Abstract
Our objective was to devise and assess a multidisciplinary simulated course in training junior doctors for possible difficult airway scenarios. The authors have run a multi-disciplinary difficult airway simulation that was designed to simulate the stresses and complications of a live situation. The course comprised of six to eight difficult airway simulations (using a Laerdal SimMan2 mannequin remote controlled by a “driver”) with two teams moving through the simulations over half a day. The simulation lasted 20 min and was followed by 40 min of in-depth structured facilitated debrief. The course was set in the anaesthetic room of a district general hospital theatre. Seventy-eight candidates (28 anaesthetic trainees, 18 ENT trainees, 19 theatre nurses and 13 operating theatre practitioners) attended this course over 6 training days set over 2 years. The main outcome measures of candidate feedback scored for eight questions on a 1–6 Likert scale. From the results, Audit of Trust inpatient airway fatalities revealed three deaths in 2 years leading up to the introduction of the simulation course. Re-audit of the subsequent 2 years, during which time the course was running, has shown no airway fatalities. A 100 % candidate feedback response rate was obtained. Delegates gave an average score of 4.8 to the simulator replicating the stress of ‘live’ situations; 5.5 to the simulator addressing training needs; 5.6 to the course improving clinical knowledge, teamwork, leadership and non-technical skills. In our conclusions, successful management of a difficult airway situation requires rapid evaluation, effective communication, strong leadership and teamwork, as well as knowledge of local environment and equipment. The results show that candidates felt an improvement in clinical knowledge, teamwork, leadership and non-technical skills, as well as the mutual understanding and respect between related medical and non-medical team members. In addition, audit of airway mortality showed a Trust-wide reduction in inpatient airway related mortality following the course. The results emphatically demonstrate the universal success of this multi-disciplinary training method for all team members, regardless of hierarchical position or background.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The new NHS presents multiple obstacles to safe and effective surgical training [1]. The streamlining of post-graduate education coupled with the European Working Time Directive (EWTD) has considerably truncated a surgeon’s training hours [2] necessitating the evolution and development of formalised work-based assessment systems as well as novel simulation-based training and assessment methods to ensure competence.
As well as the need for developing surgical dexterity in safe and effective tissue handling, surgeons need to acquire a core knowledge base, and the ability to think and work under stress [3]. Essential leadership, communication and team working skills allow for effective and safe clinical decision-making. Traditional methods of training, which have heavily depended on time expended and cumulative experience acquired, have to be revised and supplemented if we are to continue to train high caliber surgeons. These principles also hold true for anaesthetists. The 2010 Royal College of Anaesthetists curriculum recognises the important role of simulation technology in post-graduate anaesthetic training.
Emergency airway situations require rapid evaluation, effective communication within a multi-disciplinary group, strong leadership and directed treatment in a highly stressful situation [4]. They are rare enough that an ENT trainee may not even have observed a particular scenario before they are part of team or even leading the management of an emergency airway case.
Near misses and adverse events have high fatality rates in the aviation industry. Black box investigations reveal that 75 % of airline incidents are related to human error. This has led the aviation governance bodies to introduce emergency scenario simulations to investigate and address potential failures.
Over the last two decades medical academics have turned to the experience gained in the aviation industry to help address the issues arising from inexperience. There were 207 airway medical emergencies reported in the UK between 2008 and 2009 that led to a fatal or undesirable outcome [5].
Krummel [6] defines simulation as a device or exercise that enables the participant to reproduce or represent, under test conditions, phenomena that are likely to occur in actual performance. Simulation training has been advocated for core and higher surgical trainees to approach the complexity of difficult airway scenarios without the risk to a patient [7].
Our institution has a large Head and Neck Oncology department and houses the only regional rehabilitation unit within North West London that manages tracheostomised patients. There have been several critical incidents reported in relation to the emergency airway with three related fatalities over the last 5 years. In response to shared clinical governance concerns on patient safety, the ENT and anaesthetic departments have devised a novel multi-disciplinary difficult airway simulation course that has run every 3–4 months over the last 2 years (six courses in total). This course has been run “in-house” with participation from both the surgical and anaesthetic trainees, as well as operating department practitioners (ODPs) and theatre nurses. The benefits of this training method have been assessed through multi-disciplinary participant evaluation.
