Abstract
More than 10 years ago, cone-beam-computed tomography (CBCT) was introduced in ENT radiology. Until now, the focus of research was to evaluate clinical limits of this technique. The aim of this work is the evaluation of specific dosages and the identification of potential optimization in the performance of CBCT of the paranasal sinuses. Based on different tube parameters (tube current, tube voltage, and rotation angles), images of the nose and the paranasal sinuses were taken on a phantom head with the Accu-I-tomo F17 (Morita, Kyoto, Japan). The dosages applied to the lens and parotid gland were measured with OSL dosimetry. The imaging quality was evaluated by independent observers. All datasets were reviewed according to a checklist of surgically important anatomic structures. Even for lowest radiation exposure (4 mA, 76 kV, 180°, computed tomography dosage index (CTDI) = 1.8 mGy), the imaging quality was sufficient. Of course a significant reduction of the imaging quality could be seen, so a reliable mean was set for 4 mA, 84 kV, and 180° rotation angle (CTDI = 2.4 mGy). In this combination, a reduction of 92 % in lens-dose and of 77 % of dosage at the parotid gland was observed in comparison to the maximal possible adjustments (8 mA, 90 kV, 360°, CTDI = 10.9 mGy). There is potential for optimization in CBCT. Changing the rotation angle (180° instead of 360°) leads to a dose reduction of 50 %. Furthermore from clinical point of view in case of chronic rhinosinusitis a relevant reduction of dosage is possible. Therefore, it is necessary to intensify the interdisciplinary discussion about the disease specifics required quality of imaging.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The knowledge about the individual anatomic situation plays a central role for surgeons to plan interventions and to prevent complications. The current German guidelines for chronic rhinosinusitis recommend radiological imaging before surgery of the paranasal sinuses as a standard procedure [1]. The formerly used conventional radiography has been replaced by computed tomography. About 10 years ago, cone-beam-CT (CBCT) was introduced for imaging of head and neck region. Until now, research focused on the possibilities of CBCT in several diseases. So CBCT turned out to be a useful tool for diagnosis of the nose, the anterior skull base as well as for the imaging of the temporal bone [2–6]. To find the specific position in the spectrum of radiological imaging procedures, a more basic science-oriented research is necessary. Especially questions regarding the applied doses have to be answered. Kyriakou and co-workers [7] compared a high-end CT (Siemens dual source) with dental CBCTs. They found no dose advantage in CBCT in this context. But as criticism, it has to be mentioned that the 10-year-old CBCT of their study cannot be compared to currently used devices in ENT and second, the spread of the dual-source-CT is narrow. Our own data show an advantage of CBCT in comparison to a 64-slice CT of factor two to five. Therefore, a definite conclusion regarding the differences in dosage between CBCT and CT is still not possible.
The aspects of the necessary imaging quality for visualizing the paranasal sinuses have not been lighted up. The aim of this study was therefore to evaluate the possibilities of the reduction of dosage on CBCT with focus on the imaging quality. Different images of a phantom head was performed. Measurement of the doses applied directly to the lenses and the parotid glands were performed by optical stimulated luminescent dosimetry (OSL dosimetry). Afterward, a critical evaluation of the images was performed by head and neck radiologists, ENT surgeons, and specially trained ENT specialists of head and neck imaging.
Materials and methods
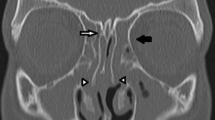
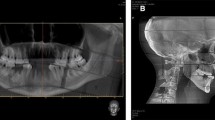
A special phantom head was used for further studies (Fig. 1, right side). To visualize the comparability of the phantom head to the real human situation, a typical coronar view of the paranasal sinuses of both subjects (parameters: 360°, 84 kV, 4 mA) was given (Fig. 2).
All images were made with the CBCT device by Morita (Accu-I-tomo F17, Morita, Kyoto, Japan) (Fig. 1, left side). This device allows a variation of the tube voltages from 60 to 90 kV in 1-kV steps and a variation of the tube current from 1 up to 10 mA in 0.5-mA steps. In Addition, a variation of the rotation angle between 180° (9 s rotation time) and 360° (17 s rotation time) is possible. Especially the 180° modus is interesting because rotation only around the back of the head is possible. Thus the lenses are not directly exposed to irradiation. Furthermore, different fields of view (4 cm in diameter and 4 cm in height up to 17 cm in diameter and 12 cm in height) are possible with this device.
