Abstract
The purpose of this study was to investigate the effectiveness of intratympanic steroids in patients with idiopathic sudden sensorineural hearing loss who did not respond to initial systemic steroid therapy. This retrospective study involved 51 patients, who did not respond to systemic steroids as a first-line treatment. Initial systemic steroid therapy consisted of administration of methylprednisolon intravenously (250 mg) at the first day and followed by orally (1 mg/kg) tapering for 14 days. Twenty-one patients accepted intratympanic treatment, and the remaining 30 patients who refused intratympanic treatment were evaluated as the control group. Steroids (dexamethasone drops, 1 mg/mL) were administered through a ventilation tube. Hearing was assessed immediately before treatment and 2 months after treatment. Recovery of hearing was defined as an improvement of >20 dB in the pure tone average. We tested 250, 500, 1,000, 2,000, 4,000, and 8,000 Hz frequencies for the pure tone audiometric evaluation. Statistically Student’s t test, Mann–Whitney U test, Chi-squared and Fisher’s exact tests were used. The pure tone average improved in 47.6 % of the intratympanic group and in 10 % of the control group (p = 0.002), with pure tone average improvements of 19.9 ± 16.5 and 4.76 ± 9.6 dB in the intratympanic and control groups, respectively. When the hearing threshold at each frequency was analyzed, improvements at all frequencies were significantly greater in the intratympanic steroid group when compared with the control group (p < 0.01). Intratympanic steroid administration is an effective therapy for sudden sensorineural hearing loss in patients, who are refractory to primary systemic steroid therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sudden sensorineural hearing loss (SSHL) is defined as hearing loss of >30 dB at three consecutive frequencies within a 72-h period. With an incidence of 5–20/100,000, SSHL represents approximately 1 % of all cases of sensorineural hearing loss [1]. Viral, vascular, and autoimmune pathologies have been considered as etiologies [2]. Although a specific factor has been detected in a small number of cases, the remaining cases are accepted as idiopathic sudden sensorineural hearing loss (ISSHL) [3].
Many different drugs have been used to treat ISSHL, but systemic corticosteroids are the only agents with proven effectiveness [4]. The spontaneous rate of recovery from ISSHL ranged from 32 to 65 % in various studies; with systemic corticosteroid therapy, the recovery rate reportedly increased to 49 to 89 % [5]. The mechanism of steroid action in the inner ear has not been fully clarified, and the optimal dose of steroids is unknown [6]. Nevertheless, higher steroid doses in the inner ear are thought to improve hearing [6].
Owing to the absence of alternative therapies and the potential side effects of long-term systemic administration of high-dose steroids, intratympanic administration of steroids has gained popularity for patients who do not respond to standard therapy. When steroids are directly administered into the middle ear, allowing perfusion into the inner ear via the round window, systemic side effects are limited, and experimental animal studies have shown that higher steroid levels are achieved in both the endolymph and perilymph compared with levels achieved by systemic use [7, 8].
This study evaluated the efficacy of local steroid therapy in patients diagnosed with ISSHL, who did not respond to standard therapy.
Methods
The records and hearing test results of patients with SSHL who were hospitalized at the Otorhinolaryngology Clinic of Bakirkoy Sadi Konuk Research and Training Hospital (Istanbul, Turkey) between December 2006 and June 2010 and who did not respond to primary therapy with systemic steroids were analyzed retrospectively. Primary steroid therapy consisted of administration of methylprednisolon intravenously (250 mg) at the first day and followed by orally (1 mg/kg) tapering for 14 days. Failure to respond was defined as an improvement in the pure tone average (PTA at 500, 1,000, 2,000, and 4,000 Hz) of <20 dB on day 14 of primary therapy. The study protocol was approved by the ethics committee of the same hospital.