Although simulation training for anaesthesia and surgery is established in many European and US medical training centres, to date and to our knowledge, no course has been described that has sought to demonstrate the innovative extra benefit obtained from, multi-disciplinary, combined training in such complex airway scenarios.
Method
A multi-disciplinary local faculty composed of ENT surgeons and anaesthetists educated in simulation-based training designed a course curriculum which attempted to emphasise and highlight the importance of multi-disciplinary management of difficult airway cases and the complimentary roles of the different team members. The over-arching objective was for all staff to obtain a “shared perspective” to patient management, in place of differing tribal perspectives based on the individual disciplines and traditional hierarchical team structures.
As an initial step, various difficult airway cases, based on the real-life experiences of the faculty, were dissected out to reveal the four main themes to clinical scenarios that encompass a wide variety of possible presentations. These four scenarios were:
-
1.
an acutely stridulous patient (e.g. smoker with obstructing laryngeal tumour presenting to A and E the post-neck trauma patient, the postop total thyroidectomy patient with neck haematoma or bilateral vocal cord paralysis, etc.),
-
2.
a patient presenting with upper airway bleeding (e.g. post-tonsillectomy/transoral laser surgery, etc.)
-
3.
a patient who cannot be intubated and ventilated (e.g. poor view of larynx/subglottic stenosis),
-
4.
a patient with a tracheostomy issues (e.g. displaced/blocked tracheostomy tube from secretions or per-stomal bleeding)
Our simulation vignettes were developed based around these four main scenario types for presentation to our multi-disciplinary participants. A typical simulation course (half-day) was organised on the following template (Table 1). Each clinical scenario was followed by a structured debrief and facilitated candidate feedback.
Ethical considerations
Junior doctors and nurses within the Anaesthetic and ENT departments were invited to attend the course. Candidates voluntarily and anonymously completed feedback. Each candidate was given written information about being a subject in a novel training technique. All candidates gave written consent that their feedback could be anonymously used for further training, teaching or publication. No live subjects or human tissues were used in the scenarios.
Candidates
Per scenario: a maximum of two surgeons and two anaesthetists participated with at least one operating department practitioner (ODP) and one theatre nurse.
Per course: six to eight simulations were run per half day (depending on faculty numbers and the ability to run two simulation groups in staggered arrangement, rotating as shown on template). The candidates remained together within their teams throughout the course to provide opportunity to evolve a group dynamic.
Simulation faculty
Ideally as many faculty as candidates.
-
1.
‘Driver’ of the simulator (can also act as patient voice)
-
2.
Nurse/assistant (plant who knows the scenario and can aid candidates within the scenario)
-
3.
Debrief lead facilitator
-
4.
Second facilitator/senior help
Scenarios
We allowed 1 h for each complete scenario and debrief. The debrief took up at least 60 % of the time. Depending on the level of candidate and the complexity of the task, the scenario comprised equal proportions of ‘clinical decision-making’ and ‘ethical dilemma’.
Simulation mannequin and simulation environment
The interactive Laerdel SimMan 2 had an electrically driven compressor, a laptop complete with programmable software and a candidate touch-screen monitor. The difficult airway scenarios were pre-programmed into simulation software and designed to play-out over 25 min in real-time.
Candidates had to use the facilities and equipment usually available to them as if the situation were happening during their normal clinical work. This included bag and mask ventilation set, nasopharyngeal airway tubes, Guedel oral airways, endotracheal tubes, bougie, laryngeal mask airways, intravenous cannulae, oxygen cylinders with tubing, flexible suction catheters, rigid suction catheter with tubing, intubating flexible bronchoscope, tracheostomy tubes, tracheal dilators, emergency surgical trachestomy set, and flexible naso-endoscope. The observations monitor reported oxygen saturations, pulse, blood pressure respiratory rate, end-tidal carbon dioxide and was fully controlled by the driver).
