Abstract
The pathomechanism of chronic rhinosinusitis with nasal polyposis (CRS/NP) seems to be unclear. Bacterial-, fungal- and combined biofilms might play a potential role in the pathogenesis of various inflammatory diseases and recently in CRS/NP. A prospective, blinded observational study was performed to confirm that the combination of conventional hematoxylin–eosin (HE) and Gram staining protocols could be used to detect bacterial and fungal biofilms in patients with CRS/NP. A total of 50 patients with CRS/NP undergoing endoscopic sinus surgery (ESS) were analyzed. The negative control group consisted of 12 patients undergoing septoplasty for nasal obstruction without CRS/NP. The nasal polyps and inferior turbinate mucosa specimens applied as negative controls were processed to HE and Gram staining. Biofilm was detected in 44 of 50 patients with CRS/NP and in none of 12 negative controls. In our series, HE method showed an obvious correlation with the results of Gram staining and was allocated to be a good predictor of biofilm existence. It was found that the microscopic structure and thickness of biofilms were strongly associated with the integrity of nasal mucosa and with the characteristics of subepithelial cellular infiltration. This study confirmed the presence of bacterial and fungal biofilms on the surface of NPs obtained from patients with CRS. Since biofilms may affect the severity and recurrence rate of CRS treated by ESS they should be detected histologically. In conclusion, HE staining combined with Gram protocol is a robust and reliable method for the detection of bacterial and fungal biofilms in CRS/NP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic rhinosinusitis (CRS) is a common inflammatory disease in ENT practice that is responsible for a great amount of medical visits and one of the main reasons for antibiotic treatment and leave of work [1]. Diagnosis of CRS is based on the duration of symptoms (nasal obstruction, hyposmia, discharge and pain), which persist over 12 weeks [1]. CRS can be classified into two main groups depending on the presence or absence of nasal polyps (NP) [1]. CRS with NP is a separate diagnostic entity, although the etiopathogenesis is still unclarified [1, 2]. Several hypotheses have been raised in the explanation of the pathogenesis of CRS, which is currently thought to be an immunological disease affected by multiple factors [1]. These are immunological disorders, allergic rhinitis, asthma, aspirin intolerance, Staphylococcus superantigens, fungal infections and the presence of different biofilms [1, 2].
Bacterial and fungal biofilms have been implicated in the pathogenesis of various chronic inflammatory diseases, which affect mucosal surfaces [3–5]. This group of infectious diseases includes chronic tonsillitis, adenoiditis, CRS, chronic otitis media and periodontitis [3, 6]. Furthermore, presence of bacterial biofilms has been reported on the surface of different surgical implants [3, 7]. Being infectious agents, bacterial and fungal colonies exist in two main forms: as free planktonic prokaryote or eukaryote cells or as complex biofilms [3–5, 8]. Biofilms are the primary structures of bacterial or fungal survival and proliferation, which are characterized by a self-produced three-dimensional extracellular matrix that consists of polysaccharides, proteins and nucleic acids [3, 9]. Bacterial biofilms are characterized by extremely high resistance against antibiotics and host immune reactions [3]. This resistance mechanism is associated with the physical barrier formed by the polysaccharide matrix that blocks the diffusion of antibiotics, superoxides, immunglobulins and opsonins [2, 3]. Biofilms can be formed by individual or mixed species of bacteria and fungi as well as Staphylococcus aureus and epidermidis, Pseudomonas aeruginosa, Streptococcus pneumoniae, Candida albicans, Candida crusei and Aspergillus niger [3–5, 9]. Usually, they are cannot be cultured and isolated by conventional microbiological protocols; therefore diagnosis is often uncertain [10].
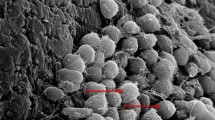
Biofilms can be detected by difficult, expensive and time-consuming protocols of scanning electron microscopy (SEM), transmission electron microscopy (TEM), confocal laser scanning microscopy (CLSM) and recently by fluorescent in situ hybridization (FISH) [11–13]. In 2010, Hochstim et al. [13] have reported a reliable and robust method for biofilm detection that was based on the conventional HE staining of fresh surgical specimens obtained from patients with CRS/NP13. These authors have compared their results with FISH analysis and found a full correspondence between the two protocols [13]. Since biofilms are thought to play a crucial role in the pathogenesis of CRS/NP, our aim was to provide a rapid, cheap, roboust and reliable method for bacterial-, fungal or combined biofilm detection.