Until now, images were performed by standard X-ray adjustments (360°, 90 kV, 8 mA) according to the recommendations of Morita Company. In this study, images of the nose and the paranasal sinuses of the phantom head with a field of view of 10 cm in height and 10 cm in diameter were performed. Different combinations of tube voltages (90 kV, 84 kV and 76 kV), tube currents (8 mA and 4 mA), and rotation angles (360° and 180°) were evaluated. The according computed tomography dose indices (CTDI) with the reduction in comparison to the maximal possible values (360°, 90 kV, and 8 mA) are presented in Table 1.
To compare the different datasets, equal levels of brightness and contrast were taken. A checklist of the clinically and surgically important anatomic structures of the nose and the paranasal sinuses was developed (a, orbital floor; b, uncinate process; c, lamina papyracea; d, os turbinale; e, anterior ethmoid artery; f, olfactory fossa; g, bony canal of the optical nerve; h, foramen rotundum; i, bony canal of the vidian nerve). This checklist was evaluated for all data sets in a blinded manner by independent observers (head and neck radiologist, ENT surgeons and specially trained ENT specialists for head and neck imaging).
The dose measurements were performed by optical stimulated luminescent dosimetry (OSL dosimetry). OSL-nanoDot-dosimeter from Landauer (Landauer, Europe, Paris) was used (Fig. 3). OSL dosimetry is based on optical stimulation like thermoluminescent dosimetry (TLD). For more than 10 years, it has been used in human dosage measurements. The OSL dosimeter contains carbon-doted aluminiumoxide (Al2O3:C) covered with lightly permeable slices of 5 and 1 mm plastic. This disc is covered by a light, impermeable container measuring 10 mm × 10 mm × 2 mm. In comparison to the TLD in OSL dosimetry a repetition of picking out the data of the dosimeter is possible. Therefore, a determination of the dosage can be performed by independent institutes [8]. The first validation was performed in mammography. Al-Senan and co-workers [9] demonstrated a good linearity (0.99 %) and dosage reproducibility. Because of the high effective ordinal number of Al2O3:C (Z eff = 11,28) a calibration with a special tool provided by the company is necessary.
To realize a consistent dose measurement, the four points of interest were marked (Fig. 1, right side). Doses were measured at both parotid glands and both eye lenses. For each separate combination of rotation angle, tube current and tube voltage, one separate dosimeter was used at each measurement point. For control, three dosimeters (without direct contact to the X-ray-tube) accompanied the other dosimeter all the time. This realized a correction of the dose in relation to the surrounding dosage (place of measurement, transport, place of detection). The control sample of the dosimeter was picked out by the developer of Landauer Europe, Paris.
Results
All datasets were analyzed regarding the anatomic checklist. All observers examined the blinded data set in independent settings, so any influence between the observers could be excluded. In all different dosage levels the anatomic structures could be evaluated in a reliable manner. Of course, the highest dosage parameters (10.6 mGy, 360°, 90 kV, 8 mA) lead to more brilliant images. But still the lowest adjustments (1.8 mGy, 180°, 76 kV, 4 mA) allowed visualization of all important structures. Especially experienced ENT surgeons considered it as good enough for planning paranasal sinus surgery. Figures 4 and 5 show the different adjustments. So everybody can come to his own conclusion.
Visualisation of the different important anatomic structures at a rotation angle of 360° (a floor of orbita, b uncinate process, c lamina papyracea, d os turbinale, e anterior ethmoid artery, f olfactory fossa, g optical nerve, h foramen rotundum, i canal of vidian nerve) with varying tube adjustments (a 360°, 90 kV, 8 mA; b 360°, 84 kV, 8 mA; c 360°, 84 kV, 4 mA; d 360°, 76 kV, 4 mA)
Visualisation of the different important anatomic structures at a rotation angle of 180° (a floor of orbita, b uncinate process, c lamina papyracea, d os turbinale, e anterior ethmoid artery, f olfactory fossa, g optical nerve, h foramen rotundum, i canal of the vidian nerve) with varying tube adjustments (a 180°, 90 kV, 8 mA; b 180°, 84 kV, 8 mA; c 180°, 84 kV, 4 mA; d – 180°, 76 kV, 4 mA)
For each combination of rotation angle, tube voltage and tube current, the dosages on the eye lenses and the parotid glands were measured. The effective surface dosage was evaluated by subtracting the surrounding measured doses from the measured doses at each measuring point. No significant differences between both sides were identified, so that a mean was evaluated. The results are shown in Fig. 6 and summarized in Tables 2 and 3. In Addition, the percental dosage reduction in comparison to the maximal adjustments is given.
