Abstract
Sonotubometry allows an assessment of the Eustachian tube (ET) function under physiological conditions. The reliability of the application of an 8 kHz pure-tone signal was investigated. In 40 normal subjects (80 ears) sonotubometric studies were performed with a custom-made device. ET opening was provoked by swallowing, yawning and Valsalva manoeuvre. An opening was detected in all patients but not in all manoeuvres. Four characteristic sonotubogram types were found. Most common was the spike-type (60%). The double-peak and the plateau-shaped curves occured in 17% each. The finding of an descendant curve was rare (5%). Of 623 measurements, only in 55% manouvres a positive sonotubometric result was found despite the fact that the patients reported an opening in all cases. The median opening time in dry swallowing, liquid swallowing, yawning and Valsalva was found to be 486, 355, 1,263 and 1,250 ms. A median sound increase of 16.0, 13.8, 15.0 and 15.0 dB was recorded for these manoeuvres. There was a statistic significant difference (P < 0.02) between the increase in sound intensity of liquid and dry swallowing. There was also a statistic significant difference found for the duration of the forced manoeuvres Valsalva and yawning as compared to dry and liquid swallowing (P < 0.0001). The use of an 8 kHz pure-tone signal showed a limited sensitivity for the detection of ET openings. This is mainly due to noise pollution, but also because of an altered positioning and/or dislocation of the probes and compression of the nostrils. The application of an 8 kHz signal is therefore not reliable enough for the use in practice. Further technical refinements and the use of alternative signals are necessary for a broader clinical application.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Eustachian tube (ET) plays a role in ventilation, pressure equilibration and drainage of the middle ear and the mastoid. Since physiology and the impact of ET alterations on the pathogenesis of middle ear diseases are not fully understood, numerous methods such as tympanometric, manometric, radiologic, endoscopic and sonometric approaches have been developed for the evaluation of the ET function [5, 6, 9, 17].
Most methods used in clinical routine study pressure variations in the middle ear. One major drawback of many methods is that they cannot be applied in both patients with an intact and patients with a perforated eardrum [3, 4, 10]. Furthermore, most of these approaches do not resemble physiologic conditions.
Sonotubometry is a method that allows the examinationof the ET under physiological conditions. In this approach a sound is applied via a probe in the nose. At the same time, the changes of sound intensity during tube opening are recorded in the external ear canal [24].
Various approaches are reported. Pure-tone as well as broadband stimuli were used as signals [1, 21, 25]. Some authors demonstrated that frequencies above 6 kHz are most favourable for clinical application since most noise pollution caused by pharyngeal activity occurs up to 5 kHz [20, 24, 25]. Clinical studies with this method showed uniequivocal results for the diagnostic and predictive value of this method in preoperative assessment [8, 11, 16, 22, 26].
Although the sonotubometric approach has many potential advantages, it was not able to dominate the diagnostics for Eustachian tube (dys)function. Instead tympanometry became a widespread method despite some drawbacks.
Employing modern audiologic technology, the aim of this study was to evaluate the diagnostic reliability and to find normal values for tubal opening for the application of an 8 kHz pure-tone signal in sonotubometric studies.
Patients and methods
Probands
Fourty-three clinically healthy normal subjects, 25 women and 18 men, were studied. Mean age was 26.0 (21–49) years. No individual had a history of ear diseases or nasal problems. Before the sonotubometric studies an otoscopic and rhinoscopic examination was performed. After clinical evaluation the subjects underwent pure-tone audiometry, tympanometry and rhinomametric assessment. Only patients with normal findings were admitted to the study. A written consent was obtained from each individual. In 3/43 cases, one of the examinations showed pathologic results. These individuals were excluded from further investigations. This resulted in 80 ears investigated.
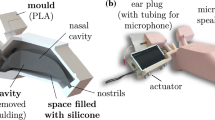
Sonotubometry device
For sonotubometric measurement a custom-made device was constructed by the Institute of Technical Acoustics. A sound generator (DSP EVM 56002, Motorola Corp., Taunusstein, Germany) generated an 8 kHz pure tone with an intensity of 60 dB at a sampling rate of 32 kHz. This tone was delivered in the nasal cavity by a loudspeaker (Sennheiser KE 4, Sennheiser Corp., Wedemark, Germany) connected with a silicon tube to the nose. To detect changes of the sound intensity during tubal opening an ear probe with a calibrated microphone (EAR Tone 3A Insert Phone, Interacoustics, Assens, Denmark) was placed in the external auditory canal. The loudspeaker and microphone were always placed on the same side of the patient so that a right ear got the sound via a right nasal cavity. To avoid an overflow of the A/D converter caused by low frequency noise components a high-pass filter (fg = 7 kHz) was introduced in the microphone pre-amplifier. After A/D conversion the microphone signal is processed by a small bandpass filter (around 8 kHz) and smoothed, in order to reduce the impact of noise by e.g. pharyngeal activity.