This study investigates the presence and microscopic features of bacterial-, fungal- and combined biofilms on the surface of NP obtained from patients with CRS. Biofilm characteristics were compared with the subepithelial infiltration and inflammatory cell types. To our knowledge, this is the first comprehensive study, which confirms the availability of combined HE and Gram staining in the histological diagnosis of biofilms.
Materials and methods
Patients and controls
We performed a prospective blinded observational study of nasal polyps obtained from patients with CRS/NP who underwent ESS at the Department of Otorhinolaryngology and Head and Neck Surgery, University of Debrecen. Nasal polyps were collected between February 2010 and January 2011. The group of patients consisted of 28 women and 22 men (n = 50, mean age = 49.4 years; range = 4–69 years) with the diagnosis of CRS/NP confirmed by nasal endoscopy and computed tomography (CT) scan of paranasal sinuses. After the coronal plane reconstruction, CT scans were examined and scored by the Lund-Mackay staging protocol. The clinical history and findings of physical examinations were obtained during confirmation of the diagnosis of CRS/NP. Clinical information on bronchial asthma, allergic rhinitis, aspirin intolerance, previous ESS, topical steroid treatment and systemic antimicrobial therapy was recorded before surgery. All the nasal polyps collected during ESS were processed to histopathological analysis. Only large nasal polyps (>2 cm) were analyzed, which could be removed by a cold device (straight ESS forceps) without any surface injury or iatrogenic disruption of biofilm layers. The removal was gently performed at the root of the nasal polyps. Twelve patients (n = 12; men = 8; women = 4; mean age = 37.2 years) scheduled for septoplasty for nasal obstruction without a medical history of CRS were recruited into the negative control group. Tissue specimens of approximately 0.5 cm3 were obtained from the anterior mucosal surface of the inferior turbinate. All of the patients gave their informed consent before donating their tissue samples for the study. We obtained Institutional Ethical Committee (DE OEC-EB/2009/12) approvals. Patients gave their informed consents. The study was carried out according to the Declaration of Helsinki.
Histopathological analysis
A total of 62 nasal mucosa specimens were fixed in 10% (w/v) formaldehyde. Specimens were embedded in 15% (w/v) purified gelatin (24 h, 56°C) and refixed in 4% (w/v) paraformaldehyde (24 h, 20°C). Blocks were cryoprotected in 20% (w/v) saccharose solution (2 h, 4°C) and sectioned into 10-μm slides at −25°C (MNT-200, Slee, Mainz, Germany). Slides were stored in 0.1 M PBS containing 0.03% (w/v) sodium azide at 4°C. Two consecutive 5-μm frozen cut sections were examined as follows: (1) conventional staining with HE; and (2) conventional Gram staining. Histological examinations were blinded for two independent researchers: P.Cs. analyzed the sections stained by HE, while T.K. examined the Gram staining results. The criteria for the histopathological classification of bacterial and also fungal or combined biofilms were the presence of characteristic morphology and Gram positivity/negativity and micro colonies for examination by optical microscopy and the presence of the surrounding polysaccharide layer. Biofilms were classified into three groups based on their integrity and thickness: (1) fragmented (0–10 μm); (2) complete (<10 μm); and (3) bulky (>10 μm). Structure and cellular infiltration of epithelial- and also the stromal (subepithelial) layers were correlated to the presence or absence of bacterial or fungal biofilms.
