Abstract
Problems in functioning are frequently seen in survivors of head and neck cancer (HNC) and proof to have increasing impact on their quality of life. With the approval of the International Classification of Functioning, Disability and Health (ICF) by the World Health Assembly in May 2001, we can now rely on a globally accepted framework and classification system based on a bio-psycho-social mode to assess and compare functional outcome. To make the ICF-classification with more than 1.400 categories applicable to every-day clinical practice, ICF core sets are established. The objective of this paper is to outline the proposed development process for the ICF core set for HNC and to invite international experts to participate in this process. The ICF core set will be defined at a Consensus conference, which will integrate evidence from preparatory studies, namely: (a) a systematic literature review regarding the outcome measures of clinical trails and observational studies, (b) semi-structured patient interviews, (c) international experts participating in a internet-based survey and (d) cross-sectional, multi-center studies for clinical applicability. To validate the ICF core set field-testing will follow. The ICF provides useful standards of clinical rehabilitation practice, research and teaching. Its application stimulates comparability of outcome parameters, eventually improving understanding of functioning and disability. The ICF can function as a new language, simplifying communication and cooperation between various professional backgrounds and between health professionals and their patients eventually leading to a more effective and economic rehabilitation. The ICF core set for HNC is designed to translate the benefits of the ICF into clinical routine. The development of ICF core sets is an inclusive and open process. Anyone who wishes to actively participate is invited to contact the project coordinator (Uta.Tschiesner@med.uni-muenchen.de). Individuals, institutions and associations can be formally associated as partners of the project.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The diagnosis of head and neck cancer (HNC) means that the patient has to face not only a life-threatening disease but also sometimes drastic functional problems in breathing, eating, speech production and pain [1, 2]. Also disfigurement can lead to changes in self-image, worsened relationship with the partner and increased social isolation [3].
Historically the intent of cancer treatment has been curative focusing on outcome measures such as tumor response, disease-free survival or overall survival [4]. Over the last years, there has been increasing interest and awareness in the behavioral and functional impact of oncologic treatment on the patient and health-related quality of life has now become a secondary endpoint in the assessment of outcome [5–8].
The heterogenity of head and neck cancer patients, in terms of tumor site, the diversity of surgical approaches and radiochemotherapeutic regimens and the patient specific differences in response to these variables make it particularly difficult to describe precise outcome [9].
Both groups of patients, those with tumor recurrence and those who are free of disease after treatment, show a great need for rehabilitation. Although the underlying tumor may not be completely cured, rehabilitation can reduce symptoms, disability and possibly health care costs-making rehabilitation successful for both the individual and society [10]. Rehabilitation is a continuous process and involves the identification of patient’s needs and problems and the relation of such needs to the given body structures and functions and factors in the patient’s environment [11]. It demands close cooperation and communication between various health professionals, e.g., oncologists, radiotherapists, ENT-surgeons, maxillofacial-surgeons, psychologists, speech and swallowing rehabilitation therapists, physical therapists and social workers.
Determining how to measure and quantify a subjective experience like functioning in every-day life-situations or quality of life has been a challenging task. Methodological advances now include increased use of validated measures, advances in study design and attention to patient’s attitudes [12]. Until now there are only very few standardized cancer specific methods that are reliable and valid and still concise enough to be practically relevant in clinical trials. Even fewer instruments have been developed for cross-cultural application [13–15]. To our knowledge, still, there are many parts of the Asian, African and American cultures are not included in any cross-cultural tool to evaluate functional outcome in head and neck cancer.
In addition, many of the available tools concentrate on selected aspects of the entire problem. For clinical practice and further research it would be valuable to have a practical framework that covers the entire spectrum of disabilities and guides all aspects of rehabilitation.
To achieve this goal, we need a comprehensive framework on how to address disabilities and a matching classification to group them effectively, which serves as a universal language understood by health professionals, researchers, patients, patient organizations and insurance companies at the same time.
The ICF framework and classification
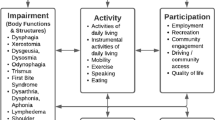
With the approval of the International Classification of Functioning, Disabilities and Health (ICF) by the World Health assembly in 2001, we can now rely on a globally agreed-upon framework and classification that fulfills these requirements [16]. The ICF belongs to the World Health Organization’s family of international health classifications. While the International Classification of Disease (ICD) classifies diagnoses and originates in 1893 (as the “International List of Causes of Death”) [17], the ICF classifies functioning and was adopted just lately, in 2001 (Fig. 1).
