Abstract
Sarcoidosis is a chronic systemic disease of unknown etiology characterized by non-caseating inflammation involving one or more organs with predilection for pulmonary and upper respiratory tract involvement. It presents with a variety of signs and symptoms which can be generalized or focused on a single organ. Sinonasal involvement is reported in about 1% of cases of sarcoidosis. Sarcoidosis can involve both the mucosa as well as bony structures in the nose and the paranasal sinuses. We present seven cases of sarcoidosis with sinonasal involvement. Four cases presented with nasal and sinus symptoms, and the other three cases developed or presented with nasal and sinus symptoms after the diagnosis of sarcoidosis was confirmed. The nasal and sinus symptoms in these patients were managed by local and systemic steroids. In four patients, endoscopic sinus surgery was performed with good outcome. Nasal and sinus symptoms, differential diagnosis and the treatment are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sarcoidosis is a multisystemic inflammatory disease of still unknown etiology. It involves lungs and intrathoracic lymph nodes in more than 90% of the cases. Histologically it is characterised by the formation of immune granulomas consisting of characteristic non-caseating epitheloid cells.
Activation of T cells and macrophages with release of various chemokines and cytokines including tumor necrosis factor, TNF-α, is believed to be one of several inflammatory pathways along which the granulomatous process is running [1–4].
Sarcoidosis may involve virtually any organ in the body. Beside intrathoracic involvement, skin lesions, extrathoracic lymph node involvement, eye and liver involvement are regarded most common [2].
In 1905 Boeck described granulomatous involvement of nasal mucosa. Later, several studies have described upper respiratory tract involvement in general and sinonasal manifestations in particular [5–14].
The prevalence of sarcoidosis varies from less than one to 40 cases per 100,000. The disease is more prevalent in rural south-eastern USA and Scandinavian countries. Colored races are more affected than white and females more than males. The onset is between 20 and 40 years, and 50% of the cases occur below the age of 30 years [1, 2].
The diagnosis is established by clinical and appropriate X-ray findings supported by biopsy of clinically involved tissues in which granulomas are found.
Serum angiotensin converting enzyme (ACE) is commonly elevated in sarcoidosis, but this elevation is both non-specific and insensitive [15]. The diagnostic value of ACE is debated, but it is considered useful in monitoring the course of the disease [4].
Hypercalcemia is seen in approximately 10% of the patients and hypercalciuria in around 35% of cases [1, 16].
The course and prognosis of the disease correlate with the mode of onset. An acute onset in the presence of erythema nodosum indicates a self-limited course with spontaneous resolution, whereas an insidious onset may be followed by a relentless course. Corticosteroids relieve symptoms and suppress inflammation and granuloma formation [1–4].
The aim of this study was to look into patients with sarcoidosis referred to our department due to sinonasal manifestations. Our experience, outcome and the review of the literature are discussed.
Material
We have retrospectively reviewed the patients with sinonasal involvement with sarcoidosis in our department for the past 10 years. The number of such patients was seven with female:male ratio 4:3 and age range 30–54.
Four patients presented with sinonasal manifestations and three patients developed sinonasal manifestations after the diagnosis of sarcoidosis was made. Three patients had only sinonasal manifestations without any other symptoms or manifestations (Table 1).
Method
The ENT examination was done on all patients and all the patients were investigated for other organ involvement of sarcoidosis.
The measurement of serum calcium was done in five patients, serum angiotensin converting enzyme (ACE) in six patients, serum antineutrophil cytoplasmic antibodies (ANCA) in five patients and Montoux test in four patients, erythrocyte sedimentation rate (ESR) in all seven patients, chest radiograph in all seven patients and computer tomograms (CT) of mediastinum in four out of total seven cases.
Biopsies of nasal sinus tissue was performed in all seven cases, cervical lymph node biopsy in one case, transbonchial biopsy in three cases, mediastinal lymph node biopsi in one case and lacrimal gland biopsy in one of total seven cases (Table 2).
Sections from paraffin-embedded formalin fixed tissue were stained for periodic acid-Schiff, methenamine silver and acid-fast stain (Ziehl-Neelsen) to rule out infection by fungi and mycobacteria.
These are conditions where non-caseating granulomas also can be histologically shown.
Results
The results are summarized in Table 2.
On serological investigations, two patients had raised level of serum calcium, three patients had normal serum calcium and two patients did not have their serum calcium done. Three patients had normal serum angiotensin converting enzyme (ACE), three had raised values of serum ACE and one patient did not have serum ACE done. Five patients showed negative ANCA and two patients did not have ANCA done. One patient had positive Montoux, three patients had negative Montoux and three patients did not have their Montoux done. Five patients showed normal erythrocyte sedimentation rate (ESR) and two patients had not got ESR done.
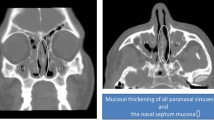
Radiological investigation revealed on chest X-ray hilar shadows in five patients (Fig. 1).