Results
Altogether fifty patients with CRS/NP who underwent ESS were included in this study. Eleven patients (22%) had bronchial asthma, seven patients (14%) had allergic rhinitis and three (6%) diagnosed with aspirin intolerance. In our series, only one patient had ASA triad (a.k.a Samter’s triad: nasal polyposis, bronchial asthma, and aspirin intolerance). The Lund-Mackay scores of coronal reconstructed CT scans varied between 7 and 24 with an average score of 19 indicating serious involvement of paranasal sinusis by CRS. The score was higher than 19 in 60% of patients (n = 30). Repeated ESS was performed in 38% (n = 19) of patients, which is an important predictive factor of CRS recurrence. In this group, number of previous surgeries varied between 1 and 13 with an average number of 3 ESS. All patients were treated by topical steroid (momethasone-furoate, beclomethason) therapy before surgery. Preoperative, systemic antibiotic treatment was performed in 13 (26%) patients. Table 1 summarizes the clinical history of patients with CRS/NP.
Histopathological examination revealed inflammatory nasal polyps with lymphocytic (LPC), eosinophilic and polymorphonuclear (PMN) infiltration of the subepithelial stroma in all cases. Bacterial-, fungal- or combined bioflims were detected in 44 (88%) of 50 patients with CRS/NP (Table 2). In the biofilm-negative cases (n = 6, 12%), histopathological analysis revealed a regular respiratory mucosa with predominantly eosinophil infiltration of the subepithelial layer (Fig. 1, Table 2). All the six biofilm-negative cases were originated from patients diagnosed with allergic rhinitis (Table 1). In our series, HE staining showed a strong correlation with the results of Gram staining and was found to be a reliable predictor of the presence or absence of biofilms. No discrepancies were found between the two staining protocols (Table 2). In the biofilm-positive specimens, the microscopic structure and thickness of biofilms were strongly associated with the histopathological characteristics of nasal mucosa and also to the dominant inflammatory cell type of the subepithelial layer (Tables 2, 3). It was found that normal respiratory mucosa with columnar ciliated epithelium is not associated with the presence of different types of biofilms (Fig. 1, Table 3). Disintegration or squamous cell metaplasia of the nasal mucosa due to the subepithelial inflammatory reactions was strongly associated with the presence of bacterial or fungal biofilms (Figs. 2, 3, 4, Table 3). It was found that LPC or PMN infiltrations of the subepithelial (stromal) layer are the most important predictors of biofilm presence (Figs. 2, 3, 4, Table 3). In contrast, predominant eosinophil infiltration decreased the chance of biofilm detection (Figs. 2, 3, 4, Table 3). In the 44 CRS/NP specimens, 25 bacterial, 8 fungal and 11 combined biofilms were detected, obviously correlated to the thickness of the biofilm itself (Figs. 2, 3, 4, Table 2). Combined fungal-bacterial biofilms were predominantly detected in bulky layers (Table 2). No biofilm-like structures were detected in mucosal specimens obtained from the inferior turbinate of patients (N = 12) applied as negative controls (Fig. 5).
Histopathological representation of a nasal polyp. a At low magnification, regular columnar epithelium and foamy cells can be detected (black arrow). Basal lamina is indicated by green arrow. The green star shows the subepithelial layer. b The subepithelial layer is infiltrated by plasmocytes and small lymphocytes (green arrows). c Biofilm structures cannot be detected on the surface of nasal epithelium (black arrow). Basal lamina is a well-identified structure (green arrow). d Gram staining is negative for bacterial or fungal elements; the polysaccharide matrix is absent (black arrow)
Histopathological examination of a CRS/NP specimen. a The nasal epithelium is destructed and massively infiltrated by inflammatory cells. The stromal layer shows a gland-like structure. b The subepithelial layer is infiltrated by eosinophils (green arrow) and polymorphonuclear cells (white arrow). c The epithelial layer is absolutely disintegrated and covered by a complete biofilm showing a homogeneous basophilic staining (black arrow). d Gram staining reveals a combined biofilm consisting of individual colonies of Gram-negative fungi and Gram-positive cocci (small inserts)
Histopathological examination of a nasal polyp. a The nasal epithelium is destroyed and infiltrated by lymphocytes; however, it shows some columnar structure (black arrow). A fragmented biofilm layer is indicated by green arrow. b The subepithelial layer is seriously infiltrated by lymphocytes. c The black arrow indicates the incomplete biofilm layer. d Gram staining reveals a combined bacterial biofilm consisting of individual colonies of Gram-positive cocci and Gram-negative bacilli (small inserts)
