Abstract
We recorded cochlear potentials by transtympanic electrocochleography (ECochG) in three hearing-impaired children with GJB2 mutation who showed otoacoustic emissions. Pure tone thresholds, distortion product otoacoustic emissions (DPOAEs) and, auditory brainstem responses (ABRs) were also obtained. Subjects 1 (35delG/35delG) and 3 (M34T/wt) had profound hearing loss and showed the picture of auditory neuropathy (AN) as DPOAEs were detected with absent ABRs in both ears. The hearing impairment found in subject 2 (35delG/35delG) was profound in the right ear and moderate in the left ear. Both DPOAEs and ABRs with normal latencies and morphology were recorded only from the left ear. On the ECochG recording the cochlear microphonic was obtained from all children. No compound action potential (CAP) was detected in subject 1. A neural response was recorded only from the left ear in subject 2 with a threshold corresponding to the audiometric threshold while no CAP was detected on the right side. The ECochG obtained from subject 3 showed a low-amplitude broad negative deflection which was identifiable down to low stimulus levels. This response decreased in amplitude and duration when utilizing a high-rate stimulation paradigm. The amount of amplitude reduction was close to that calculated for normal ears, thus revealing the presence of an adapting neural component. These findings indicate that patients with GJB2 mutations and preserved outer hair cells function could present with the picture of AN. The hearing impairment is underlain by a selective inner hair cell loss or a lesion involving the synapses and/or the auditory nerve terminals. We suggest that neonatal hyperbilirubinemia may play a role in protecting outer hair cells against the damage induced by GJB2 mutations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mutations in the GJB2 gene account for 50% of cases of autosomal recessive nonsyndromic hearing loss [12]. The GJB2 gene encodes connexin 26, which is a protein involved in the formation of gap junctions connecting the supporting cells in the cochlea. These channels are believed to play a crucial role in K+ recycling from the extracellular space back to stria vascularis [4]. Therefore, channel dysfunction would result in increased K+ concentration leading in turn to hair cell intoxication and death [4].
More than 70 mutations of the GJB2 gene have been identified so far in subjects affected by nonsyndromic hearing loss [5, 13], although the frequency of the mutations shows wide variation in different populations [3, 5, 13]. Nevertheless, the 35delG represents the most common mutation with the condition of homozygosis accounting for about 60–70% of all GJB2 mutations in European populations [5, 13]. The degree of hearing impairment ranges from mild to profound, although the majority of subjects carrying the mutation in homozygosis show severe to profound hearing loss [5, 14].
Among GJB2 mutations the pathogenetic role of the M34T variant remains a controversial issue mainly because this genotype is frequently associated with normal hearing. Recently, on the basis of combined genetic, clinical and electrophysiological data it has been proposed that this mutation could lead to different degrees of constriction of the channel pore possibly resulting in wide variations of channel dysfunction and degree of hearing impairment [1].
Current knowledge indicates that the hearing loss due to GJB2 mutation is underlain by a lesion involving both inner (IHCs) and outer (OHCs) cochlear hair cells [4, 11]. However, Cheng and collaborators [3] have reported five hearing-impaired patients with GJB2 mutations who showed preserved OHCs function as indicated by the detection of otoacoustic emissions (OAEs). Since OAEs are believed to be undetectable in the presence of hearing thresholds exceeding 30 dB HL [2], these patients were assumed to have auditory neuropathy (AN). This is a disorder of the auditory nerve characterized by alterations of the auditory perceptions relying on temporal cues [20]. The lesion involves the auditory nerve fibres, inner hair cells and/or the synapses in between [19, 20]. The resulting alterations in temporal coding of acoustic signals lead to severe impairment of speech perception and absence of auditory brainstem responses (ABRs), while OHCs activities (cochlear microphonic, otoacoustic emissions) are preserved. However, the clinical picture of AN has been confirmed only in one patient of those reported by Cheng and colleagues.
