Abstract
Evaluation of the severity of disease and the effectiveness of operative treatment is commonly done by registering pre- and postoperative symptoms. During the preceding decade, greater awareness has focused not only on the symptoms but also on patients’ quality of life (QoL). The aim of the study was to determine the effect of septoplasty, as measured by generic and disease-specific QoL questionnaires. The generic 15D and disease-specific SNOT-22 questionnaires were given to patients before the operation and 6 months after the operation. Data analysis consisted originally of 188 septoplasty patients. One-hundred and twenty-six patients (67%) answered the SNOT-22 questions, and in the 15D, the response rate was 76%. In the post-operative SNOT-22, the need to blow the nose, sneezing, runny nose, nasal obstruction, loss of smell or taste, post-nasal discharge, facial pain/pressure, difficulty in falling asleep and waking up at night improved significantly. However in the 15D the mean QoL, i.e., general well-being, became significantly poorer. The QoL became increasingly poor especially in the older age groups and among the patients in which the improvement achieved in nasal symptoms postoperatively was minor. The more nasal symptoms the patients had pre- or postoperatively, the poorer the QoL was in general. Based on our results, critical evaluation of the symptoms and findings in the patients is essential in deciding whether surgery or other treatment should be given to individual patients having nasal blockage symptoms. Especially in patients with mild symptoms or among older patients, adequate medical treatment has to be tried before even considering surgery. The results also encourage the use of a systematic questionnaire to estimate the severity of symptoms in daily clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Septoplasty is one of the most common operations performed at ear-, nose- and throat hospitals. The indications for septoplasty vary. Nasal obstruction, crusting, rhinorrhea, postnasal discharge, recurrent sinus pressure or pain, epistaxis, headache, snoring and sleep apnoea are mentioned as indications for septoplasty [1]. In a questionnaire study done 2 years post-operatively, septoplasty relieved the symptoms well or excellently in 55% and moderately in 27% of the 219 cases [2]. In another follow-up study of 35 cases, 9 months and at 9 years after the operation 55 and 26%, respectively, were subjectively free from obstruction [3]. Septoplasty sometimes results in only limited long-lasting effect on nasal blockage [1].
Society often invests in health care without definite knowledge of the health gains produced, since the systematic assessment of various interventions is usually lacking. This holds true especially for the patient values, i.e., the subjective benefits that patients perceive of treatments. Evaluation of the severity of disease and the effectiveness of treatment is commonly done by registering the pre- and postoperative symptoms. During the preceding decade, greater awareness has focused not only on the symptoms but also on the patients’ quality of life (QoL). The QoL questionnaires can monitor either generic (general) or disease-specific health. Generic health-related quality of life (HRQoL) instruments that produce a single-index number (utility) allow the comparison of cost effectiveness of various interventions in different medical specialties. It is often recommended that both general and disease-specific instruments should be used concomitantly, because, disease-specific HRQoL measurements are considered to be sensitive in detecting the change caused by the treatment. Various disease-specific HRQoL questionnaires, e.g., for rhinitis and rhinosinusitis, have been used [4]. However, the weakness of many of these measurements is that they have seldom been validated.
Several studies have investigated the effect of septoplastic surgery on patient QoL. In a prospective study by Arunachalam et al. [5], 200 septoplasty patients filled preoperative and 6-week postoperative Fairley nasal symptom scores, Nottingham health profiles (NHP) and general health questionnaire (GHQ). Nasal obstruction improvement was seen in 74% and facial pain in 72%, while postoperative improvement in nasal obstruction was independent of the grade of surgeon or concomitant lateral nasal-wall surgery. However, the majority of patients showed no change in generic NHP and GHQ. In a prospective study by Stewart et al. [6], 59 septoplasty patients filled nasal obstruction septoplasty effectiveness scales (NOSE) preoperatively and 3 and 6 months after septoplasty. There was significant improvement in the mean NOSE score at 3 months post surgery, and this change was maintained at 6 months. Severe preoperative nasal obstruction indicated a higher predicted improvement in the NOSE score. In a study using NOSE-score, 89% of the patients reported a subjective improvement in their nasal obstruction and especially younger patients seemed to benefit from septoplasty [7]. Calder and Swan [8] used generic Glasgow benefit inventories in their study in which patients reported minimal improvement in their HRQoL following septal surgery. In a prospective study by Siegel et al. [9], both symptoms and scores demonstrated significant improvement at 6 and 12 months after surgery, as measured by the Nasal Health Survey. The general health status, as measured by Short Form-12, did not change. In another study, there was an improvement in general QoL measured by Short Form Health Survey 4 months after septoplasty, but patients’ social functioning was impaired [10].