Northwick Park Hospital is presently in the process of installing a dedicated simulation suite to better enable courses such as this. The course in its present format has been adapted to run in the anaesthetic room adjoining the main ENT theatre and has worked extremely well in terms of providing an appropriate environment with the necessary tools, equipment and organizational support. Through the use of a dividing screen we ensured facilitating faculty were kept out of the scenario enactment. Such an arrangement should be possible in other hospitals so the lack of a simulation suite should not be a deterrent to the running a similar course elsewhere.
Introduction session on crisis resource management
Just a routine operation’
At the start of each course, in their teams, candidates watched a 13 min video which features Martin Bromiley talking about non-technical skill failures in his late wife’s care [7]. We then facilitated group discussions of the important issues.
Crisis resource management
Each candidate received a fact-sheet summarising the CRM principles, and how they could be utilised in clinical practice. Crisis resource management (CRM) is the adaptation of Crew resource management. This is a teaching tool developed by the American aviation industry, US military and NASA to address the shortcomings of the cockpit staff to manage situations that they possess the technical ability to resolve. It involves working in a team in a simulated crisis to investigate and address avoidable failures (Table 2).
Closing session and MDT feedback
At the close of the final group discussion, each candidate was asked to fill in a post-course evaluation questionnaire based on a 6-point Likert scale (Table 3). The cumulative results for the workshops have been evaluated. We had a 100 % response rate. Each participator was provided a certificate of attendance.
Results
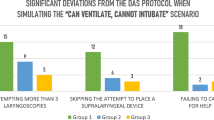
The course has now run six times in 2 years and has had 78 participants. Figure 1 illustrates the multi-disciplinary break-down of course participants and shows a broad multi-professional mix.
Trustwide audit of inpatient airway related mortality was conducted by analyzing the logs of all cardiac arrest crash calls and critical incidents reported for 2 years to the introduction of the course, and also for the same period the course was running. Three airways related avoidable mortalities occurred in 2 years leading up to the course. No such adverse event occurred during the running of the course.
Figure 2 illustrates the post-course questionnaire feedback received. Universally, across the multi-disciplinary participator spectrum there was overwhelming consensus in reporting that this novel simulation course was a positive learning experience.
All candidates scored between 5 and 6 (strongly agree) on the Likert scale in response to the questions:
-
Did the training day match their individual training needs?
-
Were the scenarios presented realistic and believable?
-
Did the debriefing sessions enhance you clinical knowledge and address non-technical skills?
-
Did the course help you reflect on your own individual knowledge and skills base?
A similarly emphatic result and score range between 5 and 6 (strongly agree) was provided by all candidates, declaring overwhelmingly that the course was likely to impact upon their clinical practice and that they felt much more confident handling the acutely unwell complex airway patient having attended the course. The candidates all revealed some degree of discomfort with the simulation environment (scoring on average between 4 and 5 on the Likert scale).
For the purpose of analysis, delegates were divided into junior trainees who had less than 2 years specialty training (core trainees) and senior trainees with more than 2 years (specialty trainees). Although junior trainees on average gave higher scores on Likert scale for each question, un-paired Student’s T test showed no statistical significance between the groups for all questions.
Discussion
Simulators provide an excellent opportunity to practice managing a crisis situation with the opportunity to implement new ideas and make mistakes in a safe and reproducible learning environment [9].
‘Human factors’ and the importance of non-technical skills has been taught in the aviation industry since the 1970s through ‘crew resource management’, and more recently with our own variation termed ‘crisis resource management’ [10]. These ‘non-technical skills’ include items such as situation awareness, team building and leadership, communication, task management, and decision-making [11, 12].
The Fourth National Audit Project coordinated by the Royal College of Anaesthetists [5] revealed an unacceptable level of serious adverse outcomes in airway management. Analysis of the cases identified repeated gaps in care that included: poor identification of at-risk patients, poor or incomplete planning, inadequate provision of skilled staff and equipment to manage these events successfully, delayed recognition of events, and failed rescue due to lack of or failure of interpretation of capnography.