Considering the database of hearing-impaired subjects with GJB2 mutations who are followed up at our institution, we found three children who showed OAEs in the presence of a hearing loss exceeding 30 dB HL. We analyzed the audiological and electrophysiological data collected from these patients. The aim was twofold. Firstly, we considered both ABR and OAE recordings in order to confirm or otherwise the diagnosis of AN. Secondly, we aimed to characterize the receptor and neural functions of the auditory periphery by means of transtympanic electrocochleography (ECochG), a near-field recording technique with a much better signal-to-noise ratio compared to ABRs. Indeed it allows us to record the compound action potential (CAP) generated by the auditory nerve, which is a much more robust response compared to ABR wave I. In addition, ECochG provides information on the receptor potentials, cochlear microphonic (CM) and summating potential (SP), which are primarily generated by OHCs [6] and IHCs [8], respectively.
Methods
Subjects
Subject 1 was a 12-month-old girl who had developed jaundice on the third day after birth with an increased bilirubin level which reached 20.2 mg/100 ml by the fourth day of life. She received phototherapy. Genetic analysis revealed the presence of the 35delG mutation in homozygosis.
Subject 2 was a 4-year-old boy whose clinical history was remarkable for high serum bilirubin level at birth (15.4 mg/100 ml on the second day of life) requiring phototherapy. He carried the 35delG mutation in homozygosis.
Subject 3 was a 12-month-old girl who had developed jaundice on the second day of life (11.2 mg/100 ml). Genetic analysis revealed the presence of the connexin 26 variant M34T.
Growth and motor development were normal in all subjects. Both CT and MRI scans (gadolinium infusion) of head and ear (including internal acoustic canal) were normal.
Distortion product otoacoustic emissions (DPOAEs)
In subject 1 DPOAEs were recorded by the Virtual 330 system. F1 and f2 level were kept at 65 and 55 dB SPL, respectively, while the f2/f1 ratio was 1.22. Primary tones were stepped in regular intervals from 1 to 4 kHz (1/12 octave steps from 1 to 4 kHz). DPOAEs were measured as an average of four separate spectral averages and eight time averages were performed. Each test lasted about 2 min. Two recordings were obtained, before and after the ECochG session.
In subjects 2 and 3 the DPOAEs were obtained by means of the ILO-92 OAE system (Otodynamics). The primary tones f1 and f2 were presented at 70 dB SPL and the f2/f1 ratio was kept at 1.21. The frequency was changed in 1/4 octave steps from 708 to 6,299 Hz. Four spectral averages were summed for each stimulus condition.
Audiometric testing
Air conduction thresholds at octave frequencies from 125 to 8,000 Hz were obtained in a sound attenuating-room (Grason-Stadler GSI 61 audiometer) in subjects 1 and 2. The degree of hearing impairment was defined by the pure tone average (PTA) threshold levels at 0.5, 1, 2 and 4 kHz. It was classified as mild (PTA 21–40 dB HL), moderate (PTA 41–70 dB HL), severe (PTA 71–95 dB HL) and profound (PTA > 95 dB HL).
In subject 3 behavioral thresholds were measured in a sound-attenuating room equipped for visual reinforced audiometry testing. Pure tones were presented in free-field from 250 to 4,000 Hz (Interacoustic AC30 Audiometer connected to a Pioneer A 103 amplifier, JBL TLX130 loudspeakers).
Tympanometry and middle ear muscle acoustic reflex thresholds (both ipsilateral and contralateral to the stimulated ear) were measured with an impedance Grason-Stadler GSI 33 audiometer. Acoustic reflexes were considered absent when no response was found at intensities higher than 110 dB HL.
ABR and ECochG recording
The ABR and ECochG recordings were performed under general anesthesia (sevoflurane) with the patient lying on a bed in an acoustically and electrically shielded room.
For ABR recordings stimuli were given monoaurally by a TDH-50 earphone and consisted of 0.1 ms clicks with alternating polarity and a maximum intensity of 90 dB nHL (referred to the psychoacoustical threshold of normal hearing subjects). Electroencephalographic activity was recorded ipsilaterally to the stimulated ear using silver-chloride cup electrodes, with the active and reference electrodes applied to the vertex and the mastoid, respectively.
