Abstract
This retrospective study aimed to assess the role of salvage surgery for local recurrence in hypopharyngeal cancer (HPC) patients who had received radiotherapy (RT) or concomitant chemoradiotherapy (CRT) as an initial treatment. The local recurrence rate, salvage rate after local recurrence and overall survival rate were investigated in 104 HPC patients who received treatment between 1991 and 2005. Local recurrence in the primary site was observed in 41 patients (rate, 39.4%) of whom only 12 could undergo further salvage surgery. Disease control was achieved in seven of these patients (successful salvage rate, 17.1%). The 5-year overall survival rate was 40.6% in the RT/CRT patient group and successful salvage rates for T1, T2, T3 and T4 primary disease were 33.3% (1/3), 20.0% (4/20), 16.7% (2/12) and 0% (0/6), respectively. Severe postoperative complications such as pharyngo-cutaneous fistula were seen in six patients (50.0%). Prognosis of patients with locally recurring HPC after RT/CRT is poor at any primary T-stage and the incidence of postoperative complication is relatively high. This should be taken into consideration when the initial treatment plan is decided and the choice of salvage surgery for such recurrent cases should be carefully determined.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite improvements in surgery, radiotherapy and chemotherapy, hypopharyngeal cancer has one of the worst prognoses of head and neck malignant diseases. Recent studies have documented the effectiveness of concomitant chemotherapy with radiation (CRT) for both survival benefits and organ preservation in head and neck cancer [1]. The addition of concomitant treatments, such as single or multi-agent chemotherapy, molecular-targeted agents [2, 3] and superselective arterial infusion [4], as an adjuvant to radiotherapy is becoming more prevalent and its survival benefit is now comparable to that of definitive surgery [5, 6]. Consequently, the role of surgical treatment is shifting to salvage therapy after the primary treatment based on radiotherapy. However, recurrent diseases tend to be more invasive and salvage surgery is often technically difficult and offers a poor prognosis [7]. Functional sacrifice due to surgical salvage of the primary site and postoperative complications often diminish the quality of life, so the decision to perform salvage surgery for locally recurring head and neck cancer remains controversial.
In this study, we assessed the role of salvage surgery in hypopharyngeal cancer by retrospectively analyzing patient outcomes of salvage surgery for local recurrence after RT/CRT as a primary treatment.
Patients and methods
We used medical records to retrospectively analyze 104 patients with previously untreated resectable HPC who received RT or CRT at Hokkaido University Hospital, Sapporo, Japan, for 14 years from 1991 to 2005. Patient characteristics are shown in Table 1. Most patients were male (n = 97, 93.3%) with an age range from 38 to 86 years (median 63 years) and a median follow-up time of 21 months (mean 27.8 months). No unresectable cases were included in this study.
All pathological findings were of squamous cell carcinoma. Seventeen patients had T1 primary tumors, 46 had T2, 27 had T3 and 14 had T4. The rates for lymph node metastasis were 52.9% with T1, 63.0% with T2, 85.2% with T3 and 85.7% with T4 (Table 2). The local recurrence rate, salvage rate after local recurrence and overall survival rate for these patients were investigated. Survival rate was analyzed by using the Kaplan–Meier’s estimate.
Table 3 shows the initial treatment breakdown of patients. Of the 104 patients, 32 received conventional RT of 62–70 Gy alone and 72 received RT with concomitant chemotherapy. These regimens consisted of weekly treatment with carboplatin (AUC = 1–2), i. v. docetaxel (10 mg/m2) or a daily low dose of cisplatin (4 mg/m2). Patients who were treated with weekly cisplatin (100–120 mg/m2) received this by arterial infusion. When the local or regional recurrence was detected during the follow-up after initial treatment of RT or CRT, appropriate surgical treatment such as laryngopharyngectomy or neck dissection was conducted depending on recurrent tumor state.
As a reference, we also analyzed the outcomes of the patients who were initially treated with definitive surgery (n = 58) during the same period (surgery group). In this group, the patient distribution of primary disease consisted of 2 patients of T1 tumor, 23 of T2, 23 of T3 and 11 of T4.
Results
Survival
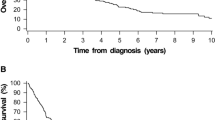
For the 37 of the 104 patients, any of recurrent disease had not been detected after initial treatment of RT or CRT during the follow-up period. They were able to have oral intake without feeding tube support and no patient had tracheostoma. The local recurrence in the primary site was observed in 41 patients (local recurrence rate, 39.4%) of whom only 12 could undergo further salvage surgery and the remaining 29 could not receive salvage surgery (Fig. 1). The 5-year overall survival rate of all patients was 40.6% for the all 104 patients (Fig. 2). Salvage surgery for recurrent primary disease achieved preservation of the larynx in four patients, one by endoscopic mucosal resection and three partial resections because of early detection of local recurrence. The remaining eight patients required laryngopharyngectomy. Eleven of the 12 patients who underwent salvage surgery needed to receive unilateral or bilateral neck dissection.