This study is part of a larger investigation on septoplasty infection. The results of preoperative antibiotics have been published earlier [11]. The aim in the second part of the study was to determine the effect of septoplasty operation, as measured by generic and disease-specific QoL questionnaires.
Patients and methods
The study was carried out from November 2006 to January 2008. The original study population consisted of 200 consecutive adult septoplasty or septocolumelloplasty patients operated at the Department of Otorhinolaryngology-Head and Neck Surgery, at Helsinki University Central Hospital, Helsinki, Finland. The patients presented for a preoperative clinical status, endoscopy and most patients also for rhinomanometry without and with decongestion. Septoplasty involved correction by mobilizing, straightening and reinserting the cartilaginous (and the bony) septum. The patients could also have inferior turbinate radiofrequency thermal ablation (RFA). The operation was performed under local or general anaesthesia. Written informed consent was obtained from all study subjects. The exclusion criteria of the study were: (1) disease that increased the infection risk, (2) rhinoplasty operation, (3) septoplasty in combination with sinus surgery and (4) age < 18 years.
There were no restrictions or directions for the surgeon regarding the surgical procedure, use of postoperative packing or nasal splints. Septoplasty could be done as day-case surgery or the patient remained overnight in the ward. In day-case septoplasties, the patient arrived next morning for removal of the nasal packing. If the patient remained overnight at hospital, the packing was removed before the patient was discharged.
The operations were performed by 28 different surgeons (19 specialists and 9 residents). In all, 157 operations (84%) were day-case surgeries and the remaining patients remained night at the hospital and were discharged the next morning. A total of 172 operations were performed under local anaesthesia supplemented with intravenous sedation and 16 septoplasties under general anaesthesia. Post-operative nasal packing was used in all operations. The packing was removed on the day following the operation in all but three cases. Silicone sheeting splints were used in 57/188 cases (30%) and the most common (33/57) duration of their use was 7 days (range 1–8 days). RFA treatment was given to 52 patients. The next follow-up visit was arranged no later than 3 months.
The 15-dimension (15D) and the 22-item Sinonasal Outcome Test (SNOT-22) questionnaires were given to the patient before the operation on the operative day and mailed to the patients 6 months after the operation. If the questionnaires were not returned within 2–3 weeks, a new questionnaire was sent twice.
Generic QoL was measured by the 15D, a 15-dimensional, standardized, self-administered HRQoL instrument that can be used both as a profile and a single-index score measure (http://www.15d-instrument.net/15D). The 15D consists of 15 dimensions: moving, seeing, hearing, breathing, sleeping, eating, speech, eliminating, usual activities, mental functioning, discomfort and symptoms, depression, distress, vitality and sexual activity. For each dimension, the respondent must choose one of the five levels that best describes his/her state of health at the moment (best level = 1; the poorest level = 5). Missing answers (provided that there are no more than three) to some of the 15D dimensions can be predicted by linear regression with age, sex and answers to the other dimensions as independent variables (http://www.15d-instrument.net/15D). Valuation of the 15D is based on the application of the multiattribute utility theory. A set of utility or preference weights, elicited from the general public through a three-stage valuation procedure, is used in an additive aggregation formula to generate the utility score, i.e., the 15D score (single-index number) over all the dimensions. The maximum score is 1 (no problems in any dimension) and minimum score is 0 (equivalent to being dead). A minimally important difference ≥0.03 is considered clinically significant or important [12]. In most of the important properties, the 15D compares favorably with other similar instruments [13–17]. The 15D is a sensitive instrument able to detect changes in the HRQoL, e.g., in rhinoconjunctivitis patients [18]. The general Finnish population data on the HRQoL were obtained from a large health examination survey carried out in Finland in 2000 and matched for age and sex when comparing patients with the general population [19].
