Abstract
Radiotherapy (RT) or concurrent chemoradiation therapy (CCRT) is not only effective at patients’ survival rates, but also produces undesirable late complications. The purpose of this study is to investigate the post-treatment late complications in nasopharyngeal carcinoma (NPC) patients, and to analyze the individual impact factors. We enrolled 188 newly diagnosed NPC patients who had received complete treatments and at least 3 years’ follow-up between March 1984 and March 2010. Late complications were modified from the Toxicity Criteria of the Radiation Therapy Oncology Group and the European Organization for Research and Treatment of Cancer. Of 188 patients, 132 were male and 56 were female. Eighty-eight patients received CCRT and the other 100 patients received RT alone. The median follow-up duration was 7.34 years (range 3.30–26.54). Only 5.3% of patients reported no complication during post-treatment follow-up. The most common major and minor complications were osteoradionecrosis (10.1%) and xerostomia (56.4%), respectively. There was no impact factor for age, underlying disease, and cancer staging. However, there was a negative impact factor for xerostomia and limb numbness in the CCRT group compared with the RT group. Besides, re-radiation for recurrent patients could increase the risk of major complications. Fortunately, these major complications were reduced after the introduction of intensity-modulated radiotherapy in 2003. The improvement of treatment modality decreased the risk of major complications. Physicians should pay more attentions and improve patients’ quality of life during follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nasopharyngeal carcinoma (NPC) is a common head and neck cancer in Taiwan. The crude annual incidence was reported to be 9.99/100,000 in the male population and 3.47/100,000 in the female population in 2008. The median age of newly diagnosed NPC patients has also been reported to be 49 years in the male population and 48 years in the female population [1]. Radiotherapy (RT) has been the standard treatment for NPC for decades. Aside from this, concurrent chemoradiation therapy (CCRT) is effective for locoregional advanced NPC patients. The 3-year progression-free survival rate was 71%, and the overall survival rate was 75% [2]. The 5-year overall and disease-free survival rate were 59 and 52%, respectively [3]. The 10-year overall survival rate in 5,037 NPC patients was 43% [4]. Although effective at patients’ survival rates, RT could also produce undesirable post-treatment late complications. This is because the nasopharynx is at the base of skull and is surrounded by the brain stem, spinal cord, pituitary–hypothalamic axis, temporal lobes, eyes, middle ear, inner ears, and parotid glands. All these organs limit the amount of RT that can be delivered to the tumor. The years of patients’ life could be prolonged after treatments but these undesirable late complications would indeed impair patients’ quality of life (QOL). The most common radiation-related complication is xerostomia (91.8–97.5%) [5, 6]. Cranial nerve neuropathy or osteoradionecrosis (ORN) is a rare but serious late complication. These complications increase medical comorbidity and social cost. The purpose of this study is to investigate the late complications of NPC patients who had received RT or CCRT at a single institution, and to analyze the individual factors among the complications. Finally, we aimed to realize the characters of the late complications and improve patients’ QOL in the future.
Materials and methods
An Institutional Review Board, Taipei Veterans General Hospital-approved retrospective chart review (2011-05-021IC) was performed on newly diagnosed NPC patients who had received RT or CCRT at a tertiary referral hospital in Taiwan, between March 1984 and March 2010. Exclusion criteria were as follows: (1) Patients had not completed treatments before March 2007, (2) had received treatments at another hospital, (3) was loss to follow-up during this period, (4) had follow-up for less than 3 years, or (5) had died from NPC during this period. All patients received a standard follow-up program under the senior author’s service at the hospital, including detailed head and neck examination every month during the first year, every 2 months in the second year, every 3 months in the third year, and every 6 months thereafter. History-taking and complete head and neck examination were performed in the outpatient department. The fiberscopy was arranged to check up the upper aerodigestive tract in detail every visit. The nasopharyngeal MRI or CT was performed 6 months after treatment and at every annual checkup. The data, including complication symptoms and date of occurrence after treatments, were obtained from the patients’ medical records. Besides, general data, including age, gender, symptoms at initial presentation before treatments, underlying disease, tumor size (T), lymph node involvement (N), presence of distant metastasis (M) according to the Cancer Staging Manual of the American Joint Committee on Cancer (AJCC) version 6.0 in 2002, tumor histopathology [7], total RT dosage, and body mass index (BMI, kg/m2) before and after treatments were also collected. All patients were provided a minimum 3-year follow-up after completion of treatments.