An airway emergency is a high stress situation that frequently involves several health care professionals. Failures are directly related to lack of preparation and poor communication between and within contributing specialities and professionals. Therefore, a course that acts as a “team dress rehearsal” can highlight the importance of non-technical skills as well as demonstrate the knowledge deficiency in a safe manner, allowing targeted help and further training to be recommended in preparation for the real scenario.
Many anaesthetic trainees recognised that with changing work practices and rotas, they may well be the only airway “specialist” on site out of hours. From the earliest point in post-graduate anaesthetic training, it is incumbent on the trainee to be familiar and skilled in the various practical options available for surgically securing the airway.
The benefit of extra information provided by the ENT trainee, through flexible naso-endoscopy (available in most ENT theatres) as a tool during the assessment of the difficult airway patient has also been highlighted. Direct visualisation of the endolarynx where opportunity permits to provide useful knowledge on the state and caliber of the upper respiratory tract, (presence or absence of tumours and blockages) providing diagnostic information and forewarning the anaesthetist of impediments to endotracheal intubation should be considered. In the blocked or displaced tracheostomy tube the flexible nasendoscope also inserted through the tube provides adjunctive information which may readily determine the cause of respiratory distress, as well as allow its remedy (railroading the tracheostomy tube back into the tracheal lumen when displaced using endoscopic guidance).
For this tool to be of clinical value, there needs to be good awareness of inter-specialty resources and skills as well as strong communication between the ENT and Anaesthetic teams. Simulation courses that target non-technical skills such as awareness, teamwork and communication, therefore, allow for a well-rounded approach to crisis management. Indeed during the course of the training day, assessors noted the teams became more accurate at managing the situation, through a better understanding of cross specialty resources and limitations, as well as stronger teamwork through improved communication.
In a crisis situation equipment that one is unfamiliar with, irrespective of how useful it would be in the scenario, is often under-utilized. Simulation courses increase familiarity with equipment and highlight areas of knowledge and practical skills that need focused re-education.
As with technical skills, it is likely that non-technical skills decline with time after training. We are currently in the process of reassessing previous delegates to assess the nature of this decline. In the interim we recommend yearly refresher courses to help reinforce and consolidate skills learnt.
Audit and re-audit of Trust data on critical incidents shows a reduction in airway related mortality during the period, the course has been running. This is a relatively short follow-up period and as the course continues, we will re-audit our outcomes.
The facilitated feedback and in-depth dissection and analysis of team scenarios also helps address non-technical failings such as poor communication or leadership failure. Difficult airway simulation is an ideal modality for this style of education, and naturally lends itself to focus on non-technical skills as well as the clinical aspects of care.
Without exception, a stark contrast is realised by both faculty and participators, when comparing how smoothly the final difficult airway scenario of the course runs relative to the first uninitiated scenario. Communication, teamwork, leadership, situation and environment awareness, planning ahead with maximal utilisation of available resources, mutual appreciation and respect for other team-members skills; all have demonstrably improved over the 3 h session with visibly less stressful faces amongst the whole team when CRM principles are consciously employed.
Results from MDT participator feedback demonstrate that workplace-based, multi-disciplinary simulation can be very effective at teaching difficult airway management and translates into better communication and team functioning, as well as acknowledgement and appreciation of one’s own, as well as others, expertise and skill limitations.
The lower scores rewarded by candidates for the comfort of the simulator is possibly more a reflection of the uncomfortable and stressful nature of the scenarios enacted rather than discomfort caused by the simulation environment.
The benefits are universal and the ultimate gain is in safer patient care. All of our MDT candidates felt more comfortable managing the acute and difficult airway situation after the course than before. This in itself should translate to a less stressful experience when the real-life difficult airway patient presents.