Two patients had normal findings on chest X-ray. Computer tomography of mediastinum showed mediastinal lymph nodes in four patients (Fig. 2) and three patients did not have their CT mediastinum done.
Histological investigations showed in all seven patients typical non-caseating granulomas in nasal sinus tissue (Fig. 3). Three patients showed granulomas on transbronchial biosy and one patient showed granulomas in mediastinal lymph node (Fig. 4). Three patients did not undergo transbronchial or mediastinal biopsy. One patient showed granulomas in cervical lymph node and one patient showed granulomas in lacrimal gland.
The treatment of these patients with confirmed sarcoidosis consisted of either medical therapy or endoscopic sinus surgery, or both.
The medical treatment consisted of local corticosteroids and/or systemic corticosteroids. The duration of medical treatment was variable ranging from few months to still continuous treatment.
Three patients were treated with systemic steroids and no surgical intervention was needed. In four patients endoscopic surgery was performed in addition to medical therapy.
Present medication:
Three patients are on no medication and are symptom free.
Two of the patients are on local nasal steroids.
One patient is using both systemic and local steroids.
One patient is on systemic steroids only (Table 3).
Discussion
In 1983 McCaffrey et al. [5] reviewed the records of 2,319 patients with the diagnosis of sarcoidosis to determine the incidence of nasal involvement. 13% patients were found to have nasal involvement. Seventeen patients (1%) had nasal lesions proven by biopsy to be non-caseating granulomatous inflammation. Additional seven patients demonstrated similar nasal clinical findings, but were not biopsied. The treatment of nasal sarcoidosis consisted of systemic steroids and in some cases topical beclomethasone dipropionate.
Wilson et al. [6] in 1988 reviewed 750 sarcoidosis patients and found involvement of the nasal mucosa in 27 patients, confirmed by histology in 21. Nasal stuffiness and crusting were the major symptoms. Topical medication improved symptoms in some patients, but the majority required systemic corticosteroids.
In a review of six patients described by Shah et al. [7] in 1997 four of the six patients were diagnosed to have sarcoidosis on the basis of their otolaryngological presentation. Oral steroid therapy was the principal treatment given.
The most common presenting symptom in eight patients described by Fergie et al. [8] in 1999 was that of nasal obstruction and crusting. The most common site of involvement was the septum and inferior turbinate.
Zeitlin et al. [9] in 2000 showed that 39% of 159 patients denied any kind of nasal symptoms. 23% of the patients had intermittent nasal symptoms that lasted less than 3 weeks and required continuous intervention with nasal steroids or use of normal saline solution. 38% of the patients were treated with nasal steroids and antibiotics for symptoms that lasted more than 3 weeks. Based on CT results, five patients underwent biopsy, which confirmed sarcoidosis.
Long et al. [10] in 2001 reviewed six patients with pulmonary sarcoidosis who developed chronic sinonasal disease. All six patients had intranasal finding consistent with sinonasal sarcoidosis, but only four had histological evidence of sinonasal sarcoidosis.
A study on 62 patients done by Meybeck et al. [11] in 2004 revealed only nasal symptom in 38 patients and an abnormality of the CT scan in 70% of cases. Rhinoscopy revealed a mucosal lesion in 11 cases. The presence of mucosal nodules on the turbinates was suggestive of sarcoidosis and was proven histologically in four cases (6.5%). In these four cases there were symptoms of nasal sinus involvement and extensive CT changes.
Braun et al. [12] in 2004 presented a retrospective study of 15 biopsy-proven sinonasal sarcoidosis. Pulmonary sarcoidosis was associated in 12 cases. Radiological studies showed nodules on the septum and/or the turbinates in 14 cases and complete or subtotal opacification of the sinuses and/or the nasal cavities in 13 cases. These were thus proposed as one of the diagnostic criteria for diagnosis of sinonasal sarcoidosis.
A study of 20 patients done by Aubart et al. [13] in 2006 showed that sinonasal involvement occurred in the course of previously known sarcoidosis in eight patients, whereas it preceded disease diagnosis in 12 patients.
Table 4 presents an overview of literature commented on above.
One of our cases—case I—presented with a nasal deformity with involvement of nasal bones, which is extremely rare (Fig. 5). Systemic steroids in this case have successfully treated the nasal deformity. However, the patient is still in the need of systemic steroid therapy. She receives 20 mg Prednisolone every other day to avoid remission.
Nasal deformity secondary to sarcoidosis has been described by Scott et al. [17] in 1992 and by Gürkov and Berghaus [18] in 2009. It is advised that rhinoplasty in patients with nasal deformity secondary to sarcoidosis should only be performed when the disease is quiescent.
In 1990 Milford et al. [19] described that the external nasal deformity—which is primarily confined to the skin—may resolve in time with adequate medical treatment.
Schikowitz et al. [20] in 1993 underlined that involvement of nasal bones and subcutaneous tissues is the least common manifestation of sarcoidosis, but can lead to swelling and widening of the nasal bridge.