In our institution, RT for NPC was delivered by two-dimensional radiotherapy (2D-RT) before 1996. Between 1996 and 2003, the introduction of three-dimensional conformal radiation therapy (3D-CRT) was used to gradually replace 2D-RT for NPC treatments. After 2003, the intensity-modulated radiotherapy (IMRT) system became a standard strategy for NPC patients. In this study, treatment modality ranged from 2D-RT, 3D-CRT to IMRT. Patients had received 2D-RT or 3D-CRT before 2003. After 2003, all patients received IMRT for the primary tumor and bilateral upper neck and conventional RT for the bilateral lower neck. The total RT dose to the primary tumor and positive neck region was 70–74 Gy in 7–8 weeks and 50–60 Gy in 5–6 weeks to the negative neck region using a linear accelerator of 6 MV photons. All patients were treated with conventional fractionation of 2 Gy per fraction at a dose of 5 daily fractions per week for 7 weeks. Platinum-based chemotherapy was administered to locoregional advanced NPC patients.
The late complications were classified and documented as follows: no complication, minor complications, and major complications with or without minor complications, which were modified from the Toxicity Criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC) [8]. Minor complications were defined as hyperpigmentation, neck fibrosis, xerostomia, middle ear effusion (MEE), chronic otitis media (COM), chronic rhinosinusitis (CRS), choanal stenosis, temporomandibular joint (TM joint) disorder, and limb numbness. Major complications were defined as temporal lobe necrosis, cranial nerve neuropathy, radiation myelitis, ORN, and dysphagia. These major complications mainly affected patients’ neurological functions and decreased their QOL. If the complications were regressed during follow-up, such as MEE or xerostomia, the latency of the late complications was still recorded. Statistical analysis was carried out with a commercially available computer software package. The t test and logistic regression model were used. A p value of 0.05 or less was considered statistically significance.
Results
Between March 1984 and March 2010, the total numbers of newly diagnosed NPC patients under the senior author’s service were 750. The patients enrolled in this study had completed treatments before March 2007. Patients who had not completed treatments, had received treatments at another hospital, loss to follow-up, and died due to NPC were excluded from this study. Thus, the final numbers of the NPC patients were 188. Patients’ demographic data were shown in Table 1. Of 188 patients, 132 were male (70.2%) and 56 were female (29.8%). The mean age was 49.49 ± 12 years (median 50.50, range 17–78 years). One hundred and eighteen of 188 patients (62.8%) had denied any underlying disease such as hypertension, type 2 diabetes mellitus, coronary artery disease, hepatic and renal insufficiency and so on. The most tumor histopathology was undifferentiated carcinoma (99 patients, 52.7%), followed by non-keratinizing carcinoma (84 patients, 44.7%) and keratinizing carcinoma (5 patients, 2.7%). The distribution of cancer staging was 15.4% in stage I, 26.6% in stage II, 42.6% in stage III, and 15.4% in stage IV.
