Abstract
Bispectral index (BIS) monitor is a neurophysiological monitoring device which continually analyses a patient’s electroencephalogram during sedation and general anaesthesia to assess the level of consciousness and depth of anaesthesia. BIS monitoring, whilst performing sleep nasendoscopy (using midazolam and propofol), has helped validate depth of sedation and allowed comparison with levels of sedation of control patients during natural sleep. A prospective study of 30 patients with snoring undergoing sleep nasendoscopy with BIS monitoring was conducted. BIS monitoring was recorded throughout the procedure and assessment of snoring was made at the appropriate level of sedation and snoring. BIS values were compared with control patients. The 30 patients undergoing sleep nasendoscopy had average BIS values ranging from 50.72 to 61.2. Similar results were seen with BIS and oxygen saturation in the control group. BIS monitoring provides an adjunct to the assessment of sleep nasendoscopy in determining the level of sedation required for snoring assessment. Comparable BIS values and oxygen saturation levels were obtained between controls and patients during sedation-induced sleep, thus validating the role of sleep nasendoscopy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A recent review article by Georgalas et al. [1] addressing an evidence-based approach for the assessment of upper-airway obstruction and patient selection for surgery concluded that sleep nasendoscopy (SNE) could provide useful information in determining the management plan for patients with snoring and obstructive sleep apnoea (OSA). SNE was conceived at our Institute in 1991 and is used as an adjunct for the evaluation of upper airway in sleep disordered breathing with respect to surgical and non-surgical treatment options [2, 3]. However, the role of SNE remains controversial and may also pose concerns with the critics claiming that the drug-induced sleep may be different from the natural physiological sleep and uncertainty around how deeply a patient should be sedated before evaluation. Assessment is subjective and requires appropriate sedative agents and the evaluation at the right time during sedation such that the patient is not too deep or too light is important, as anatomical behaviour and muscle tone variation would possibly correlate with depth of sedation. With the latter issue in mind, this study was designed utilising the bispectral index (BIS) monitor system in order to validate the role of SNE.
BIS monitor is a neurophysiological monitoring device which continually analyses a patient’s electroencephalogram during general anaesthesia to assess the level of consciousness and depth of anaesthesia. Its popularity has arisen due to increasing litigation cases involving intraoperative anaesthesia awareness, predominantly in the USA [4, 5]. A prospective study was undertaken to compare BIS monitoring in patients undergoing SNE for the assessment of snoring with those of control patients with snoring undergoing natural sleep during overnight polysomnography.
Methods
A prospective study of 30 patients (M 22, F 8) with snoring was done as they underwent SNE with BIS monitoring. Patients had a mean age of 46.3 years and body mass index of 29.3 kg m−2. All patients had undergone a sleep study and only patients who did not have moderate or severe OSA were included in this study to proceed with SNE. SNE was performed in our day surgery unit with midazolam (0.05 mg kg−1) and propofol (1.5 mg kg−1). This combination enabled midazolam to provide the background sedation, while the rapid action of propofol allowed for gradual titration and fine-tuning of sedation. BIS monitoring involved a lead of four sensor electrodes attached to the forehead (Fig. 1) which recorded values from 0 (no EEG brain activity) to 100 (patient fully awake). Light sleep occurs at BIS values of 75–90, slow-wave sleep occurs at 20–70 and rapid eye movement sleep occurs at 75–90. Standard cardiovascular monitoring was carried out. Upper airway evaluation and sedation were performed by the two senior authors for all 30 cases.
An assessment of snoring was made at the appropriate level of sedation and snoring. Values of oxygen desaturation levels occurring during natural sleep, whilst having the sleep study were used to indicate appropriate timing of when to introduce the endoscope. Assessment is not made on immediate onset of snoring but delayed until one cycle of apnoea followed by breakthrough and then repeated snoring occurs. Initial sedation tends to be deeper than natural sleep but is helpful in allowing the passage of the nasendoscope without nasal irritation. This is then held in place until one cycle of sleep disordered breathing has passed. Assessment occurs on the second and even third cycle of sleep.
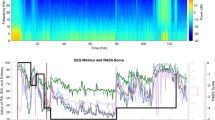
BIS values were noted during the procedure (Fig. 2) and compared with control patients who snored and were admitted undergoing natural sleep during an overnight polysomnography for sleep apnoea assessment.
Results
Snoring was demonstrated in all 30 patients undergoing SNE with BIS monitoring. Assessment was made with decreasing BIS values as the patients sleep deepened, and reassessed as sleep lightened and BIS values increased, thus allowing visualisation of the upper-airway obstruction twice at similar depth of sedation. Comparison was made with the oxygen desaturation levels observed in the patients’ natural sleep during previous sleep study, and used as a guide with the BIS value for assessment at the appropriate time of sedation to best mimic natural sleep.