With a constant rotation angle of 360° (17 s radiation exposure) a highly significant reduction of the applied dose during variation of tube voltage and tube current can be seen on the lens (90 kV/8 mA = 100 % vs. 84 kV/4 mA = 43 % vs. 76 kV/4 mA = 35 %) and the parotid gland (90 kV/8 mA = 100 % vs. 84 kV/4 mA = 44 % vs. 76 kV/4 mA = 38 %). The same observation can be made for varying voltage and current in cases of the rotation angle of 180° (9 s radiation exposure) for the lens (90 kV/8 mA = 100 % vs. 84 kV/4 mA = 44 % vs. 76 kV/4 mA = 33 %) as well as for the parotid gland (90 kV/8 mA = 100 % vs. 84 kV/4 mA = 45 % vs. 76 kV/4 mA = 37 %).
By varying the rotation angle between 360° and 180° with constant tube voltage and tube current, a clear dose reduction is detected at the lenses as well as the parotid glands. In our combinations, a reduction of about 50 % at the parotid gland and of about 80 % at the lens was possible. The differences between the reduction in cases of the parotid gland and lens result from the type of irradiation. In cases of 360° rotation, the lens and the parotid gland are directly irradiated, whereas in cases of 180° rotation only one parotid gland undergoes direct irradiation. Regarding the lenses, this only indirect irradiation leads to a high-potential of dosage reduction.
So a total reduction of about 80 % in cases of the parotid glands and of about 94 % in cases of the eye-lenses was possible (360°, 90 kV, 8 mA vs. 180°, 76 kV, 4 mA).
As mentioned above, even at lowest adjustments all anatomic structures could be visualized. The observers had knowledge about the fact of analyzing a phantom head. The similarity of visualization in comparison to a real human data set can be seen in Fig. 2. The fact that the analyzed head was just an example and that people with thicker bones or other anatomic dimensions might have poor imaging qualities at lowest adjustments leads to a controversial discussion. Finally, all observers agreed on a mean level of rotation angle of 180°, tube voltage of 84 kV, and tube current of 4 mA. With these parameters, a reduction of the surface dose of 77 % at the parotid glands and of 92 % at the lenses was achieved.
Discussion
Meanwhile, radiological imaging is a standard procedure before the surgery of the chronic diseases of the nose and the paranasal sinuses. The current gold-standard is computed tomography (CT). The upcoming technique of cone-beam-CT (CBCT) has become a competitor to CT in the last years. In ENT diagnostics, the exact role of the CBCT is still not clear. Therefore, further studies have to point out the possibilities of CBCT in different diseases in comparison to CT. Right now, one major advantage of CBCT is the lower radiation exposure. This can be realized by smaller fields of interest and the technique itself. One study from 2011 by Kyriakou and co-workers [7] showed similar dosages of dental CBCTs and a brand new high-end-CT. The analyses of Damet and co-workers [10] showed contrary results, own measurements showed half of the dose in comparison to the 64-slice-CT, so an absolute dosage evaluation is still not possible. Regarding only the dosages, a standard cone-beam CT of the paranasal sinuses has the same values as an X-ray examination of the chest. Regarding the individual risks, it is comparable to the risk of dying during one flight of 5000 km or one cigarette.
The goal of the future will be dose reduction by a discussion of the required disease-related imaging quality. In this context, there are many potential risks. The aim of the current study was to start closing this gap by focusing on chronic rhinosinusitis.