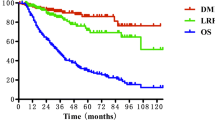
The treatment results of RT and CCRT groups were listed and compared in Table 2. Chemotherapy was added to radiation for 88 patients (46.8%, CCRT group). The other 100 patients (53.2%, RT group) received radiation alone. The mean radiation dosage was 70.05 ± 2.30 Gy in the RT group, and 69.76 ± 5.11 Gy in the CCRT group. The mean radiation dosage for all patients was 69.91 ± 3.87 Gy. Mean pre-treatment and post-treatment BMI were 24.44 (range 16–36) and 21.93 (range 14.82–32.88), respectively. Mean post-treatment weight loss was 6.75 ± 3.6 kg (10.21 ± 4.92%; weight loss compared to pre-treatment body weight). The 44.1% of patients had completed treatments before the introduction of IMRT in 2003, and 55.9% of patients were treated after 2003. The median follow-up duration was 7.34 years (range 3.30–26.54). No complication was recorded in 5.3% of patients during post-treatment follow-up. Minor complications were recorded in 64.4% of patients. There were major complications with or without minor complications in 30.3% of patients. Tables 1 and 2 demonstrated that there was no statistically significant difference in gender, underlying disease, and tumor histopathology between the RT and CCRT groups. There was also no statistically significant difference even in patterns of complications between the two groups. However, there was a statistically significant difference in cancer staging. More locoregional advanced NPC patients were treated with CCRT (p < 0.01). Interestingly, more patients also received CCRT after the introduction of IMRT in 2003 (p < 0.01).
The complication risk before and after introduction of IMRT was revealed in Table 3. It was noted that decreased the risk of major complications after introduction of IMRT in 2003, such as in stage III + IV group (the locoregional advanced group) and CCRT group (p < 0.01). If exclusion of 15 recurrent patients, there were 173 NPC patients who have only received one course of treatment modality. There was also a statistically significant difference in the complication risk among the different radiation methods within those non-recurrent NPC patients (p = 0.03).
The distribution of late complications between the RT and CCRT groups was listed in Table 4. The most common minor complication was xerostomia (56.4%), followed by MEE (43.6%) and neck fibrosis (24.5%). ORN was the most common major complication (10.1%), followed by cranial nerve neuropathy-XII (9.6%) and temporal lobe necrosis (8.5%). The median latency of the three major complications was listed in order of 83.23, 86.23 and 50.67 months, respectively. Before the introduction of IMRT, the median latency of the three major complications was 87.93, 91.87, and 64.18 months, respectively. Interestingly, the median latency of the three major complications in IMRT group showed 51.47, 38.07, and 45.97 months, respectively. Besides, the difference in xerostomia and limb numbness between the RT and CCRT groups was statistically significance (p = 0.030, p = 0.002). Although our late complication classification systems were different from the Toxicity Criteria of the RTOG and the EORTC, there were some relationships between the two classification systems. The minor complications in this study were mostly grade I–II in the Toxicity Criteria. Radiation myelitis which was classified as major complication in our classification system was grade I–II in the Toxicity Criteria. Therefore, those patients would complain L’Hermitte’s syndrome during follow-up. Moreover, the major complications in this study were mostly grade III. However, ORN was the only grade IV complication of the Toxicity Criteria among our major complication classifications.
Table 5 demonstrated no statistically significant difference in age, cancer staging, or underlying disease when different complication groups were compared with logistic regression analysis. However, there were some statistically significant differences for male patients in the major complications group, CCRT in the minor complications group, and re-radiation for recurrent patients in the major complications group. There was also another statistically significant difference in treatment modality after 2003 in major and minor complications (p = 0.019, 0.009). Decreased risks for major complications were noted in patients after the introduction of IMRT in 2003.
Discussion
NPC is a common head and neck cancer in Taiwan. RT is the standard treatment for NPC due to anatomic restrictions and the high degree of radiosensitivity. Chemotherapy also plays a role in the treatment of NPC. CCRT is superior to RT alone for locoregional advanced NPC [9]. Definitions and classifications of late complications in NPC studies reported previously vary due to the different scoring systems used. Lee et al. [10] defined late complications as those occurring more than 90 days after RT and graded them according to the Late Morbidity Scoring Criteria of the RTOG. The 3-year late complication rate in the CCRT group was higher than that in the RT group (28% vs. 13%). In our study, only 5.3% of patients (10/188 patients) reported no major or minor complications. The most minor complications were xerostomia (56.4%), followed by MEE (43.6%) and neck fibrosis (24.5%). The most major complications were ORN (10.1%), followed by hypoglossal nerve palsy (9.6%) and temporal lobe necrosis (8.5%), as shown in Table 4.