In the ICF perspective a patient’s functioning, disability and health is closely related to the underlying health condition but is not a mere consequence of it [18]. The ICF framework has adopted a multifactor understanding of function and disability, merging several factors into a bio-psycho-social perspective. The patient’s functioning is conceived as a dynamic interaction between the underlying health condition and specific personal and environmental contextual factors. It is used in clinical rehabilitation to structure a patient’s limitations [19]. Mandatory for successful management of impairments is to understand the relationship between selected target problems within the direct assessment of a patient’s functioning and disability and their contextual factors, which might either exacerbate or reduce the impairment.
The ICF classification is a hierarchical code system where various so-called ICF categories represent the basic units of the classification. Altogether there are more than 1.400 ICF-categories.
Each ICF component is represented by a letter (s, b, d, e) and followed by a four digit numeric code defining the chapter and further detailing. With a generic qualifier scale the magnitude of impairment can be evaluated. In general the mapping of a patient’s limitations to detailed ICF categories is done by the clinician guiding rehabilitation and should be transparent to the patient at any stage. Among several factors, the success of the classification depends on its usefulness and feasibility in clinical practice.
Reasoning for developing ICF core sets
However, a comprehensive, highly detailed classification, structured in a rather new and thereby unfamiliar approach to many health professionals, is not easily qualified for adoption to every-day clinical use. To overcome this obvious difficulty, so called ICF core sets are developed for medical conditions that have high impact on a patient’s functioning and disability [20]. These specific ICF core sets contain a limited number of pre-selected ICF-categories (e.g., 70 out of 1.400 categories) linked to a certain health condition. Such a health condition, e.g., laryngeal carcinoma, represents the mindset in which medical professionals are trained to think. The ICF core set contains categories not only on anatomic and pathophysiologic changes but also on functioning in every-day activities and relevant environmental factors. By tying an ICF core set to a health condition, the ICF core set becomes a familiar introduction to the bio-psycho-social view inherited in the ICF and assists the clinician to spend a minimum of time in a focused, patient-oriented way.
These ICF core sets are to be developed in two levels: A brief and a comprehensive ICF core set. The brief ICF core set includes only the most important ICF-categories and is intended to be rated in all patients of a clinical study. The comprehensive ICF core set, however, includes all categories that are typically limited in the selected health condition, and is created to guide multidisciplinary assessment [21].
Realizing that the significance and power of the ICF lies in its conceptualization of functioning and disability, there is a call for creating ICF-based instruments that are more appropriate to clinical information needs [21, 22].
Even though deriving ICF core sets in a scientifically profound way (as outlined in this paper) proves to be a work-intensive process, presently it is the best way available to combine the ICF-framework’s and classification’s advantages for patient care, inter-medical communication and scientific research with the necessary practicability and feasibility for clinical use (for advantages, see Table 1).
Experience with developing ICF core sets
The ICF core set project is a joint project of the ICF research branch of the WHO Collaboration Center of the Family of International Classifications (DIMDI) at Ludwig-Maximilians University in Munich, Germany together with the classification, assessment and surveys (CAS) team at the WHO and an increasing number of partner organizations [23].
So far ICF core sets have been developed for 12 health conditions including chronic ischemic heart disease [24], obstructive pulmonary disease [25], stroke [26], diabetes mellitus and rheumatoid arthritis [27]. So far, breast cancer [28] is the only malignant condition that has an ICF core set (for available ICF core sets, see Table 2).
We currently work on the development of an ICF core set for HNC. It is expected to be the first head and neck condition to be linked to the ICF-framework and the ICF-classification.
The ICF core set development project for HNC is a cooperation between the Department of Otorhinolaryngology at Ludwig-Maximilians University (Munich, Germany) and the ICF Research Branch of the World Health Organization (WHO) Collaboration Centre of the Family of International Classifications (DIMDI, Munich, Germany), the Classification, Assessment and Terminology-team and partner institutions across the world.