Of the 41 patients, recurrences were seen in 30 patients with tumors of the pyriform sinus, five of the postcricoid region and six of the posterior wall. Salvage surgery was performed on nine (30.0%) patients with recurrences in the pyriform sinus, two (40.0%) in the postcricoid region, and one (16.7%) in the posterior wall (Table 4). Successful salvage rates for each subsite were 16.7% for the pyriform sinus, 40.0% for the postcricoid region, and 0.0% for the posterior wall. Disease control was achieved in seven patients who underwent salvage surgeries (successful salvage rate, 17.1%). Table 5 shows successful salvage rates for each T-stage.
Survival curves after local recurrence are shown in Fig. 3. The 5-year Kaplan–Meier overall survival rate after recurrence was 19.2% among 41 patients, and overall survival rates were 57.1% with salvage surgery (n = 12) and 3.5% among those who could not receive salvage surgery (n = 29).
In the surgery group, primary disease could be controlled by partial resection of pharynx preserving larynx for three patients. Total laryngopharyngectomy with or without reconstruction was done for 55 patients. Five-year overall survival rate of the surgery group was 45.2%. Of these, radiotherapy was performed on 37 patients preoperatively and 2 postoperatively. The survival rates for each T-stage were 100% for T1, 48.2% for T2, 56.2% for T3 and 28.3% for T4, respectively. There was no statistical difference of survival rates for each T-stage between RT/CRT group and surgery group.
Postoperative complications
Postoperative complications were seen in six patients (50.0%). Pharyngo-cutaneous fistulas occurred in two of the eight patients who underwent laryngopharyngectomy (25%). A fistula closed without surgery after 2 months but the other needed surgical reconstruction to close. Prolonged wound healing in the neck without fistula also occurred in 2 of the 11 patients, including those patients who underwent neck dissection. The aspiration pneumonia occurred on one patient who received the partial resection of hypopharynx and he finally underwent glottic closure. Peritonitis in the donor site of the free jejunum graft was also observed in one patient.
Discussion
HPC has one of the worst prognoses of all head and neck tumors and a low survival rate, making the choice of treatment difficult. Recent changes in CRT have contributed to improvements in functional organ preservation, but successful locoregional control does not always increase survival rates. It has been reported that the feasibility of salvage therapies following tumor recurrence is generally low [7, 8].
In our series, the local recurrence rate of HPC was 43.7% in patients with T2–4 disease after treatment with RT/CRT, and 17.6% in those with T1 disease. When the recurrence became unequivocal, most T3 and T4 patients were considered unsuitable to receive surgical salvage. Only two of 18 patients (11.1%) who experienced local recurrence with an initial diagnosis of T3 or T4 achieved long-term survival after salvage surgery, with 15 of the 18 not even having the chance to undergo salvage surgery. All T4 patients died within 19 months after the local recurrence was detected.
Even in those with early stage (T1 or T2) tumors, disease control was successful in only 6 of 23 (26.1%) with local recurrence. In total, 70.7% of locally recurrent HPC patients were unable to receive salvage surgery. In addition, the chance for salvage surgery was more limited in patients with tumors in the primary posterior wall because of difficulties in early detection. However, the statistical analysis did not indicate a significant difference because of the low frequency of posterior wall and postcricoid tumor types. Therefore, the initial T-stage and tumor subsite are important factors that affect the indication of HPC salvage surgery.
Laryngeal cancer, by contrast, offers more chance to undergo salvage surgery for recurrence. Leon et al. [9] reported that 25 of 34 patients (73.5%) received salvage surgery for local or locoregional recurrence, and their 5-year survival rates ranged from 43 to 45% for T3 or T4 laryngeal cancer (compared with 19.2% for HPC in our data). Stoeckli et al. also reported performing salvage surgery for 39 of 44 recurrent laryngeal cancer patients, compared with 15 of the 33 recurrent HPC cases [10]. Although the hypopharynx and larynx are adjacent to each other, the results of salvage treatment are so distinct that the treatment strategy for these two cancers should not be the same. These differences should be considered when deciding on the primary treatment plan.
Some studies report an acceptable frequency of postoperative complications such as pharyngo-cutaneous fistulas after CRT [8, 9]. Even with high-dose intra-arterial infusion of cisplatin, Proctor et al. [11] found that postoperative complications were not significantly worse than those encountered during primary surgery. On the other hand, Clark et al. [12] showed that irradiation increased the incidence of postoperative pharyngo-cutaneous fistula from 24 to 38%, while Wakisaka et al. [13] noted that although the frequency of pharyngo-cutaneous fistula after RT or CRT was not high, fistula closure tended to be delayed. In the present study, we experienced severe postoperative complications including pharyngo-cutaneous fistulas in 25% of patients who underwent laryngopharyngectomy. Such complications could severely diminish the quality of life for patients.