Platinum-based chemotherapy is usually administered for locoregional advanced NPC patients. However, platinum-based chemotherapy is a well-known neurotoxic antineoplastic chemotherapy. This is why many NPC patients often complain of limb numbness in a “stocking glove” distribution despite completion of treatments many years later. Platinum associated neuropathy is primarily sensory, especially involving painful paresthesias and numbness in a “stocking glove” distribution [11]. Of the minor complications listed in Table 4, there was a statistically significant difference in xerostomia and limb numbness between the CCRT and RT groups. Platinum-based chemotherapy had indeed impaired the NPC patients’ sensory nerve function. Koom et al. [12] reported that the addition of 5-FU to cisplatin increased severe late toxicity in the skin and mucous membranes. Sumitsawan et al. [13] also stated that the addition of chemotherapy increased the propensity for skin complications and subcutaneous tissue change when compared to that of RT alone. This study also revealed that the addition of chemotherapy affected QOL in terms of peripheral neuropathy and salivary function.
Ten of 15 recurrent NPC patients (66.7%) who had received re-radiation had major complications, as shown in Table 5. Anatomically, the nasopharynx is in close proximity to the brain, spinal cord, lower cranial nerve, and inferior parts of the temporal lobes. Such vital organs have to be included in the radiation portal when prescribing RT for NPC. External beam RT doses of more than 70.2–72 Gy contribute to a higher incidence of radiation-related complications [3, 14]. Leung et al. [15] reported that 91 patients with non-metastatic and locally recurrent NPC treated with re-radiation were associated with a high risk of complications. The 5-year major complication-free rate in this series was 26.7%. Pryzant et al. [16] analyzed 53 patients with locally recurrent or persistent NPC who had received re-radiation. The incidence of severe complications was related to the total cumulative dose of RT. Higher RT doses caused greater vital organ injury; we obtained the same results in this study. A greater number of major complications were noted in recurrent NPC patients. It is possible that these major complications could increase the risks of comorbidity.
The relationship between NPC prognosis and gender remains controversial. Hao et al. [17] reported that the male gender was a significant negative impact factor in local control of NPC. August et al. [18] demonstrated that male was associated with decreased survival rates for non-keratinizing or undifferentiated carcinomas. However, Yeh et al. [3] reported that female patients had independently poor prognostic significance for all otological complications (hearing impairment, tinnitus, and otorrhea). In this study, the male gender was a negative impact factor in major complications. Physicians should pay more attention to male NPC patients over time during post-treatment follow-up because of the higher possibility of the major complications.
IMRT has recently gained popularity as treatment for head and neck cancer. This technique permits modulation of radiation beam intensity so that a high dose can be delivered to the tumor while significantly reducing the dose to the surrounding normal tissues. This means that IMRT provides improved tumor target coverage with significantly better sparing of sensitive and normal tissue structures in the treatments of locoregional advanced NPC compared to conventional RT. Table 3 showed that the risk of major complications was decreased after introduction of IMRT in 2003, in stage III + IV group and CCRT group. Even if patients had received CCRT or with locoregioinal advanced staging, it would not increase the risk of the major complications because of IMRT technology. Several studies have the same results. They have demonstrated that IMRT is superior to conventional 2D-RT while sparing the parotid glands and nervous tissues, including the brainstem, spinal cord, and temporal lobe [12, 19]. Kwong et al. [20] reported that the parotid gland-sparing IMRT achieved good locoregional control, and there was continuous recovery of salivary flow, pH, and buffering capacity in the first 2 years after IMRT. IMRT demonstrated excellent locoregional control with decreased normal tissue effects in the treatment of NPC and improved compliance to adjuvant chemotherapy [21]. Our study recorded more major complications with 2D-RT or 3D-CCRT before 2003. The introduction of IMRT in our hospital in 2003 reduced the occurrence of severe major complications. It preserved key aspects of the QOL and reduced social cost.