Histopathological analysis of a nasal polyp. a The nasal epithelium shows a squamous cell metaplasia (black arrow). A bulky and continuous biofilm layer can be identified on the surface of the epithelial layer (green arrow). b The subepithelial layer is predominantly infiltrated by eosinophil granulocytes (green arrow). c At higher magnification of the previous slides, the thickened biofilm layer can be identified as a homogeneous structure showing intense basophilic staining by H&E (green arrow). The nasal epithelium shows a total squamous cell metaplasia with increased numbers of choilocytes (white arrow). d Gram staining indicates a bacterial biofilm consisting of confluent colonies of Gram-positive cocci (small insert)
Histopathological representation of a control specimen obtained from the inferior turbinate. a At low magnification, a tenuous respiratory mucosa (black arrow) and a stromal layer showing glandular structure (green star) can be detected (black arrow). b The subepithelial layer is consisted of small glandules covered by uniform epithelial cells (green arrow). c Biofilm structures cannot be detected on the surface of nasal epithelium (black arrow). d Gram staining is negative for bacterial or fungal elements; the polysaccharide matrix is absent (black arrow)
Discussion
CRS/NP is a disease of multifactorial agents involving disturbed local immune response and chronic inflammation; however, bacterial or fungal biofilms might contribute to the damage of respiratory epithelium and subsequent hyperplasia of the subepithelial layer infiltrated by inflammatory cells [14, 15]. Local steroids and systemic antibiotic treatment might have severe influence on the flora of nasal cavity and paranasal sinuses, and in fact these medications might affect the structure and thickness of biofilms. Since our patients were all treated by local steroids (momethasone-furoate, beclomethasone), this association seems to be very strong. In contrast, biofilm-negative specimens were obtained from patients with allergic rhinitis who were regular local steroid users. Furthermore, alergic rhinitis is not a real risk factor for CRS/NP by the current rhinologic consensus [1, 2]. In the future, placebo-controlled, double blinded, dynamic studies will be neccessary to prove this causative relation and to dissolve this conflict.
In the present study, we demonstrated the presence of bacterial-, fungal- or co-existing biofilms in 44 patients with CRS/NP by the combined application of HE and Gram staining. Results of HE staining showed a full correspondence to Gram staining in detection of different biofilms. Furthermore, the failure to detect biofilms was not associated with the single application of HE staining. In the light of these results, we do think that combination of HE and Gram staining protocols should be emphasized, since HE staining is for the investigation of tissue layers and their microscopic architecture while Gram protocol stains bacilli, cocci and fungal elements.
We did not intend to make a precise identification of bacterial or fungal species, because the presence of biofilm itself is thought to be the most important factor in the pathogenesis of CRS/NP [2, 14, 15]. Furthermore, persisting biofilms in CRS/NP cases may be responsible for surgical failures and high recurrence rate of disease [1, 2]. Microbiological identification of distinct infectious agents involved in biofilm formation still requires culturing or FISH analysis with species-specific oligonucleotide probes [11–13].
There is increasing evidence that biofilms play a crucial role in several chronic inflammatory diseases [3, 6, 7, 10]. Therefore, it is plausible to introduce an easy, reliable and cheap method to identify biofilms in CRS/NP specimens. In concurrence with Hochstim et al. [13], we confirmed that the wide availability of HE and Gram staining of surgical specimens through clinical histopathology laboratories makes this a reliable method for detection of biofilms in the clinical practice [13]. Although specific treatments are not available to target biofilms, it is very important to be detected, since it is strongly associated with treatment failure and persisting symptoms [1, 2, 14, 16]. In general, therapeutic considerations can be divided into two main groups: blockade of biofilm formation and eradication of biofilms that have already formed [1, 2, 16].
In conclusion, further examinations are required to clarify the etiologic role of biofilms in the pathogenesis of CRS/NP. Finally, introduction of reliable and robust methods for biofilm detection may contribute to new therapeutic options in the treatment of patients with CRS/NP.