This ICF core set development project is funded by Deutsche Krebshilfe e.V..
Objective
The objective of this paper is to outline the proposed development process for the ICF core sets for HNC and to invite clinical experts from all over the world to actively participate in this process.
Methods for the development of the ICF core set for HNC
Defining the range of the ICF core set for HNC
The ICF core set for HNC should include a single or a group of diagnoses with similar effects on functioning, disability and health. It was decided to summarize a collection of carcinoma locations in the upper aero-digestive tract to create a combined ICF core set. As a working hypothesis, this includes carcinomas located in the oral cavity, oro- and hypopharynx, larynx and the salivary glands. The comparably small group of carcinomas of the nose and paranasal sinuses—3% of all carcinomas of the upper aero-digestive tract [29]—are not included due to significant differences in etiology, clinical presentation and resulting problems in functioning. To include nasopharyngheal carcinoma would have been even more difficult, since it occurs to 20–35% in children [30], who are excluded in the evaluation of the other cancer locations (inclusion criteria: patients >18 years).
Within this group of selected cancer locations it was decided to make the ICF core set applicable to all tumor stages, to any cancer treatment with proven efficacy—namely surgery, radiation, chemotherapy [31–33]—and also to integrate all patients who have completed initial cancer treatment independent of prognosis and time of survival so far.
To check for these working hypotheses, all data on the different subgroups (in terms of tumor location, stage, treatment and survival time) will be collected in the development phase and evaluated for significant differences that might forbid to develop a combined ICF core set for HNC.
Methods to be used in the ICF core set development
Preparatory phase
Within this phase of the project all relevant perspectives should be addressed: (a) researchers, (b) patients, (c) clinical experts. In the fourth preparatory study (d) the applicability of the ICF in typical clinical situations will be tested.
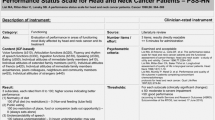
(a) Systematic literature review: This procedure captures the view of researchers by identifying and quantifying the concepts behind well-known and accepted outcome measures cited in English literature between 2000 and 2006.
In a first step studies are selected through pre-defined inclusion and exclusion criteria in a MEDLINE-based research. All found papers are then checked by two independent, ICF-trained investigators for inclusion. Both reviewers will extract data on outcome measures using a standardized electronic data record. If there is disagreement between these two reviewers a third person has to be consulted. In a second step the outcome measures and the underlying concepts will be specified and, finally, linked to ICF categories using standardized linking rules [34]. Each relevant measure will be linked separately by two health professionals trained in the ICF. Absolute and relative frequencies of outcome measures and the linked ICF-categories will be reported.
(b) Patient interviews: Semi-structured interviews with patients who suffer from head and neck cancer are held to identify those aspects that are important to the patient [35, 36]. The gathered aspects of functioning and disability are then translated into ICF-categories. All interviews are digitally recorded, transcribed verbatim and evaluated again by two independent health professionals. All patient interviewees also fill in questionnaires on their general oncologic and disease-specific status (EORTC-C30, EORTC-HN35) [13, 37], on existing comorbidities and to collect personal clinical data on the specific disease stage and treatment of the patient.
The numbers of interviews are determined by saturation, which is defined as the point during data collection where two consecutive interviews reveal no additional information. Descriptive statistics examine the frequency of ICF-categories in patient interviews.
(c) Expert survey: In an Internet based expert survey we will collect clinical experts’ opinions on the most relevant and typical problems of patients with HNC. The aim is to include experts from all six WHO regions and from different health professions, including oncologists, radiotherapists, ENT surgeons, maxillofacial surgeons, dentists, clinical psychologists, speech and language therapists, physical therapists, nurses, dieticians, and social workers. At the end of the survey, there will be a list of relevant ICF-categories together with the relative frequencies.
(d) Cross-sectional study: The cross-sectional multi-center study aims to identify the most common problems encountered when applying the ICF-classification system into clinical practice. The study design is a multi-center cross-sectional study.