The median latency of the three major complications after treatment was listed in order of 83.23 months in ORN, 86.23 months in cranial nerve neuropathy-XII and 50.67 months in temporal lobe necrosis. Huang et al. [22] documented the latency of skull base ORN after treatment ranged 3–15 years. The latency of ORN was 7–24 months if patient received re-radiation for recurrence. Lin et al. [23] reported the latency of cranial nerve palsy after radiation ranged 12–240 months. Tsui et al. [24] showed incidence of late temporal lobe necrosis varied from 1.6 to 22% at the interval of 9 months to 16 years after treatment. Our results were the same with those literatures. It is worth noting there was no significant effect to delay the latency of the three major complications with IMRT. The follow-up time of patients in non-IMRT group was longer than IMRT group. Patients could be death or loss to follow-up because of occurrence of severe major complications in non-IMRT group during follow-up period. The remaining patients in non-IMRT group temporarily do not suffered from severe major complications which lead to death. Besides, there were small sampling size numbers of both groups. Despite of the median latency in non-IMRT group was longer than IMRT group in statistics, the further study should collect more observation data about reasons of death and loss to follow-up to correct the bias. In an analysis of NPC from Hong Kong, the authors reported a 5% incidence rate of patients developed radiation induced cranial/cervical sympathetic nerve palsy [4]. In an analysis of 1,379 patients from China, no cranial nerve palsy was mentioned despite the finding that 18.4% of patients had radiation encephalomyelopathy [25]. In other words, RT induced cranial nerve neuropathy or encephalomyelopathy varied 5–18.4% [4, 25]. In our study, the persisted cranial nerve neuropathy after treatments was about 19.04% (4/21) of total pre-treatment of cranial nerve neuropathy. However, it was difficult to differentiate whether tumor itself or RT-induced cranial nerve neuropathy.
To our surprise, there were no statistically significant differences for age, cancer staging, or underlying diseases between different complication groups with logistic regression model, as shown in Table 5. There was also no statistically significant difference in treatment modality, T staging, N staging, and cancer staging between different complication groups after multivariate analysis. There was only statistically significant difference in re-radiation for recurrent patients within the major complications group after multivariate analysis. Even if patients had received CCRT or with locoregioinal advanced staging, it would not increase the risk of the major complications because of IMRT technology after 2003. We propose that all patients should receive aggressive treatments for NPC despite age, underlying diseases, and even locoregional advanced cancer staging instead of palliative treatments. We believe that these managements could increase locoregional control and improve the patient’s survival rates without more risks of severe major complications.
Limitations
The disadvantages of this study are described as follows: first, it was a retrospective chart review study, and not a prospective study. The final enrolled numbers of the NPC patients are only 188 from 750 newly diagnosed NPC at sensor’s service at a tertiary hospital from 1984 to 2010. As mentioned above, the 5-year overall survival rate was 59%, and the 10-year overall survival rate was 43%, respectively [3, 4]. Almost half of NPC patients would be alive during follow-up period. Besides, because of our country’s national health insurance system, it is very convenient for NPC patients to get any medical service at lower cost from other medical institutes. As the result, the accurate late complication rate may be underestimated due to loss to follow-up, death, or other reasons. However, all patients enrolled in the study had received follow-up of more than 7 years on average. This is the longest follow-up study to be reported in existing related English literature. The entire course of outcomes and managements about late complications were well monitored and documented in the same way under the senior author’s service at a single institute during this period. Second, there was only complication classification system but no grading system in this study. The complication grade should reflect the severity of every complication that occurs during the evaluation period. However, the first Common Toxicity Criteria for RT were published in 1989 and revised in 1999. The latest Common Toxicity Criteria were reviewed in 2003. However, our NPC patients were enrolled from 1984 to 2010. The different grading systems could result in dissimilar assessment criteria. Therefore, the late complication patterns were merely documented without any grading to avoid this drawback. Third, questionnaires about the relationship between QOL and late complications were not available. It is hard to evaluate the disability in the patients’ real life. After all, physicians should resolve patients’ physical and mental problems, and not merely treat the disease itself. Fourth, the latency of the late complications was documented. However, there was no evidence of association between the latency of the complications and any impact factor. More patients’ numbers would be needed to analyze the impact factor of the latency. Finally, dose–volume histogram data was also not available in the study. It lacked the opportunity to correlate with the late complications. Thus, more data will be available and be analyzed in further studies. It could be very useful in clinical practice if getting any information.