There are different methods of dosimetry of surface doses. One of them is OSL dosimetry known since 1992. In accordance to the TLD the basic physical method is an optical stimulation. But in contrast to TLD, OSL dosimetry realizes a picking out of the data for several times [8] which allows an independent evaluation of the measured dosages [8]. In 2011, the validation of the OSL dosimetry was performed for CT, X-ray, and mammography devices by Al-Senan and co-workers [9].
One of the first systematic overviews of the detailed anatomy of the nose and the paranasal sinuses was given by Zuckerkandl in 1882 [11]. In the context of surgical interventions in this area, the knowledge of the individual anatomy regarding the uncinate process, the lamina papyracea, the olfactory fossa, the os turbinale of the inferior turbinate, the anterior ethmoid artery, the internal carotid artery, the infraorbital nerve, the maxillary nerve, the vidian nerve, and the optical nerve is essential to plan surgery and to prevent intra- and postoperative complications. So these structures lead to an individual risk profile for intraoperative injury of brain or important organs [3, 12, 13]. Furthermore, an injury of the anterior ethmoid artery can lead to strong intraoperative bleedings [14, 15]. Nearly in every surgical intervention of the paranasal sinuses, the uncinate process is a landmark. In conclusion, the German Society of Otolaryngology, Head and Neck Surgery, recommends preoperative CT or CBCT before surgery of the paranasal sinuses in its new guidelines of chronic rhinosinusitis. [1]. The possibilities in imaging of the different anatomic landmarks of the anterior skull base by a high-end CBCT in best imaging quality could be demonstrated before [3, 5, 16–18]. But to what extend a reduction of imaging quality is possible in cases of visualizing the anterior skull has not been focused on until now. So, the aim of our study was to show the influence of the rotation angle, the tube voltage, and the tube current on the quality of images and to discuss the required quality under the aspect of dosage application on lenses and parotid glands.
Beside the brain and the thyroid gland, these two structures are the main risk-organs during radiation exposure [19]. Therefore, the goal of radiation protection in imaging of the head and neck region is to protect these structures. This is possible by varying the X-ray-adjustments (rotation angle, tube current, and tube voltage) or by variation of the examined volume.
In this study, a phantom head equivalent to a human specimen (see Figs. 1, 2) underwent multiple examinations of the paranasal sinuses with variation of the possible X-ray adjustments of the CBCT device. Representative images are demonstrated in Figs. 4 and 5, so everybody can come to his own conclusion regarding quality requirements. Our observers (head and neck radiologists, ENT surgeons, ENT surgeons with special training in imaging) analyzed the blinded data sets and they all saw no reduced interpretation even for the lowest adjustments. Of course it cannot be a general recommendation to apply the absolutely lowest adjustments. In daily routine some images with these adjustments (180°, 76 kV, 4 mA) turned out to be inadequate. So after controversial discussions within our group, a mean adjustment of 180°, 84 kV, 4 mA was taken for further routine procedure. Until now, there was no patient data set (among 500) that could not be assessed. A critical remark must be made regarding the fact that it was always a subjective evaluation of the different observers. However, there are no generally objective possibilities for assessment up to now. Another additional limitation consists in the fact that the assessment of the data is only valid for this one CBCT device. But from our point of view, the message is comprehensible and we could show that a dosage reduction is generally possible. So the dosage reduction of more than 75 % at the parotid glands and of more than 90 % at the lenses is a clear fact. The higher reduction in cases of the lenses can be explained by the technique of the 180° rotation. Hereby the X-ray-tube rotates only around the back of the head, so the lenses are not irradiated directly. Considering the pure values, a much higher irradiation of the lenses is measured in comparison to the parotid glands (1.19 vs. 0.29 mSv) for those adjustments (180°, 84 kV, 4 mA). This is due to the position of both structures in relation to the measured volume. So the lenses are directly in the neighborhood of the field of view of the paranasal sinuses, whereas the parotid glands are only marginally concerned. Furthermore, it is very important to reduce the dosage at lenses which can be achieved by the 180° mode in a perfect way. For all parameters of tube current and tube voltage, a reduction of 50 % in cases of the parotid glands and of 80 % in cases of the lenses could be revealed in the 180° mode. Alternatively a lens protection could be used [20], but this would influence the imaging quality of paranasal sinuses as well.