An extended ICF checklist tract will be used. The checklist provides a relatively simple questionnaire with guidelines and probes, which can be filled out by the physician or other health professional, and makes it possible to classify the most important ICF categories in clinical practice [38]. With respect to all categories on the second level of the ICF, the ICF checklist includes 29 (25%) categories from the component ‘body functions’, 16 (29%) from ‘body structures’, 48 (41%) from ‘activities and participation’, and 32 (43%) from ‘environmental factors’. Using the extended ICF checklist, all available medical and diagnostic information about the patient is taken into account. At the end of each of the four ICF components, the health professional responsible for the data collection at the study center can add any relevant ICF category necessary to perform a comprehensive description of functioning and disability of the patient.
Data analysis for the four preparatory studies
For the ICF-components body function, body structures, activity and participation absolute and relative frequencies will be reported at 95% confidence intervals. For the contextual component environmental factors, absolute and relative frequencies will be reported for those, where the specific factor was regarded either a barrier or a facilitator of rehabilitation.
Logistics as well as linear regression analysis will identify categories that explain most of the variance of external standards used in the study.
Consensus conference
The main task of the Consensus conference is to develop an internationally accepted ICF core set for HNC that is still practical and feasible to apply. The results of the preparatory phase are a starting point for the participating experts who work actively together for 3 days in a teamwork technique called the “Nominal Group Technique” [39]. The ICF core set Consensus conference will involve health professionals from different parts of the world. The maximum number of experts attending the conference was set at 21 (3 groups of 7 persons each), which is considered necessary to address the broad interests to involve the different professions and regions of the world. It was also decided, that each group should consist of different health professionals who will work together in the spirit of partnership and the multi-professional and interdisciplinary approach, which is typical for care and research for patients with HNC. However, when inviting experts to the conference, they have to be fluent in English in order to contribute to the process.
The recruitment strategy for the experts has to balance the needs for international expertise without compromising a feasible decision-making process. Therefore (1) formal cooperation with appropriate organizations will be established, (2) clinicians involved in the preparatory studies will be invited, (3) international and regional societies (or working groups) will be identified and their members contacted, (4) opinion leaders in the different health conditions will be identified and invited, and (5) experts in the fields of functioning and health, quality of life, health statistics, and public health from developing countries will be contacted by the WHO and invited to the conference. This strategy ensures broad international representation and clinical expertise among the participants.
Consensus procedure: The participants will be trained on both ICF in general and the data from the preparatory studies. The ICF core set categories will be identified in an iterative decision-making process. Two different kinds of sessions will be differentiated during the consensus process: a working group session, where the experts work separately in groups and discuss pros and cons for the selection of an ICF category and a condition group session, where all experts work together and give feedback for the selection of one category.
After a two-round ranking exercise followed by a final vote the experts will decide on second level categories for the comprehensive ICF core set, and—out of the comprehensive set—will vote on the about 15 second level categories for the brief ICF core set.
Testing the ICF core sets (validation phase)
After the ICF core sets are decided on, the testing and implementation of ICF core sets for HNC will be established. The general objective of this phase is to study the validity and feasibility of the brief and comprehensive ICF core set. In addition it will be tested to what extend there are typical profiles for the different cancer locations, namely oral carcinoma, salivary glands, oro- and hypopharynx, and larynx.
This is planned to be done in a multicenter cohort study at a network of cooperating organizations. The specific aim will be to examine the frequencies of patients problems in subsets including age, gender, nationality, socio-economic factors, co-morbidities, etc., to identify the categories with most variance of external standards and to analyze to what extend of the whole spectrum of disabilities is represented in the core set. Rasch analyses will help to understand what extent of the whole spectrum of problems in functioning and disability is represented in the ICF core set for malignant tumors of the upper aerodigestive tract.
The project will be conducted in conformity with the ethical principles of the Declaration of Helsinki. All appropriate study-related documents will be presented to the Ethics committees for review and approval.
Figure 2 summarizes the time schedule for the ICF core set development for HNC.
Discussion
ICF core sets are practical tools for different purposes. They allow clinicians and researchers to classify and describe individual’s functioning using the most relevant ICF codes. In a clinical set-up the ICF core set for HNC may not be seen in competition to established tools to collect information (e.g., validated patient questionnaires, video swallow, speech intelligibility testing), but rather as a comprehensive framework to structure the obtained information in the bio-psycho-social view of the ICF and guide rehabilitation accordingly.