The SNOT-22 has been used in studies on chronic rhinosinusitis and is also a useful tool in nasal septal surgery [20, 21]. The SNOT-22 has 22 items and was recently reported to be valid and easy to use [20]. In the questionnaire, patients rate each item from 0 (no problem) to 5 (problem as bad as it can be). The total maximum number of points in the SNOT-22 is thus 22 × 5 = 110 points. The patient is also asked to mark at maximum the five most important items.
In a septoplasty study published earlier, in which the SNOT-22 was used pre- and 3 months postoperatively, the scores are 36.3 and 19.3; the difference is 17.0 points [21]. The published scores of chronic rhinosinusitis are 43.9 and 31.3 (3-month postoperative difference 12.6) and in nasal polyps 40.8 and 23.1 (difference 17.7) [20]. In healthy populations, the mean SNOT-22 score is 9.3 [22]. The minimally important difference, i.e., the smallest change in the SNOT-22 score that can be detected by a patient, is 8.9 points [20].
The study was approved by the Research Ethics Board of the Helsinki University Central Hospital. Data analysis and statistics of the study were done by a professional statistician. Statistical analysis was performed with the Student’s t-test in cases where two population means were compared. The results were confirmed using also the Wilcoxon test. Where the requirement for normal distribution was not met, the Mann–Whitney U-test and Wilcoxon signed rank tests were used instead. Spearman rank correlation was used to measure the relationship between the 15D and SNOT-22 scores. The difference between the groups was considered significant at p ≤ 0.05.
Results
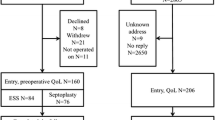
The data analysis consisted of 188 patients. Afterward, 12 patients were excluded because of the following reasons: 7 patients were treated postoperatively by antibiotic not allowed by the study protocol, 2 patients were treated with antirheumatic drugs, 1 patient had insulin-dependent diabetes, one patient underwent sinus surgery in combination with septoplasty and one patient underwent only inferior turbinate-RFA. Demographic data of the patients are shown in the Table 1. The preoperative SNOT-22 (pre-SNOT-22) was answered by 168/188 patients (89%) and the postoperative SNOT-22 (post-SNOT-22) was returned by 137 (73%). In all, 126 patients (67%) answered all the SNOT-22 questions and their data could be used for comparison of the pre- and postoperative results. The preoperative 15D (pre-15D) was answered by 183 patients (97%) and post-15D answers suitable for the analysis were received from 143 patients (76%). The mean age of all septoplasty patients was 41.3 years. The mean age of those patients who did not answer all the QoL questionnaires was 40.7 years.
Generic 15D results
The baseline HRQoL score of the patients (0.949) was slightly higher than that of the general population (0.937, p = 0.019). Compared to the general population the septoplasty patients fared statistically significantly better on the 15D dimensions moving, seeing, speech, discomfort and symptoms, and depression whereas they were worse off on the sleeping dimension (Fig. 1). The mean 15D score before septoplasty was 0.949 and after septoplasty 0.928, p < 0.001 (N = 143). The results of the different pre- and 6-month postoperative 15D -dimensions are shown in Fig. 1. Seeing, hearing, speech, eliminating, mental functioning, discomfort and symptoms, depression, vitality and sexual activity scores were significantly poorer 6 months after septoplasty.