Conclusions
The survival rate of NPC was increased after improvement of treatment modality. However, many NPC patients complained of late complications during follow-up. In this study, there was a negative impact factor for xerostomia and limb numbness in the CCRT group. Re-radiation could cause more major complications. However, the risks of major complications were reduced with the introduction of IMRT after 2003. Fortunately, we determined that there was no negative impact factor regardless of patients’ age, underlying disease, and cancer staging. Patients do not need to worry about the side effects of treatments and should be encouraged to complete the entire course of treatments with confidence. Improvement of treatment modality increased the survival rate of NPC and decreased the risk of major complications. Moreover, physicians must pay more attentions to these late complications during follow-up and improve patients’ QOL.
References
Bureau of Health Promotion (2008) Cancer Registry annual report, 2008. Bureau of Health Promotion, Department of Health, The Executive Yuan, Taiwan, pp 28–29
Le QT, Tate D, Koong A, Gibbs IC, Chang SD, Adler JR, Pinto HA, Terris DJ, Fee WE, Goffinet DR (2003) Improved local control with stereotactic radiosurgical boost in patients with nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 56(4):1046–1054
Yeh SA, Tang Y, Lui CC, Huang YJ, Huang EY (2005) Treatment outcomes and late complications of 849 patients with nasopharyngeal carcinoma treated with radiotherapy alone. Int J Radiat Oncol Biol Phys 62(3):672–679
Lee AW, Poon YF, Foo W, Law SC, Cheung FK, Chan DK, Tung SY, Thaw M, Ho JH (1992) Retrospective analysis of 5037 patients with nasopharyngeal carcinoma treated during 1976–1985: overall survival and patterns of failure. Int J Radiat Oncol Biol Phys 23(2):261–270
Hughes PJ, Scott PM, Kew J, Cheung DM, Leung SF, Ahuja AT, van Hasselt CA (2000) Dysphagia in treated nasopharyngeal cancer. Head Neck 22(4):393–397
Epstein JB, Robertson M, Emerton S, Phillips N, Stevenson-Moore P (2001) Quality of life and oral function in patients treated with radiation therapy for head and neck cancer. Head Neck 23(5):389–398
Shanmugaratnam K, Sobin LH (1991) International histological classification of tumors: histological typing of upper respiratory tract tumors and ear, 2nd edn. World Health Organization, Geneva, pp 32–33
Cox JD, Stetz J, Pajak TF (1995) Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 31(5):1341–1346
Cooper JS (2000) Concurrent chemotherapy and radiation therapy for advanced stage carcinoma of the nasopharynx. Int J Radiat Oncol Biol Phys 48(5):1277–1279
Lee AW, Lau WH, Tung SY, Chua DT, Chappell R, Xu L, Siu L, Sze WM, Leung TW, Sham JS, Ngan RK, Law SC, Yau TK, Au JS, O’Sullivan B, Pang ES, O SK, Au GK, Lau JT (2005) Preliminary results of a randomized study on therapeutic gain by concurrent chemotherapy for regionally-advanced nasopharyngeal carcinoma: NPC-9901 Trial by the Hong Kong Nasopharyngeal Cancer Study Group. J Clin Oncol 23(28):6966–6975
Greenspan A, Treat J (1988) Peripheral neuropathy and low dose cisplatin. Am J Clin Oncol 11(6):660–662
