ranged from 167 to 177 in the tinnitus group and 33–54 in the control group (P > 0.05). Mean depression scores and stress scores were slightly higher in the tinnitus group, but there was no statistical significance. Levels of blood stress hormones (NE, Epi, 5-HIAA, and cortisol) ranged widely with huge standard deviation. Although the mean blood levels of NE and 5-HIAA were slightly elevated in the tinnitus group, as compared to the control group, the difference was not statistically significant (P > 0.05) (Table 1).
For further evaluation of the association between tinnitus, NE, and 5-HIAA, we investigated the proportions of participants with abnormally elevated NE or 5-HIAA in both tinnitus and control groups. Abnormally elevated NE or 5-HIAA was observed in 150/344 (43.6 %) of tinnitus sufferers and was found to be significantly more common among those with tinnitus than the controls (24/87, 27.6 %) (P < 0.05), and abnormally elevated 5-HIAA was also more frequently observed in tinnitus sufferers (21.9 %) than in control participants (8.1 %) (P < 0.01) (Fig. 1). However, the proportion of participants with abnormally elevated NE was not significantly different between the tinnitus (29.5 %) and control (22.9 %) groups, which suggests that the higher proportion of abnormally elevated NE or 5-HIAA for participants in the tinnitus group was mostly due to their elevated 5-HIAA.
Proportion of individuals with elevated blood stress hormones in the tinnitus group and control group. Abnormally elevated NE and 5-HIAA were observed in 150/344 (43.6 %) of tinnitus patients and were found to be significantly more common in those with tinnitus than in the control participants 24/87 (27.6 %) (P < 0.05). Abnormally elevated 5-HIAA was more frequently observed in the tinnitus group (P < 0.01)
According to the above results, we postulated a grading system according to elevated stress hormones: no elevation as grade 0, elevation of NE as grade 1, elevation of 5-HIAA as grade 2 and, lastly, elevation of both NE and 5-HIAA as grade 3. We then compared these values with clinical data of tinnitus sufferers and evaluated whether NE and 5-HIAA are good clinical markers in them. As seen in Fig. 2, participants with elevated NE and 5-HIAA seemed to have a longer duration of tinnitus than participants with normal stress hormone levels, although there was no statistical difference. Moreover, tinnitus sufferers with abnormally elevated NE and 5-HIAA tended to have higher tinnitus scores with regard to loudness, awareness, annoyance and effect on daily life although there were no significant differences between groups (Fig. 3). Multiple regression tests with age adjustment (Table 2) showed that hearing loss, BDI, BEPSI and elevated stress hormones were the most related factors for tinnitus and, in this test, we also used our postulated grades of abnormally elevated stress hormones. Lastly, we conducted a partial correlation test with age adjustment, because 5-HT levels could increase with aging [25]. In Table 3, VAS scores, THI, hearing level, BDI, and BEPSI were well correlated with each other, but stress hormone levels did not correlate with that, and 5-HIAA and cortisol were only correlated with the duration of tinnitus. There were some correlations between levels of stress-related hormones.
Discussion
The phantom sound of tinnitus is strongly associated with emotional stress, anxiety and depression [26, 27]. In relation to stress, tinnitus is a chronic stressor that is similar to other chronic diseases [28]. When tinnitus becomes chronic, individuals catastrophize their coping resources and begin to experience chronic negative emotions accompanying the tinnitus. Recent research using scalp electroencephalography and low-resolution electromagnetic tomography in 27 adults with tinnitus revealed that tinnitus related distress is associated with emotion-related areas, such as the amygdala, nucleus accumbens-ventral tegmental area, parahippocampal gyrus, and posterior subcallosal anterior cingulate cortex [29]. In other studies about stress and tinnitus, findings that some individuals with tinnitus have evidence of activation of the dorsal medial thalamus the neurons of which project directly to the lateral nucleus of the amygdala was shown, and that such abnormal activation of the extralemniscal auditory pathways can explain stress-related signs in some individuals with tinnitus [30, 31].