Transtympanic ECochG was performed by means of a sterilized stainless steel electrode which was insulated except for the tip, placed on the promontory wall with the aid of an operating microscope. Two silver-chloride cup electrodes applied to the earlobe and forehead served as the reference and ground electrodes, respectively. Stimuli were trains of rarefaction and condensation 0.1 ms clicks, which were separately delivered in free-field by means of two high frequency drivers mounted on a single polyurethane horn (Electro-Voice DH1A/2MT 16 Ω, HP420) with a maximum intensity of 120 dB peSPL (corresponding to 90 dB nHL, referred to the psychoacoustical threshold of normally hearing subjects). The stimulus train consisted of a single click, which was followed 15 ms later by ten clicks with an inter-stimulus interval of 2.9 ms. The inter-train interval was kept at 197 ms. The stimulus was calibrated in free-field by means of a Brüel and Kjaer 4165 microphone (mounted on the 800 B Larson–Davis sound level meter), positioned 1 m from the base of the polyurethane horn, corresponding to the distance between the patient’s ear and the horn.
For both ABR and ECochG recordings, signals were differentially amplified (50,000), filtered (5–8,000 Hz) and sent to a computer for analog-to-digital conversion, displaying and averaging. The procedure of averaging the responses evoked separately by condensation and rarefaction clicks was applied to the ECochG recordings to extract the CAP. Then, the resulting curve was subtracted from the response evoked by condensation clicks to obtain the CM [15].
The CM amplitudes and thresholds were compared to the values obtained from 30 normally hearing ears (mean amplitude at 120 dB SPL 13.94±10.69 μV, range 1.56–37.6 μV; mean threshold 82.04 ± 10.47 dB SPL, range 60–110 dB SPL).
Results and discussion
Absent CAP and CAP with normal duration and morphology
Patients were followed up 2–3 years from the first evaluation, and this allowed us to obtain reliable audiometric thresholds.
Subject 1 showed the picture of AN since ABRs were absent while DPOAEs were detected in both ears (Fig. 1). Pure tone thresholds indicated profound hearing loss. Tympanometry was normal while acoustic middle ear muscle reflexes were absent.
The ECochG recordings (Fig. 2) revealed only the presence of CM while no CAP could be identified in either ear. CM amplitude was slightly below normal limits (right 1.69 μV, left 1.72 μV at 120 dB SPL) while CM threshold (right 100 dB SPL, left 110 dB SPL) was elevated compared to normal ears.
The absence of neural response in ECochG recordings at the maximum stimulation intensity is consistent with the audiometric picture indicating profound deafness. Indeed the 35delG mutation in homozygosis is associated with a degree of hearing impairment ranging from severe to profound in the majority of patients carrying GJB2 mutation [5, 13].
The presence of both DPOAEs and CM indicate that outer hair cell activity is preserved. In contrast, the absence of both SP and CAP point to a lesion involving inner hair cells. ECochG findings are consistent with currently available histopathological data. Temporal bone analysis carried out in one patient with GJB2 mutation showed degeneration of cochlear hair cells with preservation of auditory nerve fibers [11]. Moreover, histological studies performed in Cx26-deficient mice also showed hair cell degeneration and death [4].
The hearing loss affecting subject 2 (Fig. 3) was profound in the right ear and moderate in the left ear. Although uncommon, asymmetric hearing loss in patients carrying the 35delG mutation in homozygosis has been previously reported [13]. Neither OAEs nor brainstem responses could be obtained from the right ear whereas DPOAEs and ABRs with normal latencies and morphology were recorded from the left ear. Tympanometry was normal while middle ear muscle acoustic reflexes were found only in the left ear at 110 dB HL.
On the ECochG recording CM was detected with amplitudes (right 36.54 μV, left 4.80 μV at 120 dB SPL) and thresholds (80 dB SPL) within normal limits in both ears (Fig. 4). CAP could only be recorded from the left ear with 90 dB SPL threshold (normal CAP mean threshold 47.0±1.6 dB SPL) and this value was close to the PTA threshold levels at 1, 2 and 4 kHz. CAP duration (2.2 ms at 120 dB SPL) was also within normal limits (normal CAP mean duration at 120 dB SPL 2.5 ± 0.1 ms) while the SP was identifiable as a small negative deflection preceding the CAP.