Pre- and postoperative 15D dimensions (N = 143) and those of the general population matched for age and sex. The statistical significance between pre- and post-septoplasty is marked with asterisk and of the preoperative 15D compared with general population is marked with ×, */× p < 0.05, **/×× p < 0.01, ***/××× p < 0.001. Results are expressed as mean + SEM (standard error of mean)
In the 15D score, there were no differences between the various age groups before septoplasty, but there were significant postoperative changes in the two groups (Fig. 2). In the age groups 35–55 years and those older than 55 years, the general decrease in QoL was statistically significant (p < 0.05 and p < 0.01, respectively).
When the pre- and post-15D scores were compared, there were no differences between men and women (p = 0.474), between day-case and ward patients (p = 0.508), or whether or not nasal splints were used (p = 0.730). The operation-type technique (septoplasty N = 93, septocolumelloplasty N = 19 or swinging-door N = 31) or work experience of the surgeon did not affect the 15D score change. The mean score change in the postoperative noninfection group (N = 136) was −0.0203 and in the infection group (N = 7) −0.0423, respectively.
Disease-specific SNOT-22 results
The mean pre-SNOT-22 points were 21.52 (range 0–73) and post-SNOT-22 points 17.40 (range from −44 to 48), and the difference was 4.11, p = 0.000045 (N = 126). Table 2 shows the mean values of the pre- and post-SNOT-22 items and their differences and probability levels. The need to blow the nose, sneezing, runny nose, nasal obstruction, loss of smell or taste, postnasal discharge, facial pain/pressure, difficulty in falling asleep and waking up at night were the items that improved significantly after the operation.
The pre- and post-SNOT-22 in non-RFA patients (N = 92) were 19.30 and 15.77, p = 0.00098. The pre- and post-SNOT-22 in RFA patients (N = 34) were 27.50 and 21.82, p = 0.019. Experience of the surgeon, anaesthesia, use of nasal splints, type of operation (i.e., septoplasty or septocolumelloplasty) or day-surgery did not affect the SNOT-22, p-values 0.12, 0.94, 0.56, 0.95 and 0.70, respectively.
Comparison of 15D and SNOT-22 results
Figure 3 shows the mean generic 15D scores before and after septoplasty divided into four groups, according to pre-SNOT-22 scores. In the groups, the age and sex distributions were similar. There were significant differences between the groups, showing that the higher the score in the SNOT-22, i.e., the more nasal symptoms, the lower the score in the 15D, i.e., the lower the HRQoL.
Figure 4 shows the 15D scores divided into two groups. Hopkins et al. [20] showed that the minimally important difference (i.e., the smallest change in SNOT-22 score that can be detected by a patient) is 8.9 points. In Fig. 4, the first group consisted of patients (N = 82) whose change in the SNOT-22 was less than 8.9 points and in the second group those (N = 44) whose change in the SNOT-22 score was ≥8.9 points. In the first group, the mean pre-SNOT-22 was 15.7 points (range 0–46) and the change in the 15D score was −0.032, p = 0.000. In the second group, the same corresponding values were 32.6 points (range 11–73), score change was 0.0028, and p = 0.701.
Pre- and 6-month postoperative 15D scores divided into two groups according to the mean change in SNOT-22 values. Group 1: change in SNOT-22 is <8.9 points, group 2: change in SNOT-22 is ≥8.9 points. The 8.9 points were chosen for the limit as Hopkins et al. have shown that the minimally important difference, i.e., the smallest change in the SNOT-22 score that can be detected by a patient, is 8.9 points. Results are expressed as mean + SEM
Discussion
This study measured the effect of septoplasty on HRQoL using the disease-specific SNOT-22 and generic 15D questionnaires. Our response-rates were 76% for the 15D and 67% for the SNOT-22 questionnaire. These figures compare favorably with other septoplasty HRQoL studies (49–60%) published [5, 6, 9]. The 188 operations included were septoplasties at a large university hospital, reflecting very well the results in daily clinical praxis. Six months after the septoplasty, as measured by the SNOT-22, the need to blow the nose, sneezing, runny nose, nasal obstruction, loss of smell or taste, postnasal discharge, facial pain/pressure, difficulty in falling asleep and waking up at night improved significantly. However, the general HRQoL, as measured by the 15D-questionnaire, grew increasingly poorer (Fig. 1). HRQoL became poorer especially in the older age group (Fig. 2), and when the improvement achieved in nasal symptoms postoperatively was minor (Fig. 4). The more nasal symptoms the patients had pre- or postoperatively, the poorer the HRQoL (Fig. 3).