Inclusion criteria were the following: SSHL of at least 30 dB at three or more consecutive frequencies in fewer than 3 days, unilateral hearing loss, age >18 years, no history of treatment at another center, no identified etiological factors to explain the hearing loss, no history of a previous otologic disease or operation on the affected ear, no history of previous chemotherapy or radiotherapy, admission for first-line therapy within 30 days after the onset of hearing loss, no response or <20-dB improvement in PTA within 14 days of systemic oral steroid therapy, and the ability to complete the treatment protocol of our clinic.
A total of 51 patients, who were refractory to systemic steroid therapy and, who met the other inclusion criteria were included in the study. All patients were informed about the additional therapy in terms of complications and advantages. The study group consisted of 21 patients who provided informed consent for treatment with intratympanic steroids in addition to systemic steroids. The control group included 30 patients who refused additional therapy after systemic steroid therapy.
Intratympanic steroid administration
For intratympanic therapy, a ventilation tube (inner diameter, 1.14 mm) was placed in the postero-inferior part of the tympanic membrane under local anesthesia. The patient was placed in the supine position with the head tilted about 30–40° toward the healthy side and was instructed to remain in the supine position for about 20–30 min and to avoid swallowing after perfusion. The patients were told to warm the dexamethasone (Onadron 1 mg/mL; I.E. Ulagay) for 5 min at body temperature, and to insert five drops of the drug through the external auditory canal four times a day. The participants were told to pump the tragus to improve flow into the middle ear. Patients were examined daily to check transmission of the drug from the tube and to avoid potential complications. Patients were instructed to avoid getting water in their ears during this period. The treatment continued for 2 weeks.
Hearing assessment
Audiologic assessment was performed using an Interacoustics AC40 clinical audiometer. The PTA on day 14 after completion of systemic steroid therapy was accepted as the initial audiometric value. The PTA evaluated at the second month after that date was the final audiometric value. Improvement was defined as a change of >20 dB. The improvement at each frequency (250, 500, 1000, 2,000, 4,000, and 8,000 Hz) was also determined.
Statistical analysis
The Number Cruncher Statistical System 2007 (NCSS, Kaysville, UT, USA) and Power Analysis and Sample Size 2008 Statistical Software (NCSS) were used for statistical analyses. Student’s t test was used for intergroup comparisons of normally distributed parameters, and descriptive statistical methods (mean, standard deviation) were used to compare quantitative data. The Mann–Whitney U test was used to compare initial and final audiometric PTAs and values for each frequency. Qualitative data were compared using the Chi-squared and Fisher’s exact tests. Significance was indicated by p < 0.05.
Results
The mean age of the 51 patients in the study was 43.75 ± 16.19 years (range 18–68 years). Of the participants, 54.9 % (n = 28) were men and 45.1 % (n = 23) were women. Twenty-one patients who received intratympanic steroids were in the study group, and the remaining 30 patients were in the control group. The descriptive characteristics of the two groups are given in Table 1. The two groups did not differ significantly in terms of age, gender, or other descriptive characteristics (p > 0.05).
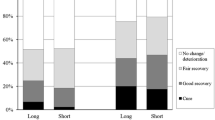
The mean initial PTA values were 92.38 ± 23.67 and 89.07 ± 23.61 dB in the intratympanic steroid group and control group, respectively, and did not differ significantly (p > 0.05). Improvement was detected in 10 (47.6 %) of the 21 patients who received intratympanic steroid perfusion and in only three (10 %) of the 30 control patients. The improvement rate was significantly higher in the intratympanic group (p < 0.01) (Table 2; Fig. 1).
The PTA of patients who received intratympanic steroids improved by 19.9 ± 16.5 dB, and the PTA of patients in the control group improved by 4.76 ± 9.6 dB; the difference in the improvement was significant (p < 0.01) (Table 3; Fig. 2). In addition, in Table 4, we can see the averages of pure-tone audiometric values at each separate frequency. When improvements at each frequency on pure tone audiograms were analyzed separately for each group, both groups showed better improvements at the lower frequencies than at the higher frequencies (Fig. 3). When the groups were compared, the improvements at all frequencies were greater in the study group than in the control group (p < 0.01).