The findings obtained from subject 2 in the right ear were similar to those collected from subject 1 except for the absence of DPOAEs. In contrast, the left ear showed a moderate hearing loss. Consistent with this finding the ECochG recordings displayed a CAP showing normal morphology and duration, while the threshold elevation corresponded to degree of hearing loss obtained by audiometric evaluation. Although the dissociation between hearing thresholds and OAE recordings in the left ear could suggest the presence of AN [3], the detection of a normal ABR ruled out this diagnosis. Thus, both the audiological and electrophysiological findings obtained from subject 2 indicate a cochlear hearing loss with spared function of OHCs or, at least, of a considerable number of them.
Long-lasting CAP
The audiological picture obtained from subject 3 (Fig. 5) was typical of AN since the detection of DPOAEs was associated with absent ABRs in both ears. Visual reinforced audiometry performed in free-field indicated profound hearing loss. Tympanometry was normal while middle ear muscle acoustic reflexes were absent.
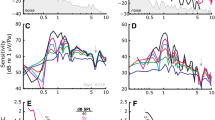
The ECochG recordings showed the CM superimposed on a broad negative potential (Fig. 6). Both CM amplitude (right 44.45 μV, left 11.46 μV at 120 dB SPL) and threshold (right 70 dB SPL, left 90 dB SPL) were within normal limits in both ears. The CAP could not be distinguished from the SP except for the response obtained from the right ear at 120 dB SPL. Moreover, compared to the recordings collected from normal ears, the ECochG response took on the appearance of a broad low-amplitude negative deflection, which recovered in no less than 10 ms at high stimulus levels (Fig. 7), this was identifiable down to low stimulus intensities (70 and 80 dB SPL in the right and left ear, respectively) in spite of the elevated audiometric thresholds (Fig. 6). In order to clarify whether this slow negative potential was just the SP slowly returning to baseline, or whether it also contained a neural component, a high-rate stimulation paradigm was performed in order to take advantage of neural adaptation (Fig. 8). When considering the stimulus sequence displayed in Fig. 8, in normally hearing subjects the response evoked by the last click (11th) of the stimulus train (adapted response) was reduced in amplitude compared with the response evoked by the initial (first) click (non-adapted response) of the sequence. The decrease mainly involved the CAP (68% attenuation at 110 dB SPL) while the SP showed only minor changes in amplitude (27% attenuation at 110 dB SPL) [9]. Looking at the recordings obtained from subject 3 the duration of the response evoked by the last click of the sequence appeared considerably shortened while its amplitude was decreased by 50% compared to the non-adapted state. These findings indicate that, at least at 110 dB SPL, the broad negative deflection superimposed on CM originates from neural rather from receptor elements. The remarkable increase in duration observed in the non-adapted state compared to normal could result from the altered timing in spike initiation leading to desynchronization of auditory nerve fiber discharge.
The genotype M34T/wt found in subject 3 is a pathological variant of connexin 26. This variant has been associated with constriction of channel pores leading to variable amounts of hearing impairment [1]. Taking into account these findings, it could be hypothesized that moderately increased K+ concentrations in the extracellular space due to pore dysfunction may enhance the glutamate release or slow its reuptake [4], which in turn underlies the prolonged depolarization of auditory nerve terminals. This could bring about a sort of conduction block along the auditory nerve preventing synchronized auditory information from reaching the brainstem [20]. This hypothesis could explain the findings of profound hearing loss and absent ABRs associated with detectable neural activation. Nevertheless, alternative explanations are also possible. Since there is no agreement about the pathogenetic role of the M34T variant [18], the phenotype observed in subject 3 may also be related to other unidentified mutations in GJB2 or in other genes.