Average BIS values ranged from 50.66 to 63.1 during SNE snoring evaluation (Fig. 3). Similar results were seen with BIS monitoring in control patients having natural sleep during polysomnography (48.7–61.2). On analysis of variance there was no significant difference in BIS recorded ranges in both the SNE group and the control group, P value of 0.72.
Discussion
SNE assessment of snoring is useful as it provides evaluation of the upper airway in the dynamic mode during sleep. However, numerous controversies and debates have arisen and attempts have been made to address some of these by various authors. For instance, criticisms made by Marais [6], whilst comparing snorers and non-snorers, it was claimed that snoring was produced during SNE in a large number of the non-snorers and was not produced in many of the snorers. This was challenged by Berry et al. [7], demonstrating in their study using target-controlled infusion of propofol during SNE that all their snorers and non-snorers responded as expected. Similarly, questions and concerns that arose about test–retest reliability and of inter-rater reliability of SNE have been elegantly addressed by studies conducted by Rodriguez-Bruno et al. [8] and Kezirian et al. [9], respectively. The issue of assessing the patient at the correct moment has not previously been addressed, and this indeed is an important point as one has to bear in mind the pharmacology and the pharmacokinetics of the different drugs used during sedation. With this in mind our present study with BIS was designed. If the patient is assessed too early, the muscle relaxation effect of the drug may be over emphasised and if the patient is assessed too late then important anatomical aspect of the obstructive episodes may be missed. Thus the depth of sedation during which the assessment is conducted should be as close to the levels of depth of natural sleep. Evaluation only occurs as a snapshot of a patient’s whole sleep cycle. However, combining it with BIS values of patients undergoing natural sleep has allowed a more accurate assessment of sleep disordered breathing.
BIS monitoring has provided an adjunct to the assessment of SNE in determining the level of sedation required for snoring assessment. Previous studies have shown how SNE can be used for the assessment of snoring level [2, 3]. Combining this with BIS monitoring allows more accurate assessment of sedation induced snoring. Others have disputed a lower incidence of anaesthesia awareness with BIS monitoring [10]; however, our results are comparable with BIS values obtained for control patients with snoring undergoing natural sleep. BIS monitoring, while performing SNE, has helped validate depth of sedation and mimics those levels of sedation of control patients with snoring undergoing overnight polysomnography.
References
Georgalas C, Garas G, Hadjihannas E, Oostra A (2010) Assessment of obstruction level and selection of patients for obstructive sleep apnoea surgery: an evidence based approach. J Laryngol Otol 124:1–9
Croft CB, Pringle M (1991) Sleep nasendoscopy: a technique of assessment in snoring and obstructive sleep apnoea. Clin Otolaryngol 16:504–509
Kotecha BT, Hannan AS, Khalil HMB, Georgalas C, Bailey P (2007) Sleep nasendoscopy: a 10-year retrospective audit study. Eur Arch Otorhinoloaryngol 264:1361–1367
Sleigh JW, Andrzejowski J, Steyn-Ross A, Steyne-Ross M (1999) The bispectral index: a measure of depth of sedation. Anesth Analg 88(3):659–661
Myles PS, Leslie K, Forbes A, Chan MT (2004) Bispectral index monitoring to prevent awareness during anesthesia: the B-Aware randomised controlled trial. Lancet 363(9423):1757–1763
Marais J (1998) The value of sedation nasendoscopy: a comparison between snoring and non-snoring patients. Clin Otolaryngol Allied Sci 23:74–76
Berry S, Robin G, Williams A, Watkins A, Whittet HB (2005) Validity of sleep nasendoscopy in the investigation of sleep related breathing disorders. Laryngoscope 115:538–540
Rodriguez-Bruno K, Goldberg AN, McCulloch CE, Kezirian EJ (2009) Test-retest reliability of drug-induced sleep endoscopy. Otolaryngol Head Neck Surg 140:646–651
Kezirian EJ, White DP, Malhotra A, Ma W, McCulloch CE, Goldberg A (2010) Interrater reliability of drug-induced sleep endoscopy. Arch Otolaryngol Head Neck Surg 136(4):393–397
Avidan MS, Zhang L, Burnside BA, Finkel KJ, Searleman AC, Selvidge JA, Saager L, Turner MS, Rao S, Bottros M, Hantler C, Jacobsohn E, Evers AS (2008) Anesthesia awareness and the bispectral index. N Engl J Med 358(11):1097–1108
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Babar-Craig, H., Rajani, N.K., Bailey, P. et al. Validation of sleep nasendoscopy for assessment of snoring with bispectral index monitoring. Eur Arch Otorhinolaryngol 269, 1277–1279 (2012). https://doi.org/10.1007/s00405-011-1798-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-011-1798-1