In turn, stress may contribute to the development or aggravation of tinnitus. A Swedish study including 9,756 participants showed that the participants with various stressors, e.g., occupational, poorer self-rated health, long-term illness, and poorer sleep quality had a higher prevalence of hearing problems including tinnitus [32].
Depression is also closely related to tinnitus as a stressor. Prevalence rates of depressive disorders in tinnitus patients range from 14 % up to 80 %, according to the type of clinical interview (self-reporting or standardized clinical interview) and operationalization criteria (DSM-IV vs. ICD-10) [26]. Stress describes a transient aversive state, interfering with a person’s ability to adequately adapt to stressors; in contrast, depression is a rather constant emotional state [27]. Joos et al. [27] recently revealed, using standardized low-resolution brain electromagnetic tomography, that stress and depression have distinct neural circuits in the brain. However, stress is an important factor in depression, and stress-induced structural changes in brain regions such as the hippocampus have clinical ramifications for disorders such as depression, post-traumatic stress disorder and individual differences in the aging process [33, 34]. In our study, there were notable associations between BDI, BEPSI and the severity of tinnitus (Table 3), and a multiple regression study also showed similar results (Table 2).
Table 3 shows that hearing loss was well correlated with the severity of tinnitus as well as BDI and BEPSI. And poor hearing, of course, was also a most related factor for tinnitus, as seen in Table 2. According to our study results, hearing loss and tinnitus are closely related, as previously known, and stress and depression are also closely associated with hearing loss and tinnitus. Interestingly, of the four stress hormones measured in this study, 5-HIAA was the most frequently elevated in the tinnitus group, as compared to the control group.
Two consecutive studies [16, 35] have revealed increased basal cortisol release and blunted cortisol in response to social stress in tinnitus patients. However, they later found that the blunted cortisol responses to stress are much more robust than the subtle basal cortisol change. Our results did not show any difference in basal cortisol between tinnitus and control groups. Also, the basal cortisol level did not correlate with the severity of tinnitus, BDI, and BEPSI scores. According to our results, the basal activity of the HPA axis in tinnitus patients does not seem to be elevated above that of normal participants. For this study, we removed bias due to circadian rhythm by randomly measuring the cortisol level of both groups in the morning, and we thought comparing of mean plasma cortisol level between both groups would be available.
Our study differed from other studies on this topic by the relatively short duration of tinnitus of our participants, 33.8 ± 47.7 months, whereas that of a former study was 5.5 years [35]. Considering our results of good correlation between plasma cortisol and 5-HIAA level and duration of tinnitus, difference of duration of tinnitus in both studies might be the cause of different result. Besides that, we also think investigations of cortisol response to acute stress could be more important to prove dysfunction of HPA axis in tinnitus patients, than just measuring basal cortisol levels. Further investigations are needed to confirm that.
In investigations of catecholamine release, the mean level of plasma NE was slightly higher in the tinnitus group, as compared to the control group, with no statistical significance. We initially assumed that plasma NE or Epi were good indicators for stress levels in tinnitus patients. However, we found no statistically significant difference in plasma NE or Epi levels between the tinnitus and control groups. Variable stressful conditions in the control group could partially explain this negative result. Even though there was no difference between the two groups, we can use abnormally elevated NE or Epi levels in the plasma of the patients with tinnitus as an indicator of their stress, a factor that should be taken into account during patient counseling.
Serotonin (5-hydroxytryptamine, 5-HT) is a neurotransmitter that controls many brain functions. Since 5-HT transmission forms a major modulatory network within sensory systems and filters auditory information [11], 5-HT dysfunction has been thought to contribute to tinnitus development. Under stress, the synthesis and release of 5-HT also increases in various brain areas, and activation of the HPA axis plays a role in this process [9, 10]. Our study results showed higher proportions of participants with abnormally elevated plasma 5-HIAA in the tinnitus group than in the control group, and this could be explained by increased turnover of 5-HT in the brain of tinnitus sufferers. A recent study of Mitani et al. [34]. showed an increased plasma 5-HIAA level in depressed patients. They explained their results by increased 5-HT turnover in brain, which resulted from a compensatory action to act as an antidepressant and protect the patient against stress. We can also assume that the increased 5-HT turnover in patients with tinnitus shown in this study was a response to the stress of tinnitus. Considering that tinnitus is a chronic disabling condition, it is possible that the increased plasma 5-HIAA level is a representative blood indicator for chronic stress due to tinnitus. Therefore, tinnitus patients with an abnormally elevated 5-HIAA should focus on treating their stress levels.