A Brief ICF core set may facilitate international studies and studies comparing the consequences of different conditions. A Comprehensive ICF core set can be used in the clinic as a checklist to assess patient’s needs, to formulate rehabilitation goals and to evaluate progress. A general reference framework may be powerful both with regard to communication between health professionals within specific settings and when communicating between health professionals and patients.
As in any scientific effort, there are uncertainties that have to be resolved during the process. As mentioned, the preparatory studies will provide the necessary information to guide decisions on the working hypotheses regarding inclusion criteria on (a) cancer location, (b) treatment type, and (c) prognosis. It is important to realize that the ICF core set Consensus conference will provide only a first, best possible version of ICF core sets for HNC, which needs to be tested in the validation phase.
Physicians and patient perceptions of clinical outcome in oncology often have low correlation [40, 41]. In order to capture both sides of reality for an ICF core set for patients with HNC, we will collect data from patient interviews (part 2 and 4 of the preparatory studies) and from scientists and clinical experts who treat the patients (part 1and 3 of the preparatory studies).
The assessment of functioning and quality of life data is highly sensitive to ethno-cultural and language differences [42, 43]. In head and neck cancer patients in particular areas like “ pain” or “constipation” are associated with cultural background [44]. In order to come up with a first version of an ICF core set for HNC that integrates information from different cultural backgrounds, the preparatory studies will gather data on patients being treated at centers from different countries (part 4 of the preparatory studies) and from professionals in an international expert survey (part 3 of the preparatory studies). The consensus conference will be internationally designed.
However, both preparatory studies collect information only from English speaking participants. This is done to ease comparability of results from different countries, but on the other hand might contain a structural bias for countries where English in not the native language. The issue of the extent and relevance of such a bias will be addressed in the validation phase following the Consensus conference.
The main reason for the creation and implementation of ICF are obviously advantages to patient care. However, besides these there are still some other advantages to other fields of medical treatment:
The ICF core sets help to comprehensively address and structure patients’ problems. This may be particularly useful during medical training but may also be of value in the hands of experienced clinicians since physicians may underestimate patients’ functional problems [45] and in a multi-professional teamwork approach which in many times is required when dealing with head and neck cancer where fighting the tumor and managing the sequela after therapy go together. Integrating the target problems of a patient in e.g., the referral to a medical institution or a letter of discharge can improve precision of the mandate of medical therapy between institutions and increase transparency of treatment for the patient. Moreover, internal reporting on the success of a certain procedure can be evaluated efficiently.
Several health organizations are now collaborating on several ICF core set development programs worldwide [23]. The ICF core sets allow clinicians and researchers to classify and describe an individual’s functioning using widely accepted terminology. Shared terminology and common definitions permit international studies and ease the comparison among them.
An ICF core set can also be used to rate the content validity of health-status measures and, thereby, select appropriate instruments for the specific needs of persons with HNC. In the future, ICF and the ICF core sets may become the new base for the further development of such measures.
In a decade where health care providers increasingly question the necessity of a certain procedure that is not applied in all patients with this diagnosis, the use of ICF categories can assist health care professionals in explaining the necessity of a certain procedure for a patient. ICF facilitates linking medical data across different conditions or interventions for efficient, transparent and cost-effective health care.
However, making the ICF practical and easy-to-use in clinical routine is the most crucial aspect when implementing the ICF framework and classification to rehabilitation of patients with HNC. The two main obstacles are (a) the rather new and thereby unfamiliar way of thinking integrated in ICF and (b) the vast amount of categories included in the entire classification. To overcome both obstacles brief and comprehensive ICF core sets are to be developed. With the help of these core sets we hope to gain the clinical feasibility to translate the high value proposition encountered in the ICF classification towards rehabilitation of patients HNC.
In conclusion, this is just a small step forward in the development of a world-wide accepted and standardized tool for the assessment of functional impairment of HNC. Establishing standard, disease-specific ICF core sets in the long run should be useful for clinical practice, teaching, medical research and cooperation between the various players in a modern health care system.
Invitation for participation
The development of ICF core sets is an inclusive and open process. Therefore, the authors of this paper encourage clinical experts and patients to actively participate in the process. Anyone who wishes to actively participate in this process is invited to contact the international project coordinator (uta.tschiesner@med.uni-muenchen.de). Individuals, institutions and associations can be formally associated as partners of the project.