In the previous septoplasty studies, a positive effect on HRQoL has often been seen. Septoplasty resulted in significant improvement in disease-specific HRQoL, high patient satisfaction and decreased medication use. Severe preoperative nasal obstruction indicated a higher predicted improvement [6]. After septoplasty, both disease-specific and generic QoL improved in the population of 65 years of age or older [23]. Turbinate surgery improved the outcome of septoplasty surgery [24], but a study showing no effect of lateral nasal-wall surgery was also published [5].
Our SNOT-22 results are well in accordance with the expected results of septoplasty, especially in blockage of the nose which decreased from 2.96 to 1.60, with a mean difference of 1.36 (Table 2). However, the smallness of the mean total pre-SNOT-22 score, 21.5 points, was surprising. The postoperative mean value was 17.4, thus the difference was only 4.1 points. In the previous studies of septoplasty, chronic rhinosinusitis and nasal polyposis the decrease in symptom score was 17.0, 12.6 and 17.7, respectively [20, 21]. We conclude that our patients had significantly milder nasal symptoms than in the studies published earlier. Our study is limited by the lack of a control group. Formation of a control group in surgical studies, however, is always a challenge. In this study, the use of validated QoL-questionnaires and the fact that we studied a consecutive septoplasty patient series diminish the weakness caused by a missing control group.
In healthy populations, the mean SNOT-22 score is 9.3, and in patients, the minimally important difference is 8.9 points [20, 22]. We divided the SNOT-22 results of the patients into two groups (Fig. 4), based on this 8.9 points result. In those patients (35%) in whom the change was ≥8.9, the general QoL did not decrease as it did in the other group with no detectable change (Fig. 4).
The increasingly poor generic HRQoL after the operation is interesting, and worsening was most significant in the oldest age group. The discomfort caused by the operation and convalescence probably outran the benefit that septoplasty gave. It is interesting that in the last four items of the SNOT-22 (reduced concentration, frustrated/restless/irritable, sad and embarrassed) the mean difference was negative, suggesting decreasing HRQoL in these items. Although the changes were not statistically significant, there was thus concordance between the 15D and SNOT-22 results.
Is the increasingly poor QoL clinically relevant? In the previous 15D studies, an increase or decrease of 0.03 or more was clinically important [12]. Throughout our group, the change was −0.021, thus suggesting it was clinically unimportant. However, in the subgroups of elderly patients (change −0.050) and in patients with only a minor decrease in nasal symptoms after septoplasty (change −0.032), the change in HRQoL probably bears significant impact on the life of the patient. A previous study has also shown that younger patients seem to benefit from septoplasty [7].
The Fig. 3 shows the clinically relevant impression that the nasal symptoms are correlated with general well-being. The Fig. 3 shows clearly that the more nasal symptoms the lower the HRQoL. Thus, careful diagnostics and treatment of patients having nasal symptoms are important. Pirilä and Tikanto [25] showed in septoplasty patients with very severe deviation that anterior rhinoscopy is sufficient for preoperative screening, but in milder deviations acoustic rhinometry and rhinomanometry significantly predicted postoperative success.
