Abstract
Parathyroid cysts are rare lesions that can present clinically as low neck masses. The clinical diagnosis of parathyroid cyst can be challenging and requires a high level of suspicion as it often mimics a thyroid nodule. The cyst occasionally can cause compressive symptoms such as dysphagia or dyspnea. When it occurs in the mediastinum, it can cause recurrent laryngeal nerve paralysis. In this report, we present a patient with a hyperfunctional parathyroid cyst in association with a papillary thyroid carcinoma. In addition, we briefly discuss the current literature on parathyroid cyst. This case is unusual in its clinical presentation in that the parathyroid cyst mimicked a thyroid goiter.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parathyroid cysts are rare lesions that can present clinically as cervical masses. Sandstrom was the first author to describe a parathyroid cyst in 1880 [11]. The first functioning mediastinal parathyroid cyst was surgically removed by Noble in 1936 [9]. Today, just over 300 cases have been reported in the world literature [7]. The clinical diagnosis of parathyroid cyst can be challenging and require a high level of suspicion as it often mimics a thyroid nodule. The cyst occasionally can cause compressive symptoms such as dysphagia or dyspnea. When it occurs in the mediastinum, it can cause recurrent laryngeal nerve paralysis.
In this report, we describe a patient with a hyperfunctional parathyroid cyst in association with a papillary thyroid carcinoma. In addition, we briefly discuss the current literature on parathyroid cyst. This case is unusual in its clinical presentation in that the parathyroid cyst appeared to be a thyroid goiter.
Case report
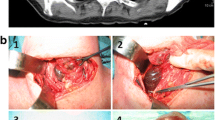
A 76-year-old man was admitted to the hospital in August 2005 for back surgery. During the hospital stay, a barium esophogram was performed because of dysphagia, which revealed an extrinsic mass narrowing the esophagus. A computed tomography (CT) of the neck revealed a left thyroid lobe mass with retrosternal extension and mild tracheal and esophageal compression (Fig. 1). An ultrasound of the neck revealed a 7.7 × 3.8 × 2.9 cm left lobe with a 4.9 × 3.3 × 2.7 cm, dominant, hypoechoic nodule extending into the retrosternal and supraclavicular regions. An additional complex cystic nodule in the left upper pole was noted measuring 1.5 × 1.7 × 1.8 cm.
A fine-needle aspiration of the dominant nodule was attempted, but the results were not conclusive. His thyroid function tests performed at the time were within normal limits with a TSH of 2.1 mcIU/mL (normal 0.3–4.7) and a free T4 of 1.1 ng/dL (normal 0.8–1.6). Since that hospitalization, the patient was noted to have an elevated serum calcium ranging from 11.7 to 12.9 mg/dL (normal 8.7–10.5). A parathyroid hormone (PTH) assay performed in December 2005 was 449 pg/mL (normal 11–55) associated with a serum calcium of 12.9 mg/dL.
Subsequently, the patient underwent neck exploration for thyroidectomy and parathyroid exploration in 07 April 2006. Intraoperatively, the patient was found to have a firm, brown, 5.5 × 2.5 × 2 cm mass in the left lower pole of the thyroid gland. Sectioning of the mass at the time of frozen section showed a multiloculated, thick-walled cyst containing a large amount of chocolate-colored fluid.
Representative frozen and permanent histologic sections of the cyst wall demonstrated a thick, dense fibrous wall with adherent blood and fibrin (Fig. 2a). The adjacent parenchyma consisted of hypercellular parathyroid tissue and a small focus of compressed rim of normal parathyroid tissue (Fig. 2b). Within the hypercellular parathyroid tissue, there were multiple foci of recent (Fig. 2c) and old hemorrhage (Fig. 2d). Overall, the histopathological findings were consistent with a parathyroid adenoma that had undergone cystic degeneration. Additionally, there was a 1.1 cm nodule within the left mid thyroid gland that histologically exhibited nuclear features of papillary thyroid carcinoma (Fig. 3). These include pale, ovoid nuclei; fine, powdery chromatin; easily identifiable intranuclear grooves; and scattered intranuclear pseudo-inclusions.