In conclusion a crucial reduction of the applied dosage for visualization of the paranasal sinuses in cases of chronic rhinosinusitis by CBCT is possible from the clinical and radiological point of view. With a tolerable reduction of imaging quality a dose reduction of more than 90 % at the lenses and of more than 75 % at the parotid glands can be achieved. Furthermore, in CBCT the 180° mode is absolutely appropriate from the aspect of radiation exposure.
References
Stuck BA, C. Bachert P. Federspil et al. (2011) Rhinosinusitis guidelines-unabridged version: S2 guidelines from the German Society of Otorhinolaryngology, Head and Neck Surgery. HNO
Bremke M, R. Leppek and J.A. Werner (2010) Digital volume tomography in ENT medicine. HNO
Güldner C, Diogo I, Windfuhr J et al (2011) Analysis of the fossa olfactoria using cone beam tomography (CBT). Acta Otolaryngol 131(1):72–78
Kurzweg T, Dalchow CV, Bremke M et al (2011) The value of digital volume tomography in assessing the position of cochlear implant arrays in temporal bone specimens. Ear Hear 31(3):413–419
Savvateeva DM, Güldner C, Murthum T et al (2010) Digital volume tomography (DVT) measurements of the olfactory cleft and olfactory fossa. Acta Otolaryngol 130(3):398–404
Offergeld C, Kromeier J, Aschendorff A et al (2007) Rotational tomography of the normal and reconstructed middle ear in temporal bones: an experimental study. Eur Arch Otorhinolaryngol 264(4):345–351
Kyriakou Y, Kolditz D, Langner O, Krause J, Kalender W (2011) Digital volume tomography (DVT) and multislice spiral CT (MSCT): an objective examination of dose and image quality. Rofo 183:144–153
Yukihara EG, McKeever SW (2008) Optically stimulated luminescence (OSL) dosimetry in medicine. Phys Med Biol 53(20):R351–R379
Al-Senan RM, Hatab MR (2011) Characteristics of an OSLD in the diagnostic energy range. Med Phys 38(7):4396–4405
Damet J, Sans-Merce M, Mieville F et al (2010) Comparison of organ doses and image quality between CT and flat panel XperCT scans in wrist and inner ear examinations. Radiat Prot Dosimetry 139(1–3):164–168
Zuckerkandl E (1882) Normale und pathologische Anatomie der Nasenhöhle und ihrer pneumatischen Anhänge. In: W. Braumüller (ed) vol. 1. Vienna
Keros P (1962) On the practical value of differences in the level of the lamina cribrosa of the ethmoid. Z Laryngol Rhinol Otol 41:809–813
Kainz J, Stammberger H (1988) The roof of the anterior ethmoid: a locus minoris resistentiae in the skull base. Laryngol Rhinol Otol (Stuttg) 67(4):142–149
Ohnishi T, Yanagisawa E (1994) Endoscopic anatomy of the anterior ethmoidal artery. Ear Nose Throat J 73(9):634–636
Simmen D, Raghavan U, Briner HR et al (2006) The surgeon’s view of the anterior ethmoid artery. Clin Otolaryngol 31(3):187–191
Bremke M, Wiegand S, Sesterhenn AM et al (2007) Digital volume tomography in the diagnosis of nasal bone fractures. Rhinology 47(2):126–131
Bremke M, Sesterhenn AM, Murthum T et al (2009) Digital volume tomography (DVT) as a diagnostic modality of the anterior skull base. Acta Otolaryngol 129(10):1106–1114
Balbach L, Trinkel V, Guldner C et al (2011) Radiological examinations of the anatomy of the inferior turbinate using digital volume tomography (DVT). Rhinology 49(2):248–252
ICRP (2007) The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP 37(2–4):1–332
Prins R, Dauer LT, Colosi DC et al (2011) Significant reduction in dental cone beam computed tomography (CBCT) eye dose through the use of leaded glasses. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112(4):502–507
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Güldner, C., Ningo, A., Voigt, J. et al. Potential of dosage reduction in cone-beam-computed tomography (CBCT) for radiological diagnostics of the paranasal sinuses. Eur Arch Otorhinolaryngol 270, 1307–1315 (2013). https://doi.org/10.1007/s00405-012-2177-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-012-2177-2