In our study, those patients who received RFA treatment had higher pre-SNOT-22 points than the non-RFA group (27.50 vs. 19.1), while the decrease in symptoms was also higher, 5.68 versus 3.53, respectively. Thus, we suggest that the RFA treatment could be combined with septoplasty in cases, when in combination with septal deviation, there are also signs that nasal mucosal oedema causes blockage and other nasal symptoms and medical treatment has not eased the symptoms. RFA can be recommended, because it is well tolerated [26].
As far as we know, only three septoplasty studies have investigated the generic pre- and postoperative HRQoL. In a prospective study, 200 septoplasty patients filled NHP and GHQ, questionnaires, and in another study Short Form-12 was used [5, 9]. The general health status of the patients did not change in these studies. In another study, there was an improvement in general QoL measured by Short Form Health Survey 4 months after the septoplasty, but patients’ social functioning was impaired [10]. No previous studies have explored a general HRQoL that became poorer after septoplasty. Our findings may have resulted from septoplasties that were mostly performed on patients with mild symptoms. We have observed a similar, however yet unpublished, deterioration 15D-measured of HRQoL in those coronary artery disease patients who had a good baseline HRQoL. We and surgeons in general are sometimes very optimistic regarding the results that can be achieved when operatively treating patients having nasal blockage. However, we must underline that statistically significant deterioration of general HRQoL has been detected only in this study, and further research is needed to confirm our finding.
We recommend that septoplasty patients having only minor symptoms should not be operated on or at least the indication for septoplasty should be very carefully discussed with the patient. The results of this study also encourage the use of a systematic questionnaire, e.g., the SNOT-22, for patients with nasal symptoms in daily clinical practice to estimate the severity of these symptoms.
Conclusion
In this study undertaken 6 months after septoplasty, the total SNOT-22 score was reduced, showing that septoplasty had decreased the nasal symptoms. However, the mean general well-being, i.e., the HRQoL, became poorer after septoplasty.
Does septoplasty enhance the QoL in patients? The answer is yes if we operate on septal deviation patients with moderate or severe nasal symptoms that can probably expect a detectable cure of these symptoms. The answer is no—and we could even degrade the QoL—if we perform septoplasty on patients with mild nasal symptoms, especially among older patients. The evident cases requiring corrective septoplasty are no problem, but there is often a fine-line between the decision to operate or not to operate in clinical practice. Surgeons are sometimes very optimistic regarding the results that can be achieved when operatively treating patients having nasal blockage. Based on the results of this study, critical evaluation of the symptoms and findings in patients is essential in deciding whether the surgery or other treatment should be given to individuals having nasal symptoms.
References
van Olphen AF (2008) The septum. In: Scott–Brown’s otorhinolaryngology. Head Neck Surg 2:1582–1588
Hytönen M, Blomgren K, Lilja M et al (2006) How we do it: septoplasties under local anaesthetic are suitable for short stay surgery; the clinical outcomes. Clin Otolaryngol 31(1):64–68
Jessen M, Ivarsson A, Malm L (1989) Nasal airway resistance and symptoms after functional septoplasty: comparison of findings at 9 months and 9 years. Clin Otolaryngol Allied Sci 14(3):231–234
van Oene CM, van Reij EJ, Sprangers MA et al (2007) Quality-assessment of disease-specific quality of life questionnaires for rhinitis and rhinosinusitis: a systematic review. Allergy 62(12):1359–1371
Arunachalam PS, Kitcher E, Gray J et al (2001) Nasal septal surgery: evaluation of symptomatic and general health outcomes. Clin Otolaryngol Allied Sci 26(5):367–370