Comparison with patients with congenital AN
Subjects 1 and 3 were included in our database of congenital AN (Table 1). Besides subjects with GJB2 mutations the database includes 17 children showing DPOAEs associated with absent ABRs. The degree of hearing impairment ranges from mild to profound while two subjects exhibit normal hearing thresholds. Twelve children had been discharged from NICU, three have familiar hearing impairment, while no risk factors for hearing loss could be identified in two subjects. It is noteworthy that neonatal hyperbilirubinemia with serum bilirubin levels ranging from 10 to 44 mg/100 ml has been reported in the clinical history of 12 subjects out of 17. Of these, eleven had been discharged from NICU.
Conclusion
We reported the audiological and electrocochleography findings obtained from three children with GJB2 mutations who showed DPOAEs associated with moderate to profound hearing loss. This represents an unexpected finding since OAEs are believed to be undetectable in the presence of hearing thresholds exceeding 30 dB HL (2). Recently, five patients with GJB2 mutations showing OAEs associated with severe to profound hearing loss have been reported by Cheng and colleagues [3]. These patients were assumed to have AN; however, the diagnosis was confirmed in only one of them who underwent ABR recording. The patients reported in this study showed OAEs in the presence of hearing threshold elevation higher than 30 dB HL. The picture of AN could be confirmed in only two of them whereas the presence of ABR with normal latencies and morphology ruled out the AN diagnosis in subject 2. Moreover, both the morphology and duration of the CAP recorded from this patient were similar to those obtained from normal ears. These findings indicate that the presence of OAEs in subjects with GJB2 mutations and threshold elevation higher than 30 dB HL do not necessarily underlie AN. Of the two subjects with the picture of AN, one showed absence of the CAP, thus indicating a lesion involving IHCs, while the ECochG findings obtained from the other allow us to localize the lesion in the distal portion of auditory nerve fibers.
The OHCs function was preserved the subjects reported in this study as indicated by both OAEs and CM recordings [19]. Conversely, the activity of IHCs and/or auditory nerve terminals was impaired in all patients. This represents a puzzling finding since it seems difficult to explain why high K+ concentrations are selectively toxic for the afferent compartment of the cochlea while leaving unchanged the OHC function. The latter was also preserved in children with congenital AN and no GJB2 mutation showing variable degrees of hearing impairment. Although in these children the peripheral lesion is possibly underlain by multiple etiological factors, the majority of them also showed elevated bilirubin levels during the first days of life. Particularly, this finding was almost invariably present in children who had been discharged from NICU. Recent studies [17] performed on the jaundiced Gunn rat animal model for kernicterus reported no abnormalities in cochlear hair cells in spite of the elevated serum bilirubin levels. Most importantly, a neuroprotective role for bilirubin has been demonstrated in hippocampal and cortical neuronal cultures [7], while mild to moderately elevated serum bilirubin levels have been associated with better outcome in diseases involving oxidative stress ([16] for review). It seems interesting that staining for the two isoforms of Heme Oxygenase (HO-1 and HO-2) has been observed in OHCs but not in IHCs [21]. It has also been proposed that the protective effects of heme oxygenase against oxidative stress in the cochlea may be related to its product, bilirubin [10]. This may indicate that OHCs but not IHCs tend to utilize bilirubin as an antioxidant. On the basis of the above reported findings, it is tempting to hypothesize that high serum bilirubin levels protect OHCs against the damage induced by several etiological agents including an increased K+ concentration due to connexin 26 dysfunction.