Lastly, as a weakness of our study, the results show a large inter-individual variability in biological measurements among tinnitus patients. Because our study involves more than 300 participants, their heterogeneity in tinnitus severity might effect on this variability. Further study considering this may bring out more precise relation between stress hormones and tinnitus.
Conclusion
We conducted this relatively large case-control study including over three hundred participants with tinnitus, and found that plasma 5-HIAA is more frequently elevated in tinnitus sufferers, and that its levels are correlated to some degree with the duration of tinnitus and elevation of other stress hormones. Elevation of stress-related hormones, as well as hearing loss, BDI, and BEPSI were the most related factors with tinnitus in multiple regression tests. Subjective measures about tinnitus, stress, and depression were well correlated with each other, and also well correlated with hearing level.
This study identified clinical and diagnostic value in measuring stress-related hormones in tinnitus sufferers. We believe that various plasma stress hormones could be used to monitor the stress levels of tinnitus sufferers, and 5-HIAA seems to be the most valuable stress hormone for this purpose.
References
Heller AJ (2003) Classification and epidemiology of tinnitus. Otolaryngol Clin North Am 36(2):239–248
Eggermont J, Roberts L (2004) The neuroscience of tinnitus. Trends Neurosci 27:876–882
Jastreboff PJ (1990) Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res 8(4):221–254
Moller AR (2003) Pathophysiology of tinnitus. Otolaryngol Clin North Am 36:249–266
Nodar RH (1996) C.A.P.P.E.-a strategy for counseling tinnitus patients. Int Tinnitus J 2:111–113
Fuchs E, Flugge G (2003) Chronic social stress: effects on limbic brain structures. Physiol Behav 79(3):417–427
Mason JW (1968) A review of psychoendocrine research on the pituitary-adrenal cortical system. Psychosom Med 30(5 Suppl:):576–607
Mason JW (1968) A review of psychoendocrine research on the sympathetic-adrenal medullary system. Psychosomatic medicine 30(5 Suppl:):631–653
Lanfumey L, Mongeau R, Cohen-Salmon C, Hamon M (2008) Corticosteroid-serotonin interactions in the neurobiological mechanisms of stress-related disorders. Neurosci Biobehav Rev 32(6):1174–1184. doi:10.1016/j.neubiorev.2008.04.006
Inoue T, Tsuchiya K, Koyama T (1994) Regional changes in dopamine and serotonin activation with various intensity of physical and psychological stress in the rat brain. Pharmacol Biochem Behav 49(4):911–920
Simpson JJ, Davies WE (2000) A review of evidence in support of a role for 5-HT in the perception of tinnitus. Hear Res 145(1–2):1–7
Alpini D, Cesarani A (2006) Tinnitus as an alarm bell: stress reaction tinnitus model. ORL J Otorhinolaryngol Relat Spec 68(1):31–36. doi:10.1159/000090488 discussion 36–37
Horner KC (2003) The emotional ear in stress. Neurosci Biobehav Rev 27(5):437–446
Horner KC, Guieu R, Magnan J, Chays A, Cazals Y (2001) Prolactinoma in some Meniere’s patients-is stress involved? Neuropsychopharmacology 26:135–138
Schmitt C, Patak M, Kroner-Herwig B (2000) Stress and the onset of sudden hearing loss. Int Tinnitus J 6:41–49
Hebert S, Lupien SJ (2007) The sound of stress: blunted cortisol reactivity to psychosocial stress in tinnitus sufferers. Neurosci Lett 411(2):138–142. doi:10.1016/j.neulet.2006.10.028
Spodendlin H, Lichtensteiger W (1966) The adrenergic innervation of the labyrinth. Acta Otolaryngol 61:423–434