References
Morton RP, Izzard ME (2003) Quality-of-life outcomes in head and neck cancer patients. World J Surg 2:884–889
Rogers SN, Miller RD, AliK, Minhas AB, Williams HF, Lowe D (2006) Patients persieved health statusfollowing primary surgery for oral and oropharyngeal cancer. Int J Oral Maxillofacial Surg 35:913–919
Lee-Preston V, Steen IN, Kelly GC, Welch AR, Meikle D, Stafford FW, Wilson JA (2004) Optimizing the assessment of quality of life after laryngeal cancer treatment. J Laryngol Otol 118:432–438
Aaronson NK (1988) Quality of life: what is it? How should it be measured?. Oncology 2:69–74
Rogers SN, Humphris G, Lowe D et al (1998) The impact of surgery for oral cancer on quality of life as measured by the Medical outcomes short form 36. Oral Oncol 34:171
DAntonio LL, Zimmermann GJ, Cella DF, Long SA (1996) Quality of life and functional status measures in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg 122:482–487
Aaronson NK, Beckmann J (eds) (1986) The quality of life in cancer patients. EORTC study group on quality of life. J Psychosoc Oncol 4:43–53
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E et al (1993) The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol 11(3):570–579
List MA, Bilir SP (2004) Functional outcomes in head and neck cancer. Semin Radiat Oncol 14(2):178–189
Stucki G, Sangha O (1997) Principles of rehabilitation. In: Klippel IJH, Dieppe IPA (eds) Rheumatology. Mosby, London, pp 11.1–11.14
Stucki G, Ewert T, Cieza AS (2004) Value and application of ICF in rehabilitation. Disabil Rehabil 24(17):932–938
List MA, Stracks J (2000) Evaluation of quality of life in patients definitively treated for squamous carcinoma of the head and neck. Curr Opin Oncol 12:215–220
Aaronson NK, Ahmedzai S, Bergman B et al (1993) The European organization for research and treatment of cancer QLQ-C30: a quality of life instrument for use in international clinical trilas in oncolgy. J Nat Cancer Inst 85:365–376
Bjordal K, de Graeff A, Fayers PM, Hammerlid E et al (2000) A 12 country field study of EORTC QLQ-C30 and the head and neck cancer specific module (EORTC QLO-H&N35) in head and neck cancer patients. Euro J Cancer 36:1796–1807
Chandu A, Smith AC, Rogers SN (2006) Health-related quality of life in oral cancer: a review. J Oral Maxillofac Surg 64(3):495–502
World Health Organization (2001) International Classification of Functioning, Disability and Health ICF
www.who.int/classifications/icd/en/index
Stucki G, Grimby G (2004) Foreword: applying the ICF in medicine. J Rehabil Med 44(3 Suppl):5–6
Cieza A, Stucki G (2004) New approaches to understand the impact on musculoscelletal conditions. Best practise and research Clin Rheumatol 18(2):141–154
Stucki G, Cieza A, Ewert T, Kostanjsek N, Chatterji S, Üstün T B (2002) Application of the international classification of functioning, disability and health (ICF) in clinical practice. Disabil Rehabil 24:281–282
Stucki G, Ewert T, Cieza A (2002) Value and application of the ICF in rehabilitation medicine. Disabil Rehabil 24(17):932–938
Stucki G, Cieza A, Ewert T, Kostanjsek N, Chatterji S, Üstün TB (2002) Application of the international classification of functioning, disability and health (ICF) in clinical practice. Disabil Rehabil 24:281–282
A list of collaborating partners and organizations: http://www.icf-research-branch.org/aboutus/partners.htm
Cieza A, Stucki A, Geyh S, Berteanu M et al (2004) ICF core sets for chronic ischemic heart disease. J Rehabil Med 44(Suppl):94–99
Stucki A, Stoll T, Cieza A, Weigl M et al (2004) ICF core sets for obstructive pulmonary disease. J Rehabil Med 44(Suppl):114–120
Geyh S, Cieza A, Schouten J, Dickson H, Frommelt P, Omar Z, Kostanjsek N, Ring H, Stucki G (2004) ICF core set for stroke. Rehabil Med 44(Suppl):135–141