No complications requiring discontinuation of the therapy were detected in any patients. Brief, mild vertigo occurred in three patients during therapy. Otitis media was observed in two patients after therapy, and this was treated with systemic antibiotics. One patient developed a persistent tympanic membrane perforation and was successfully treated with a paper patch. Otomycosis was not observed in any patient.
Discussion
The etiopathogenesis and treatment of SSHL remains controversial. The most commonly considered theories for the etiopathogenesis are viral infections, vascular events, autoimmune causes, and membrane rupture of the labyrinth [3, 9]. A specific factor can be detected in approximately 10 % of cases [3]. Different combination therapies, including systemic steroids, have been used for treatment. Nevertheless, about 20–50 % of patients do not benefit from treatment. Thus, additional therapies are needed.
In recent studies, intratympanic steroid therapy has been shown to provide additional hearing in about 38–53 % of patients who had not benefited from systemic steroid therapy [10–12]. Success rates of 12–100 % have been reported for treatment using intratympanic steroid therapy [13, 14]. The success rate may vary depending on the steroid, application method, dosage, previous therapies, and time of therapy initiation. Some researchers have used this treatment as salvage therapy in patients who are refractory to systemic steroids, and others have used it as a primary therapy. In some studies, an improvement of 10 dB in the mean PTA was considered a success; in other studies, a 50 % improvement in the PTA was accepted as the success criterion. In our clinic, intratympanic steroid therapy is used as salvage therapy, with a 20-dB improvement in the PTA as the success criterion.
Some researchers have advocated that the benefit obtained from intratympanic steroid administration is related to the spontaneous recovery of SSHL or the delayed effects of systemic steroids. However, in studies that included control groups, intratympanic steroid therapy resulted in better outcomes compared with the control group [10, 11, 15, 16]. In our study, 51 patients who were refractory to primary therapy with systemic steroids were analyzed. Improvement was detected in 10 (47.6 %) of the 21 patients who received intratympanic steroids (mean PTA gain, 19.9 ± 16.5 dB) and in 3 (10 %) of the 30 patients in the control group (mean PTA gain, 4.76 ± 9.6 dB). The degree and rate of improvement were significantly better in the intratympanic steroid group (p < 0.01).
Improvement rates were also evaluated according to frequencies in the present study. Improvements at all frequencies were significantly greater in the intratympanic steroid group when compared with the control group (p < 0.01). In each group, improvements were better at the lower frequencies than at the higher frequencies. In experimental studies investigating the cochlear pharmacokinetics of steroids perfused into the middle ear, markers showing the cochlear distribution of the drug were at higher concentrations near the round window (basal turn) compared with the apical turn [17, 18]. Based on this result, patient responses to this therapy would be expected to be better at high frequencies. However, in the present study, low-frequency hearing loss (cases of apical turn involvement) showed improvement at a higher rate than high-frequency hearing loss in both groups. Similarly, in studies by She et al. [16], Choung et al. [12], and Gouveris et al. [19], better improvement was obtained at lower frequencies in patients who received intratympanic steroids. According to one theory, variations in the cochlear distribution of glucocorticoid receptor subtypes may account for this [20]. Another theory proposes that the basal part of the cochlea is more susceptible to trauma and free oxygen radical-related damage [21]. In a study supporting the latter theory, internal and external ciliary cells in the basal part of the cochlea, in contrast to the apical cells, developed ultrastructural anomalies following injury that could lead to severe or total ischemia [22]. This condition may explain why the effect of intratympanic steroids is more limited in patients with high-frequency hearing loss.