a Low power photomicrograph [hematoxylin and eosin (H&E) stain; ×40, original magnification] of the cyst exhibits a thick, dense fibrous wall (W) containing blood (B). Just beyond the cyst wall, there is hypercellular parathyroid tissue (P) completely devoid of adipose tissue. b Medium power photomicrograph (H&E stain; ×100, original magnification) of the compressed rim of normal parathyroid tissue. Note the presence of adipocytes (arrows). c Medium power photomicrograph (H&E stain; ×100, original magnification) of cyst wall (W) with adjacent hypercellular parathyroid tissue (P) with recent hemorrhage. d Medium power photomicrograph (H&E stain; ×100, original magnification) of cyst wall (W) with adjacent hypercellular parathyroid tissue (P) containing hemosiderin-laden macrophages (arrows) indicative of old hemorrhage
Clinically, the patient’s PTH went from a pre-surgical level of 380 pg/mL to a post-resection level of 31 pg/mL, which was consistent with a successful resolution of his hyperparathyroidism. For the papillary thyroid carcinoma, the patient underwent a total thyroidectomy and received post-operative iodine-131 therapy. Currently, he is free of disease 1.5 years following surgery and is normocalcemic.
Discussion
Parathyroid cysts are rare clinical entities, and up to this date, just over 300 cases have been reported in the literature. The majority present as asymptomatic neck masses, but a smaller number of cases have also been described in the mediastinum. Occasionally, the cysts can grow to a large size and cause compressive symptoms, pain, and even recurrent laryngeal nerve palsy [8]. The sizes of parathyroid cysts have been reported to range from 1 to as large as 15 cm. Generally, parathyroid cysts are more commonly seen in women with a female-to-male ratio of 2.5:1 [1]. Although it can occur at any age between 16 and 79 years, most present between the fourth and sixth decades [10, 13].
Parathyroid cysts can be classified into non-functional and functional cysts. Non-functional cysts are much more common and are considered true cysts in that they are not derived from cystic degeneration. Functional cysts are rare, and it was not until 1936 that the first functioning mediastinal parathyroid cyst was surgically resected [9]. These cysts are thought to arise from adenomas that underwent central necrosis and degeneration [2]. The major clinical distinctions between non-functional and functional cysts are the patients with functional cysts often present with hyperparathyroidism, hypercalcemia and hypophosphatemia [2]. These patients can sometimes suffer weakness, weight loss, urinary incontinence, and memory disturbances due to high level of calcium [15]. These levels usually return to normal post-operatively. Functional cysts occur more commonly in the mediastinum, where they are almost as common as non-functional cysts.
Several theories have been proposed for the etiology of parathyroid cysts, but the four most accepted include [1, 5, 7, 8, 10, 12]: (1) embryologic remnants of the third and fourth pharyngeal pouches; (2) enlargement or coalescence of pre-existing microcysts; (3) enlargement of microcysts due to retention of cyst fluid; and (4) cystic degeneration of a parathyroid adenoma. The first theory is supported by the common location of parathyroid cyst in the inferior parathyroid gland. Furthermore, various combinations of tissues (lymphoid, muscular, thymic, salivary, adipose and mesenchymal) found in the cyst wall suggest an embryologic multipotential tissue of origin [7, 10]. The second theory is supported by the findings that microcysts are common in autopsy series and in normal parathyroid glands when carefully sectioned [6]. The third theory is supported by the fact that parathyroid cysts can be induced in laboratory animals when they are administered calcium acetate, vitamin D, parathyroid extract, and dihydrotachysterol [10]. The final theory is supported by histological studies of parathyroid cysts in patients with hyperparathyroidism.