Cieza A, Ewert T, Üstün B, Chatterji S, Konstansjek N, Stucki G (2004) Development of ICF core sets for patients with chronic conditions. J Rehabil Med 44(3 Suppl):9–11
Brach M, Cieza A, Stucki G, Füßl M, Cole A, Ellerin B, Fialka-Moser V (2004) ICF core sets for breast cancer. J Rehabil Med 44(Suppl):121–127
Wright, ST, Pou A (2004) Neoplasms of the nose and paranasal sinuses; grand rounds presentation, UTMB, Dept. of Otolaryngol, http://www.utmb.edu/otoref/Grnds/Nose-sinus-CA-040519/Nose-sinus-CA-040519.htm
Paulino AC, Grupp SA (2006) Nasopharyngeal cancer; http://www.emedicine.com/ped/topic1553.htm
De Nittis AS, Machtay M, Rosenthal DI et al (2001) Advanced oropharyngeal carcinoma treated with surgery and radiotherapy, oncologic outcome and functional assessment. Am J Otolaryngol 22(5):329–335
Friedlander P, Caruana S, Bhuvanesh S et al (2002) Functional status after primary surgical therapy for squamous cell carcinoma. Head Neck 24(2):111–114
Robertson ML, Gleich LL, Barrett WL, Glukmann JK (2001) Survival, function and quality of life after external beam irradiation and brachytherapy, base-of-tongue cancer. Laryngoscope 111(8):1362–1365
Cieza A, Brockow T, Ewert T et al (2002) Linking health-status measurements to the international classification of functioning, disability and health. J Rehabil Med 34:205–210
Kirwan J, Heiberg T, Hewlett S et al (2003) Outcomes from the patient perspective workshop at OMERACT 6. J Rheumatol 30(4):868–876
Kvale S (1996) Interviews—an introduction to qualitative research interviewing. Sage Publications, Beverly Hills
Bjordal K, de Graeff A, Fayers PM, Hammerlid E et al (2000) A 12 country filed study of the EORTC QLQ-C30 and the head and neck spacific module (EORTC QLQ-HN35) in head and neck patients. Euro J Cancer 36:1796–1807
World Health Organization (2003) ICF Checklist. Geneva
Delbeq AI, Van de Ven AH, Gustafson DH (1975) Group techniques for program planning: a guide to nominal group and delphi processes. Glencoe, Scott
Otto RA, Dobie RA, Lawrence V (1997) Impact of laryngectomy on quality of life: perspective of the patient versus that of the health care provider. Ann Otol Rhinol Laryngol 106(8):693–699
Mohide EA, Archibald SD, Tew M, Young JE, Haines T (1992) Postlaryngectomy quality-of-life dimensions identified by patients and health care professionals. Am J Surg 164(6):619–622
Pasick RJ, Stewart SL, Bird JA, D Onofrio CN (2001) Quality of data in multiethical health surveys. Public Health Rep 116(Suppl 1):223–243
Hahn EA, HolznerB, Kemmler G, Sperner-Unterweger B, Hudgens SA, Cella D (2005) Crosscultural evaluation of health stus using item response theory: FACT_B comparison between Austrian and U.S: patients with breast cancer Eval Health Prof 28(2):233–259
Allison (2001) Health-related quality of life comparisons in French and English-speaking populations. Community Dent Health 18(4):214–218
Steiner WA, Ryser L, Huber E, Uebelhart D, Aeschlimann A, Stucki G (2002) Use of the ICF model as a clinical problem-solving tool in physical therapy and rehabilitation medicine. Phys Ther Nov 82(11):1098–1107
Author information
Authors and Affiliations
Corresponding author
Additional information
The project is funded by Deutsche Krebshilfe e.V. The project is developed in cooperation with the World Health Organization (WHO).
Rights and permissions
About this article
Cite this article
Tschiesner, U., Cieza, A., Rogers, S.N. et al. Developing core sets for patients with head and neck cancer based on the International Classification of Functioning, Disability and Health (ICF). Eur Arch Otorhinolaryngol 264, 1215–1222 (2007). https://doi.org/10.1007/s00405-007-0335-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-007-0335-8