In case I of this study (Fig. 6), the nasal bones were found to be involved with sarcoidosis that resulted in cosmetic deformity, the mucosa and the soft tissues of the nose being normal. Surgery in this case was performed only for diagnostic purpose. No cosmetic surgery has been performed due to lack of total remission.
Involvement of nose and paranasal sinuses in sarcoidosis is uncommon and involvement as presenting manifestations is rare. Among our cases four patients presented with nasal symptoms and the other three developed nasal and sinus symptoms after the diagnosis of sarcoidosis was confirmed. In our group four patients (case II, V, VI and VII) underwent endonasal endoscopic sinus surgery, which was mandatory for the outcome in these patients. We regard limited well-controlled intranasal operative procedures of vital importance in the treatment of sinonalsal manifestations. Kay and Har-El [21] in 2001 also underlined the role of endonasal sinus surgery in sinonasal sarcoid.
We conclude that treatment of sarcoidosis depends upon the site and extent of the disease. Systemic manifestations such as pulmonary involvement require the use of oral corticosteroids or low-dose methotrexate. Intranasal steroids can be used for nasal sarcoidosis often requiring intermittent systemic steroids. Sinus drainage procedures may be necessary in the management of acute or chronic sinusitis unresponsive to medical treatment.
References
Nunes H, Bouvry D, Soler P, Valeyre D (2007) Review sarcoidosis. Orphanet J Rare Dis 2:48
Aladesanmi OA (2004) Sarcoidosis: an update for the primary care physician. Med Gen Med 6(1):7
Baughman RP, Lower EE, du Bois RM (2003) Sarcoidosis. Lancet 361:1111–1118
Costabel U (2001) Sarcoidosis: clinical update. Eur Respir J 18(Suppl. 32):56–68
McCaffrey TV, McDonald TJ (1983) Sarcoidosis of the nose and paranasal sinuses. Laryngoscope 93(10):1281–1284
Wilson R, Lund V, Sweatman M, Mackay IS, Mitchell DN (1988) Upper respiratory involvement in sarcoidosis and its management. Eur Respir J 1(3):269–272
Shah UK, White JA, Gooey JE, Hybels RL (1997) Otolaryngologic manifestations of sarcoidosis: presentation and diagnosis. Laryngoscope 107:67–75
Fergie N, Jones NS, Havlat MF (1999) The nasal manifestation of sarcoidosis: a review and report of eight cases. J Laryngol Otol 113:893–898
Zeitlin JF, Tami TA, Baughman R, Winget D (2000) Nasal and sinus manifestations of sarcoidosis. Am J Rhinol 14(3):157–161
Long CM, Smith TL, Loehrl TA, Komorowski RA, Toohill RJ (2001) Sinonasal disease in patients with sarcoidosis. Am J Rhinol 15(3):211–215
Meybeck A, Just N, Heurtebise F, Chanez P, Crampette L, Darras J, Wallaert B, Groupe de travail “nez-Bronches” de la SPLF (2004) Involvement of nasal sinuses in sarcoidosis. A prospective study of 63 patients. Rev Mal Respir 21(2 Pt 1):279–286 Article in French
Braun JJ, Gentine A, Pauli G (2004) Sinonasal sarcoidosis: review and report of fifteen cases. Laryngoscope 114:1960–1963
Aubart FC, Quayoun M, Brauner M, Attali P, Kambouchner M, Valeyre D, Nunes H (2006) Sinonasal involvement in sarcoidosis: a case-control study of 20 patients. Medicine (Baltimore) 85(6):365–371
Mrowka-Kata K, Kata D, Lange D, Namyslowski G, Czecior E, Banert K (2010) Sarcoidosis and its otolaryngological implications. Eur Arc Otorhinolaryngol 267:1507–1514
Baudin B (2005) Angiotensin I-converting enzyme (ACE) for sarcoidosis diagnosis [Article in French]. Pathol Biol (Paris) 53(3):183–188
Sharma OP (2005) Renal sarcoidosis and hypercalcemia. Eur Respir Monograph 10:220–232
Scott PMJ, Morphopoulous G, Bleach N (1992) Augmentation rhinoplasty in nasal sarcoidosis. J Laryngol Otol 106:544–546
Gürkov R, Berghaus A (2009) Nasal reconstruction in advanced sinunasal sarcoidosis. Rhinology 47(3):327–329
Milford CA, Mugliston T, Lund VJ (1990) “Medical rhinoplasty” in nasal sarcoidosis. Rhinology 28:137–139
Schikowitz MJ, Alvy A (2003) Sarcoidosis presenting as nasal obstruction. Am J Rhinol 7:133–138
Kay DJ, Har-El G (2001) The role of endoscopic sinus surgery in chronic sinonasal sarcoid. Am J Rhinol 15:249–254
Conflict of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gulati, S., Krossnes, B., Olofsson, J. et al. Sinonasal involvement in sarcoidosis: a report of seven cases and review of literature. Eur Arch Otorhinolaryngol 269, 891–896 (2012). https://doi.org/10.1007/s00405-011-1778-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-011-1778-5