References
Marple BF, Stankiewicz JA, Baroody FM, Chow JM, Conley DB, Corey JP, Ferguson BJ, Kern RC, Lusk RP, Naclerio RM, Orlandi RR (2009) Parker MJ; American Academy of Otolaryngic Allergy Working Group on Chronic Rhinosinusitis. Diagnosis and management of chronic rhinosinusitis in adults. Postgrad Med 121(6):121–139
Al-Mutairi D, Kilty SJ (2011) Bacterial biofilms and the pathophysiology of chronic rhinosinusitis. Curr Opin Allergy Clin Immunol 11(1):18–23
Suh JD, Ramakrishnan V, Palmer JN (2010) Biofilms. Otolaryngol Clin North Am 43(3):521–530
Foreman A, Psaltis AJ, Tan LW, Wormald PJ (2009) Characterization of bacterial and fungal biofilms in chronic rhinosinusitis. Am J Rhinol Allergy 23(6):556–561
Healy DY, Leid JG, Sanderson AR, Hunsaker DH (2008) Biofilms with fungi in chronic rhinosinusitis. Otolaryngol Head Neck Surg 138(5):641–647
Mladina R, Skitarelić N, Musić S, Ristić M (2010) A biofilm exists on healthy mucosa of the paranasal sinuses: a prospectively performed, blinded, scanning electron microscope study. Clin Otolaryngol 35(2):104–110
Perloff JR, Palmer JN (2004) Evidence of bacterial biofilms on frontal recess stents in patients with chronic rhinosinusitis. Am J Rhinol 18(6):377–380
Zernotti ME, Angel Villegas N, Roques Revol M, Baena-Cagnani CE, Arce Miranda JE, Paredes ME, Albesa I, Paraje MG (2010) Evidence of bacterial biofilms in nasal polyposis. J Investig Allergol Clin Immunol 5:380–385
Foreman A, Wormald PJ (2010) Different biofilms, different disease? A clinical outcomes study. Laryngoscope 120(8):1701–1706
Ferguson BJ, Stolz DB (2005) Demonstration of biofilm in human bacterial chronic rhinosinusitis. Am J Rhinol 19(5):452–457
Mladina R, Poje G, Vuković K, Ristić M, Musić S (2008) Biofilm in nasal polyps. Rhinology 46(4):302–307
Psaltis AJ, Ha KR, Beule AG, Tan LW, Wormald PJ (2007) Confocal scanning laser microscopy evidence of biofilms in patients with chronic rhinosinusitis. Laryngoscope 117(7):1302–1306
Hochstim CJ, Choi JY, Lowe D, Masood R, Rice DH (2010) Biofilm detection with hematoxylin-eosin staining. Arch Otolaryngol Head Neck Surg 136(5):453–456
Hekiert AM, Kofonow JM, Doghramji L, Kennedy DW, Chiu AG, Palmer JN, Leid JG, Cohen NA (2009) Biofilms correlate with TH1 inflammation in the sinonasal tissue of patients with chronic rhinosinusitis. Otolaryngol Head Neck Surg 141(4):448–453
Galli J, Calò L, Ardito F, Imperiali M, Bassotti E, Passali GC, La Torre G, Paludetti G, Fadda G (2008) Damage to ciliated epithelium in chronic rhinosinusitis: what is the role of bacterial biofilms? Ann Otol Rhinol Laryngol 117(12):902–908
Young D, Morton R, Bartley J (2010) Therapeutic ultrasound as treatment for chronic rhinosinusitis: preliminary observations. J Laryngol Otol 124(5):495–499
Acknowledgments
This work was supported by the grants from Hungarian Scientific Research Fund (OTKA PD75371) and from Mecenatúra Fund of Debrecen University (DE OEC Mec 17/2008).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tóth, L., Csomor, P., Sziklai, I. et al. Biofilm detection in chronic rhinosinusitis by combined application of hematoxylin-eosin and gram staining. Eur Arch Otorhinolaryngol 268, 1455–1462 (2011). https://doi.org/10.1007/s00405-011-1623-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-011-1623-x