Koom WS, Kim TH, Shin KH, Pyo HR, Kim JY, Kim DY, Yoon M, Park SY, Lee DH, Ryu JS, Jung YS, Lee SH, Cho KH (2008) SMART (simultaneous modulated accelerated radiotherapy) for locally advanced nasopharyngeal carcinomas. Head Neck 30(2):159–169
Sumitsawan Y, Chaiyasate S, Chitapanarux I, Anansuthiwara M, Roongrotwattanasiri K, Vaseenon V, Tooncam H (2009) Late complications of radiotherapy for nasopharyngeal carcinoma. Auris Nasus Larynx 36(2):205–209
Yeh SA, Huang YJ (2007) Dose escalation for patients with locally advanced nasopharyngeal carcinoma treated with radiotherapy alone. Am J Clin Oncol 30(4):401–405
Leung TW, Tung SY, Sze WK, Sze WM, Wong VY, Wong CS, O SK (2000) Salvage radiation therapy for locally recurrent nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 48(5):1331–1338
Pryzant RM, Wendt CD, Delclos L, Peters LJ (1992) Re-treatment of nasopharyngeal carcinoma in 53 patients. Int J Radiat Oncol Biol Phys 22(5):941–947
Hao SP, Tsang NM, Chang KP, Hsu YS, Chen CK, Fang KH (2008) Nasopharyngectomy for recurrent nasopharyngeal carcinoma: a review of 53 patients and prognostic factors. Acta Otolaryngol 128(4):473–481
August M, Dodson TB, Nastri A, Chuang SK (2001) Nasopharyngeal carcinoma: clinical assessment and review of 176 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 91(2):205–214
Pow EH, Kwong DL, McMillan AS, Wong MC, Sham JS, Leung LH, Leung WK (2006) Xerostomia and quality of life after intensity-modulated radiotherapy vs. conventional radiotherapy for early-stage nasopharyngeal carcinoma: initial report on a randomized controlled clinical trial. Int J Radiat Oncol Biol Phys 66(4):981–991
Kwong DL, Pow EH, Sham JS, McMillan AS, Leung LH, Leung WK, Chua DT, Cheng AC, Wu PM, Au GK (2004) Intensity-modulated radiotherapy for early-stage nasopharyngeal carcinoma: a prospective study on disease control and preservation of salivary function. Cancer 101(7):1584–1593
Lee N, Xia P, Quivey JM, Sultanem K, Poon I, Akazawa C, Akazawa P, Weinberg V, Fu KK (2002) Intensity-modulated radiotherapy in the treatment of nasopharyngeal carcinoma: an update of the UCSF experience. Int J Radiat Oncol Biol Phys 53(1):12–22
Huang XM, Zheng YQ, Zhang XM, Mai HQ, Zeng L, Liu X, Liu W, Zou H, Xu G (2006) Diagnosis and management of skull base osteoradionecrosis after radiotherapy for nasopharyngeal carcinoma. Laryngoscope 116(9):1626–1631
Lin YS, Jen YM, Lin JC (2002) Radiation-related cranial nerve palsy in patients with nasopharyngeal carcinoma. Cancer 95:404–409
Tsui EYK, Chan JHM, Ramsey RG, Leung TW, Cheung YK, Luk SH, Lai KF, Wong KPC, Fong D, Yuen MK (2001) Late temporal lobe necrosis in patients with nasopharyngeal carcinoma: evaluation with combined multi-section diffusion weighted and perfusion weighted MR imaging. Eur J Radiol 39:133–138
Qin DX, Hu YH, Yan JH, Xu GZ, Cai WM, Wu XL, Cao DX, Gu XZ (1988) Analysis of 1379 patients with nasopharyngeal carcinoma treated by radiation. Cancer 61:1117–1124
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, CC., Ho, CY. Post-treatment late complications of nasopharyngeal carcinoma. Eur Arch Otorhinolaryngol 269, 2401–2409 (2012). https://doi.org/10.1007/s00405-011-1922-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-011-1922-2