Methods for perfusing steroids into the middle ear include injection with a needle, myringotomy, and instillation via a ventilation tube inserted into the tympanic membrane or via a round window microcatheter (MicroWick) [23–26]. The best method is unclear because studies on this issue have included limited numbers of patients. In addition, the steroid type, concentration, dosage, and duration of use have not yet been standardized. In a study by Silverstein et al. [27] involving patients with Meniere’s disease, different steroid types were administered via different methods, and no one method was shown to be superior.
Injection with a fine needle is the most frequently used method. Although this is an easy method, it does not seem safe. Furthermore, the steroid does not remain in the middle ear for very long because it passes through the Eustachian tube. As use of this method has been limited, its effects on the pharmacokinetics of the steroid are unknown [10–12]. Air in the middle ear can also lead to problems. In our clinic, the preferred method is administration of drugs four times daily for a prolonged period via instillation through a ventilation tube, because of the ease of application.
Another issue of debate is the selection of the steroid to be used. In an animal study by Parnes et al. [7] methylprednisolone remained at the highest concentration in the perilymph for the longest period. However, methylprednisolone injection causes a burning sensation in the ear and throat, reducing patient compliance and possibly leading to discontinuation of therapy. Dexamethasone is among the most potent anti-inflammatory steroids, although the effect of dexamethasone in the perilymph lasts only about 6 h, in contrast to 24 h for methylprednisolone [7, 28]. Thus, in our study, we told to patients to self-administer five drops of dexamethasone (Onadron 1 mg/mL; İ.E. Ulagay) every 6 h, and patients were called daily to follow up on complications and drug perfusion. The frequent administration of intratympanic steroids for a prolonged period (14 days) distinguishes our study from other intratympanic studies.
In conclusion, intratympanic steroid administration may be an alternative therapy in patients, who are refractory to primary systemic steroid therapy. We consider that frequent local administration of the steroid for a prolonged period is important in successful treatment. Randomized controlled trials with larger numbers of patients are needed before recommending the routine use of intratympanic steroids in patients with refractory ISSHL.
References
Filipo R, Covelli E, Balsamo G, Attanasio G (2010) Intratympanic prednisolone therapy for sudden sensorineural hearing loss: a new protocol. Acta Otolaryngol 130(11):1209–1213
Lautermann J, Sudhoff H, Junker R (2005) Transtympanic corticoid therapy for acute profound hearing loss. Eur Arch Otorhinolaryngol 262(7):587–591
Hughes GB, Freedman MA, Haberkamp TJ, Guay ME (1996) Sudden sensorineural hearing loss. Otolaryngol Clin North Am.Rev 29(3):393–405
Wilson WR, Byl FM, Laird LN (1980) The efficiency of steroids in the treatment of idiopathic sudden hearing loss. A double-blind clinical study. Arch Otolaryngol 106(12):772–776
Moskowitz D, Lee KJ, Smith HW (1984) Steroid use in idiopathic sudden sensorineural hearing loss. Laryngoscope 94(5 Pt 1):664–666
Kakehata S, Sasaki A, Oji K et al (2006) Comparison of intratympanic and intravenous dexamethasone treatment on sudden sensorineural hearing loss with diabetes. Otol Neurotol 27(5):604–608
Parnes LS, Sun AH, Freeman DJ (1999) Corticosteroid pharmacokinetics in the inner ear fluids: an animal study followed by clinical application. Laryngoscope 109(7 Pt 2):1–17
Chandrasekhar SS (2001) Intratympanic dexamethasone for sudden sensorineural hearing loss: clinical and laboratory evaluation. Otol Neurotol 22(1):18–23