Stewart MG, Smith TL, Weaver EM et al (2004) Outcomes after nasal septoplasty: results from the nasal obstruction septoplasty effectiveness (NOSE) study. Otolaryngol Head Neck Surg 130(3):283–290
Gandomi B, Bayat A, Kazemei T (2010) Outcomes of septoplasty in young adults: the nasal obstruction septoplasty effectiveness study. Am J Otolaryngol 31(3):189–192
Calder NJ, Swan IR (2007) Outcomes of septal surgery. J Laryngol Otol 121(11):1060–1063
Siegel NS, Gliklich RE, Taghizadeh F et al (2000) Outcomes of septoplasty. Otolaryngol Head Neck Surg 122(2):228–232
Croy I, Hummel T, Pade A et al (2010) Quality of life following nasal surgery. Laryngoscope 120(4):826–831
Lilja M, Mäkitie AA, Anttila VJ et al (2011) Cefuroxime as a prophylactic preoperative antibiotic in septoplasty: a double blind randomized placebo controlled study. Rhinology 49:58–63
Sintonen H (1994) The 15D-measure of health-related quality of life: I. Reliability, validity and sensitivity of its health state descriptive system. National Centre for Health Program Evaluation, Melbourne (Working Paper 41)
Sintonen H (1995) The 15-D measure of health-related quality of life: II feasibility, reliability and validity of its valuation system. Working Paper 42. National Center for Health Program Evaluation. National Health and Medical Research Council. Melbourne (http://www.buseco.monash.edu.au/centres/che/pubs/wp42.pdf)
Stavem K (1999) Reliability, validity and responsiveness of two multiattribute utility measures in patients with chronic obstructive pulmonary disease. Qual Life Res 8:45–54
Hawthorne G, Richardson J, Day NA (2001) A comparison of the assessment of quality of life (AQoL) with four other generic utility instruments. Ann Med 33:358–370
Sintonen H (2001) The 15D instrument of health-related quality of life: properties and applications. Ann Med 33:328–336
Moock J, Kohlmann T (2008) Comparing preference-based quality-of-life measures: results from rehabilitation patients with musculoskeletal, cardiovascular, or psychosomatic disorders. Qual Life Res 17:485–495
Petersen KD, Kronborg C, Gyrd-Hansen D et al (2008) Quality of life if rhinoconjuctivitis. Allergy 63:284–291
Aromaa A, Koskinen S (2004) Health and functional capacity in Finland. Baseline results of the Health 2000 health examination survey. Publ Natl Public Health Inst Series B 127:171
Hopkins C, Gillett S, Slack R et al (2009) Psychometric validity of the 22-item Sinonasal Outcome Test. Clin Otolaryngol 34(5):447–454
Buckland JR, Thomas S, Harries PG (2003) Can the Sino-nasal Outcome Test (SNOT-22) be used as a reliable outcome measure for successful septal surgery? Clin Otolaryngol Allied Sci 28(1):43–47
Gillett S, Hopkins C, Slack R et al (2009) A pilot study of the SNOT 22 score in adults with no sinonasal disease. Clin Otolaryngol 34(5):467–469
Busaba NY, Hossain M (2004) Clinical outcomes of septoplasty and inferior turbinate reduction in the geriatric veterans’ population. Am J Rhinol 18(6):343–347
Samad I, Stevens HE, Maloney A (1992) The efficacy of nasal septal surgery. J Otolaryngol 21(2):88–91
Pirilä T, Tikanto J (2009) Acoustic rhinometry and rhinomanometry in the preoperative screening of septal surgery patients. Am J Rhinol Allergy 23:605–609
Hytönen ML, Bäck LJJ, Malmivaara AV et al (2009) Radiofrequency thermal ablation for patients with nasal symptoms: a systematic review of effectiveness and complications. Eur Arch Otorhinolaryngol 266(8):1257–1266
Acknowledgments
We thank Timo Pessi for doing the statistics. We also thank the Department of Otorhinolaryngology’s Research Funds for financial support.
Conflict of interest
None of the authors have any commercial association that might pose a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hytönen, M.L., Lilja, M., Mäkitie, A.A. et al. Does septoplasty enhance the quality of life in patients?. Eur Arch Otorhinolaryngol 269, 2497–2503 (2012). https://doi.org/10.1007/s00405-012-1931-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-012-1931-9