Pre-operative CT and ultrasound can help to distinguish whether the mass is solid or cystic, but usually cannot differentiate thyroid from parathyroid cysts and the results are often experience dependence [14]. FNA is the most useful non-surgical means for the diagnosis of parathyroid cyst. Aspiration of clear fluid from the cyst should alert the physician of a high possibility of it being a parathyroid cyst [3]. Radioimmunoassays of the cyst contents for PTH and thyroglobulin are sensitive techniques to distinguish between thyroid and parathyroid cysts; however, they are rarely performed.
FNA has been suggested to be the initial treatment for easily accessible, small non-functional parathyroid cysts [4]. If repeated aspirations fail, surgery is the definitive treatment [7]. Sclerosing therapy can be used as an alternative to surgery, but it may be associated with many complications. All functional cysts and large, symptomatic non-functional cysts are best treated with surgery [7].
Our patient had an incidental finding of extrinsic compression on a barium swallow. His only complaint at that time was dysphagia. Although CT and ultrasound evaluation confirmed the presence of two cystic lesions in the left thyroid, they were unable to distinguish thyroid from parathyroid origin. However, the findings of elevated PTH and hypercalcemia were most consistent with the latter.
In conclusion, the pathological findings and post-operative PTH confirmed the presence of a functional parathyroid cyst. As noted, functional parathyroid cysts are much less common than non-functional cysts, and they tend to be localized in the mediastinum. Our patient had a functional parathyroid cyst that was located at the inferior border of the left thyroid.
References
Alvi A, Myssiorek D, Wasserman P (1996) Parathyroid cyst: current diagnostic and management principles. Head Neck 18(4):370–373
Fallon MD, Haines JW, Teitelbaum SL (1982) Cystic parathyroid gland hyperplasia—hyperparathyroidism presenting as a neck mass. Am J Clin Pathol 77(1):104–107
Fortson JK, Patel VG, Henderson VJ (2001) Parathyroid cysts: a case report and review of the literature. Laryngoscope 111(10):1726–1728
Ippolito G, Palazzo FF, Sebag F, Sierra M, De Micco C, Henry JF (2006) A single-institution 25-year review of true parathyroid cysts. Langenbecks Arch Surg 391(1):13–18
Jha BC, Nagarkar NM, Kochhart S, Mohan H, Dass A (1999) Parathyroid cyst: a rare cause of an anterior neck mass. J Laryngol Otol 113(1):73–75
McGinty LP, Lischer CE (1963) The surgical significance of parathyroid cysts. Surg Gynecol Obstet 117:703–708
McKay GD, Ng TH, Morgan GJ, Chen RC (2007) Giant functioning parathyroid cyst presenting as a retrosternal goitre. ANZ J Surg 77:297–304
Mils AK, Aanning LH (1990) Parathyroid cyst: case report of a rare surgical lesion of the neck. S D J Med 43(4):15–17
Noble J, Borg J (1936) Hyperparathyroidism complicated by hyperthyroidism. Report of a case. Arch Intern Med 58:846–859
Page GV, Burke ML, Metzger WT (1984) Parathyroid cysts. Am Surg 50(1):29–32
Sandstrom I (1880) Omen ny kortel hos menniskan och at skilliga daggdjus. Upsala Lakareforen Forh 14:441–471
Takashima S, Nakano H, Minamoto K, Misao T, Shiota K (2005) A thoracoscopically resected case of mediastinal parathyroid cyst. Acta Med Okayama 59(4):165–170
Thacker WC, Wells VH, Hall ER (1971) Parathyroid cysts of the mediastinum. Ann Surg 174(6):969–975
Ujiki MB, Nayar R, Sturgeon C et al (2007) Parathyroid cyst: often mistaken for a thyroid cyst. World J Surg 31:60–64
Wani S, Hao Z (2005) Atypical cystic adenoma of the parathyroid gland: case report and review of literature. Endocr Pract 11(6):389–393
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cao, H., Lai, C.K., Head, C.S. et al. Cystic parathyroid presenting as an apparent thyroid goiter. Eur Arch Otorhinolaryngol 265, 1285–1288 (2008). https://doi.org/10.1007/s00405-008-0608-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-008-0608-x