Muchnik C, Hildesheimer M, Rubinstein M (1980) Effect of emotional stress on hearing. Arch Otorhinolaryngol 228(4):295–298
Muchnik C, Rosenthal T, Peleg E, Hildesheimer M (1998) Stress reaction to intense sound exposure under different arousal levels in guinea pigs. Acta Otolaryngol 118:646–650
Cransac H, Peyrin L, Cottet-Emard JM, Farhat F, Pequignot JM, Reber A (1996) Aging effects on monoamines in rat medial vestibular and cochlear nuclei. Hear Res 100(1–2):150–156
Park S, Park DS, Park KH, Kim JH, Han MA, Yeo SW (2007) Measurement of stress, anxiety and depression in the patients with tinnitus and their clinical significance. Korean J Audiol 11:21–28
Newman CW, Jacobson GP, Spitzer JB (1996) Development of the tinnitus handicap inventory. Arch Otolaryngol Head Neck Surg 122(2):143–148
Huh B, Yim J, Bae J, Choi S, Kim S, Hwang H (1996) The validity of modified korean-translated BEPSI (brief encounter psychosocial instrument) as instrument of stress measurement in outpatient clinic. J Korean Acad Fam Med 17(1):42–53
Beck AT, Steer RA, Brown GK (1996) BDI-II, Beck depression inventory : manual. 2nd edn. Psychological Corp. Harcourt Brace, San Antonio, Tex. Boston
Murakami H, Bessinger K, Hellmann J, Murakami S (2008) Manipulation of serotonin signal suppresses early phase of behavioral aging in Caenorhabditis elegans. Neurobiol Aging 29(7):1093–1100. doi:10.1016/j.neurobiolaging.2007.01.013
Langguth B, Landgrebe M, Kleinjung T, Sand GP, Hajak G (2011) Tinnitus and depression. World J Biol Psychiatry 12(7):489–500. doi:10.3109/15622975.2011.575178
Joos K, Vanneste S, De Ridder D (2012) Disentangling depression and distress networks in the tinnitus brain. PLoS ONE 7(7):e40544. doi:10.1371/journal.pone.0040544
Malouff JM, Schutte NS, Zucker LA (2011) Tinnitus-related distress: a review of recent findings. Curr Psychiatry Rep 13(1):31–36. doi:10.1007/s11920-010-0163-1
Vanneste S, Plazier M, der Loo E, de Heyning PV, Congedo M, De Ridder D (2010) The neural correlates of tinnitus-related distress. Neuroimage 52(2):470–480. doi:10.1016/j.neuroimage.2010.04.029
Moller AR, Moller MB, Yokota M (1992) Some forms of tinnitus may involve the extralemniscal auditory pathway. Laryngoscope 102(10):1165–1171. doi:10.1288/00005537-199210000-00012
Møller AR (2010) Textbook of tinnitus. Springer
Hasson D, Theorell T, Wallen MB, Leineweber C, Canlon B (2011) Stress and prevalence of hearing problems in the Swedish working population. BMC public health 11:130. doi:10.1186/1471-2458-11-130
McEwen BS (2000) The neurobiology of stress: from serendipity to clinical relevance. Brain Res 886(1–2):172–189
Mitani H, Shirayama Y, Yamada T, Kawahara R (2006) Plasma levels of homovanillic acid, 5-hydroxyindoleacetic acid and cortisol, and serotonin turnover in depressed patients. Prog Neuropsychopharmacol Biol Psychiatry 30(3):531–534. doi:10.1016/j.pnpbp.2005.11.021
Hebert S, Paiement P, Lupien SJ (2004) A physiological correlate for the intolerance to both internal and external sounds. Hear Res 190(1–2):1–9. doi:10.1016/S0378-5955(04)00021-8
Conflict of interest
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, DK., Chung, D.Y., Bae, S.C. et al. Diagnostic value and clinical significance of stress hormones in patients with tinnitus. Eur Arch Otorhinolaryngol 271, 2915–2921 (2014). https://doi.org/10.1007/s00405-013-2785-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-013-2785-5