References
Bicego M, Beltramello M, Melchionda S, Carella M, Piazza V, Zelante V et al (2006) Pathogenetic role of the deafness-related M34T mutation of Cx26. Hum Mol Genet 15:2569–2587
Bonfils P, Piron JP, Uziel A, Pujol R (1988) A correlative study of evoked otoacoustic emission properties and audiometric threshold. Arch Otolaryngol 245:53–56
Cheng X, Brashears S, Morlet T, Ng SS, Berlin C, Hood L, Keats B (2005) Connexin 26 variants and auditory neuropathy/dys-synchrony among children in schools for the deaf. Am J Med Genet 9999:1–6
Cohen-Salmon M, Ott T, Michel V, Hardelin JP, Perfettini I, Eybalin M, Wu T, Marcus DC, Wangemann P, Willecke K, Petit C (2002) Targeted ablation of connexin 26 in the inner ear epithelial gap junction network causes hearing impairment and cell death. Curr Biol 12:1106–1111
Cryns K, Orzan E, Murgia A, Huygen PL et al (2004) A genotype-phenotype correlation for GJB2 (connexin 26) deafness. J Med Genet 41:147–154
Dallos P, Wang CY (1974) Bioelectric correlates of kanamycin intoxication. Audiology 13:277–289
Doré S, Takahashi M, Ferris CD, Hester LD, Guastella D, Snyder SH (1999) Bilirubin, formed by activation of heme oxygenase-2 protects neurons against oxidative stress injury. Proc Natl Acad Sci 96:2445–2450
Durrant JD, Wang J, Ding DL, Salvi RJ (1998) Are inner or outer hair cells the source of summating potentials recorded from the round window? J Acoust Soc Am 104:370–377
Eggermont JJ, Odenthal DW (1974) Action potentials and summating potentials in the normal human cochlea. Acta Otolaryngol Suppl 316:39–61
Fairfield DA, Kanicki AC, Lomax MI, Altschuler RA (2004) Induction of heat shock protein (Hsp32) in the rat cochlea following hyperthermia. Hear Res 188:1–11
Jun AI, McGuirt WT, Hinojosa R, Green GE, Fischel-Ghodsian N, Smith RJ (2000) Temporal bone histopathology in connexin 26-related hearing loss. Laryngoscope 110:269–275
Kenneson A, Van Naarden Braun K, Boyle C (2002) GJB2 (connexin 26) variants and nonsyndromic sensorineural hearing loss: a HuGE review. Genet Med 4:258–274
Liu XZ, Pandya A, Angeli S, Telischi FF, Arnos KS, Nance WE, Balkany T (2005) Audiological features of GJB2 (connexin 26) deafness. Ear Hear 26:361–369
Salvinelli F, Casale M, D’Ascanio L, Firrisi L, Greco F, Baldi A (2004) Hearing loss associated with 35delG mutation in Connexin-26 (GJB2) gene: audiogram analysis. J Laryngol Otol 118:8–11
Santarelli R, Scimemi P, Dal Monte E, Arslan E (2006) Cochlear microphonic potential recorded by transtympanic electrocochleography in normally hearing and hearing-impaired ears. Acta Otorhinolaryngol Ital 26:78–95
Sedlak TW, Snyder SH (2004) Bilirubin benefits: cellular protection by a biliverdin reductase antioxidant cycle. Pediatrics 113:1776–1782
Shaia WT, Shapiro SM, Spencer RF (2005) The jaundiced Gunn rat model of auditory neuropathy/dyssynchrony. Laryngoscope 115:2167–2173
Snoeckx RL, Huygen PL, Feldmann D, Marlin S et al (2005) GJB2 mutations and degree of hearing loss: a multicenter study. Am J Hum Genet 77:945–957
Starr A, Picton TW, Sininger Y, Hood LJ, Berlin CI (1996) Auditory neuropathy. Brain 119:741–753
Starr A, Isaacson B, Michalewski HJ, Zeng FG, Kong YY, Beale P, Paulson GW, Keats BJ, Lesperance MM (2004) A dominantly inherited progressive deafness affecting distal auditory nerve and hair cells. J Assoc Res Otolaryngol 5:411–426
Watanabe K, Oshima T, Kobayashi T, Ikeda K (2003) The expression and localization of heme oxygenase in the adult guinea pig cochlea. Brain Res 966:162–166
Acknowledgments
This research was supported by MURST project n. 2004061714_004. We are grateful to Patrizia Lunardelli for her invaluable technical support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Santarelli, R., Cama, E., Scimemi, P. et al. Audiological and electrocochleography findings in hearing-impaired children with connexin 26 mutations and otoacoustic emissions. Eur Arch Otorhinolaryngol 265, 43–51 (2008). https://doi.org/10.1007/s00405-007-0412-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-007-0412-z