Schuknecht HF, Kamura RS, Nougal PM (1973) The pathology of sudden deafness. Acta Otolaryngol 76(2):75–97
Xenellis J, Papadimitriou N, Nikolopoulos T et al (2006) Intratympanic steroid treatment in idiopathic sudden sensorineural hearing loss: a control study. Otolaryngol Head Neck Surg 134(6):940–945
Ho GM, Lin HC, Shu MT, Yang CC, Tsai HT (2004) Effectiveness of intratympanic dexamethasone injection in sudden deafness patients as salvage treatment. Laryngoscope 114(7):1184–1189
Choung YH, Park K, Shin YR, Cho MJ (2006) Intratympanic dexamethasone injection for refractory sudden sensorineural hearing loss. Laryngoscope 116(5):747–752
Battista RA (2005) Intratympanic dexamethasone for profound idiopathic sudden sensorineural hearing loss. Otolaryngol Head Neck Surg 132(6):902–905
Lefebvre PP, Staecker H (2002) Steroid perfusion of the inner ear for sudden sensorineural hearing loss after failure of conventional therapy: a pilot study. Acta Otolaryngol 122(7):698–702
Plaza G, Herráiz C (2007) Intratympanic steroids for treatment of sudden hearing loss after failure of intravenous therapy. Otolaryngol Head Neck Surg 137(1):74–78
She W, Dai Y, Du X et al (2010) Hearing evaluation of intratympanic methylprednisolone perfusion for refractory sudden sensorineural hearing loss. Otolaryngol Head Neck Surg 142(2):266–271
Salt AN, Ma Y (2001) Quantification of solute entry into cochlear perilymph through the round window membrane. Hear Res 154(1–2):88–97
Saijo S, Kimura RS (1984) Distribution of HRP in the inner ear after injection into the middle ear cavity. Acta Otolaryngol 97(5–6):593–610
Gouveris H, Selivanova O, Mann W (2005) Intratympanic dexamethasone with hyaluronic acid in the treatment of idiopathic sudden sensorineural hearing loss after failure of intravenous steroid and vasoactive therapy. Eur Arch Otorhinolaryngol 262(2):131–134
Bamberger CM, Bamberger AM, de Castro M, Chrousos GP (1995) Glucocorticoid receptor beta, a potential endogenous inhibitor of glucocorticoid action in humans. J Clin Invest 95(6):2435–2441
Sha SH, Taylor R, Forge A, Schacht J (2001) Differential vulnerability of basal and apical hair cells is based on intrinsic susceptibility to free radicals. Hear Res 155(1–2):1–8
Billett TE, Thorne PR, Gavin JB (1989) The nature and progression of injury in the organ of Corti during ischemia. Hear Res 41(2–3):189–197
Kopke RD, Hoffer ME, Wester D, O’Leary MJ, Jackson RL (2001) Targeted topical steroid therapy in sudden sensorineural hearing loss. Otol Neurotol 22(4):475–479
Silverstein H (1999) Use of a new device, the microwick, to deliver medication to the inner ear. Ear Nose Throat J 78(8):595–598
Haynes DS, O’Malley M, Cohen S, Watford K, Labadie RF (2007) Intratympanic dexamethasone for sudden sensorineural hearing loss after failure of systemic therapy. Laryngoscope 117(1):3–15
Plontke SK, Löwenheim H, Mertens J et al (2009) Randomized, double blind, placebo controlled trial on the safety and efficacy of continuous intratympanic dexamethasone delivered via a round window catheter for severe to profound sudden idiopathic sensorineural hearing loss after failure of systemic therapy. Laryngoscope 119(2):359–369
Silverstein H, Choo D, Rosenberg SI, Kuhn J, Seidman M, Stein I (1996) Intratympanic steroid treatment of inner ear disease and tinnitus (preliminary report). Ear Nose Throat J 75(8):468–471
Bird PA, Begg EJ, Zhang M, Keast AT, Murray DP, Balkany TJ (2007) Intratympanic versus intravenous delivery of methylprednisolone to cochlear perilymph. Otol Neurotol 28(8):1124–1130
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Erdur, O., Kayhan, F.T. & Cirik, A.A. Effectiveness of intratympanic dexamethasone for refractory sudden sensorineural hearing loss. Eur Arch Otorhinolaryngol 271, 1431–1436 (2014). https://doi.org/10.1007/s00405-013-2594-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-013-2594-x