As the treatment outcomes for the survival of CRT are not superior to those of definitive surgery, the latter should remain a treatment option for patients pursuing a higher chance of survival rather than organ preservation. The CRT survival rate of the present study was 40.6%, while that of the definitive surgery group (n = 58) was 45.2% during the same period of comparison in our institute. This difference was not statistically different (Wilcoxon’s rank test). CRT has become increasingly popular over the past decade, but it is difficult to make great improvements to successful salvage by advances on surgical technique. On this basis, we recommend surgical salvage for local failure of HPC in patients with good performance status and potentially resectable recurrent tumors; this decision should be made after careful consideration and unless there are no other options for such patients.
Conclusion
To assess the role of salvage surgery for failure cases of HPC who underwent RT/CRT as an initial treatment, we retrospectively analyzed the outcomes of salvage surgery for such recurrent cases. We demonstrated that it is difficult to salvage locally recurrent HPC, especially at more advanced T-stages or when tumors recur on the posterior wall. The limited effects of surgical salvage for recurrent HPC need to be addressed when choosing the initial treatment plan for HPC.
References
Pignon JP, le Maître A, Maillard E, Bourhis J, MACH-NC Collaborative Group. (2009) Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): an update on 93 randomised trials and 17, 346 patients. Radiather Oncol 92(1):4–14
Bernier J, Schneider D (2007) Cetuximab combined with radiotherapy: an alternative to chemoradiotherapy for patients with locally advanced squamous cell carcinomas of the head and neck? Eur J Cancer 43:35–45
Bernier J (2008) A multidisciplinary approach to squamous cell carcinomas of the head and neck: an update. Curr Opin Oncol 20:249–255
Robbins KT, Vicario D, Seagren S, Weisman R, Pellitteri R, Kerber C, Orloff L, Los G, Howell SB (1994) A targeted supradose cisplatin chemoradiation protocol for advanced head and neck cancer. Am J Surg 168:419–422
Soo K-C, Tan E-H, Wee J, Lim D, Tai B-C, Khoo M-L, Goh C, Leong S-S, Tan T, Fong K-W, Lu P, See A, Machin D (2005) Surgery and adjuvant radiotherapy vs concurrent chemoradiotherapy in stage III/IV nonmetastatic squamous cell head and neck cancer: a randomised comparison. Br J Cancer 93:279–286
Bahadur S, Thakar A, Mohanti BK, Lal P (2002) Results of radiotherapy with, or without, salvage surgery versus combined surgery and radiotherapy in advanced carcinoma of the hypopharynx. J Laryngol Otol 116:29–32
Richey LM, Shores CG, George J, Lee S, Couch MJ, Sutton DK, Weissler MC (2007) The effectiveness of salvage surgery after the failure of primary concomitant chemoradiation in head and neck cancer. Otolaryngol Head Neck Surg 136:98–103
Lee SC, Shores CG, Weissler MC (2008) Salvage surgery after failed primary concomitant chemoradiation. Curr Opin Otolaryngol Head Neck Surg 16:135–140
Leon X, Quer M, Orus C, Lopez M, Gras JR, Vega M (2001) Results of salvage surgery for local or regional recurrence after larynx preservation with induction chemotherapy and radiotherapy. Head Neck 23:733–738
Stoeckli SJ, Pawlik AB, Lipp M, Huber A, Schmid S (2000) Salvage surgery after failure of nonsurgical therapy for carcinoma of the larynx and hypopharynx. Arch Otolaryngol Head Neck Surg 126:1473–1477
Proctor E, Robbins KT, Vieira F, Hanchett C, Sommes G (2004) Postoperative complications after chemoradiation for advanced head and neck cancer. Head Neck 26:272–277
Clark JR, de Almeida J, Gilbert R, Irish J, Brown D, Neligan P, Gullane PJ (2006) Primary and salvage (hypo) pharyngectomy: analysis and outcome. Head Neck 28:671–677
Wakisaka N, Murono S, Kondo S, Furykawa M, Yoshizaki T (2008) Post-operative pharyngocutaneous fistula after laryngectomy. Auris Nasus Larynx 35:203–208
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Taki, S., Homma, A., Oridate, N. et al. Salvage surgery for local recurrence after chemoradiotherapy or radiotherapy in hypopharyngeal cancer patients. Eur Arch Otorhinolaryngol 267, 1765–1769 (2010). https://doi.org/10.1007/s00405-010-1274-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-010-1274-3