Having trialled this novel course “in-house” over 2 years, summatively collecting and auditing candidate feedback (which in itself enabled further course optimisation and improvement), the faculty now believe the course to have been sufficiently validated in meeting its initial over-arching objective (all MDT staff to obtain a “shared perspective” to management of the difficult airway patient, in place of differing tribal perspectives based on the individual disciplines and traditional hierarchical team structures). The data has already been presented at the Difficult Airway Society in 2010 [13] and 2011 [14]. With further validation, we hope to demonstrate that elements of this MDT simulation approach will prove robust enough to allow sufficiently high fidelity for assessment of candidate competence at Core Trainee (CT) and Higher Surgical Trainee (HST) level in managing the difficult airway patient.
Having been collectively embraced by surgical/anaesthetic trainees, theatre ODPs, theatre nurses and by a multi-disciplinary faculty, the course organizers are now planning to open course enrolment to all our regional trainees (CTs and HSTs in ENT-Head and Neck and Anaesthetics) rotating through training programmes. Through peer-review publication and multi-disciplinary dissemination of the course findings, we are hopeful that other acute care training units across the country, who deal with sufficient numbers of difficult airway patients, will be encouraged to adopt this multi-disciplinary simulation model locally with minimal expenditure.
This innovative and novel approach to MDT difficult airway management has universal/global appeal and on the back of this, collaborative educational network links have already been established between our unit and other similar H and N training centres in Singapore and Sydney to facilitate international exchange of this, and other similar MDT educational courses, materials and tools.
References
Temple J (2010) Time for training. A review of the impact of the European working time directive on the quality of training. http://www.mee.nhs.uk/PDF/14274%20Bookmark%20Web%20Version.pdf. Accessed May 2010
Spencer F (1978) Teaching and measuring surgical techniques—the technical evaluation of competence. Bull Am Coll Surg 63(3):9–12
Holzman RS, Cooper JB, Gaba DM, Philip JH, Small SD, Feinstein DJ (1995) Anesthesia crisis resource management: real-life simulation training in operating room crises. Clin Anesth 7(8):675–687
Reznek M, Smith-Coggins R, Howard S, Kiran K, Harter P, Sowb Y, Gaba D, Krummel T (2003) Emergency medicine crisis resource management (EMCRM): pilot study of a simulation-based crisis management course for emergency medicine. Acad Emerg Med 10(4):386–389
Cook TM, Woodall N, Frerk C (2011) Major complications of airway management in the UK (NAP4). Br J Anaesth 106(5):617–631
Krummel T (1998) Surgical simulation and virtual reality: the coming revolution. Ann Surg 5:635–637
Bromiley M (2008) Have you ever made a mistake? Bulletin of the Royal College of Anaesthetists 48:2442–2445
Gaba DM (2001) Simulation-based training in Anesthesia crisis resource management (ACRM): a decade of experience. Simulation and Gaming 32(2):175–193
Helmreich R (2003) On error management: lessons from aviation. Br Med J 320:781–785
Reader T, Flin R, Lauche K, Cuthbertson BH (2006) Non-technical skills in the intensive care unit. Br J Anaesth 96:551–559
Dieckmann P, Gaba D, Rall M (2007) Deepening the theoretical foundations of patient simulation as social practice. Simul Healthc 2(3):183–193
Kirk R (1998) Surgical excellence-threats and opportunities. Ann R Coll Surg Engl Suppl 80:256–259
Boss JML, Morris H, Tatla T (2010) Teaching difficult airway management to a multidisciplinary team using workplace-based simulation and a crisis resource strategy. Poster presentation at the Difficult Airway Society AGM
Boynton C, Boss J, Mehta N, Tatla T, Morris H (2011) The tools, the process and the training—a three pronged approach to improving the management of the difficult airway. Poster presentation at the Difficult Airway Society AGM
Conflict of interest
There are no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mehta, N., Boynton, C., Boss, L. et al. Multidisciplinary difficult airway simulation training: two year evaluation and validation of a novel training approach at a District General Hospital based in the UK. Eur Arch Otorhinolaryngol 270, 211–217 (2013). https://doi.org/10.1007/s00405-012-2131-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-012-2131-3