The method allows the registration of changes in sound intensity as well as a visualization shape of the tube opening induced by the changes of the sound intensity over the time during the tube-opening manoeuvre.
Tube-opening manoeuvres
For provocation of a tube opening, manoeuvres such as Valsalva, dry swallowing, water swallowing and yawning were performed. Every single manoeuvre was performed four times in a row. The various manoeuvres were performed before and after decongestion with xylometazoline 0.1% drops. The proband had to indicate if an increase of the loudness of the applied tone could be mentioned during the performed manoeuvre.
Evaluation of the recordings
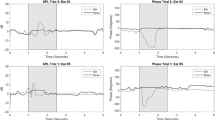
Data were stored in a PC and the resulting sonotubograms were visualized on the screen. The device was able to detect a 5 dB signal in a 110 dB noise. To classify a change in the sound intensity recorded as a valid tube opening, a sonotubogram had to show at least an increase of 5 dB during the manoeuvre. Furthermore, the proband had to report if he detected an increase of loudness in the examined ear during the manoeuvre. Only cases where both requirements were fulfilled were accepted as valid tube openings. The recorded events were analysed in a computer for further evaluation (Fig. 1).
Statistic evaluation
The mean sound intensities and durations were calculated by averaging the repeated measurements for each manoeuvre of each proband. Analyses of variance were performed for the mean sound intensity and the mean duration using the type of manoeuvre, the ear side and the status of decongestion as independent factors. For pairwise comparisons adequate t tests were calculated. All statistical analyses were performed with SAS for Windows (version 8.02).
Results
A total of 623 measurements were performed; 344 could be used for the analysis (55%). All 40 probands reported a tube opening during at least one manouevre. In 39/40 (97.5%) cases, sonotubometry was able to identify at least one opening event.
The various manoeuvres showed a wide variety in their ability to trigger individual tube activity. Most events were recorded during swallowing 57.0% (28.8% dry swallowing and 28.2% swallowing with fluid, respectively). In yawning 18.9% of the manoeuvres triggered an opening. Valsalva manoeuvre showed in 24.1% positive results (P < 0.0001).
The duration of all openings was found between 2.8 ms and 7.2 s (median 459 ms, average 705.4 ms, SD ± 711.3 ms). A median increase of sound intensity of 14.0 (0.5–40 dB, average 15.2 dB, SD ± 7.8) dB was recorded during tubal activity.
The mean duration of tube openings and the mean increase of sound intensity were 355.6 ms (SD ± 335.1, median 265.0 ms) and 13.8 dB (SD ± 7.8, median 12.5 dB) for liquid swallowing, and 486.9 ms (median 369.0 ms; SD ± 375.1) and 16.0 dB (median15.0 dB, SD ± 7.9) for dry swallowing, respectively (P < 0.0203, P < 0.0755, NS).
For Valsalva manoeuvre values of 1,250.8 ms (median 1,000 ms, SD ± 908.2) and 15.8 dB (median 15.0 dB, SD ± 7.6) were registered. In yawning a mean duration of 1,263.4 ms (median 1,000 ms, SD ± 805.4) opening time and a mean sound intensity increase of 16.5 dB (median 15.0 dB, SD ± 7.6) was recorded.
A statistic significant difference was found for the increase of sound intensity (dB) between Valsalva manoeuvre and liquid swallowing (P < 0.02). There was also a statistic significant difference found for the duration of the forced manoeuvres Valsalva and yawning, as compared to dry and liquid swallowing (P < 0.0001). There were no further statistically relevant differences found in the analyses of variance for the mean sound intensity or duration.
Four characteristic types of sonotubograms could be found. Most common was the occurrence of the spike type (Type I). Its shape is characterized by a short and steep increase of sound intensity and a subsequent rapid decrease after the peak intensity (Fig. 2). About 60.2% sonotubograms displayed this characteristic.
The second most common type was the so-called double-peak type (Type II, Fig. 3). Curves with this feature were found in 17.7%. The finding of a plateau curve (Type III, Fig. 4) and of a descendant type (Type IV, Fig. 5) occurred in 17.2 and 4.9%, respectively. Characteristic sonotubograms were mostly associated with certain manoeuvres. Spike-shaped sonotubograms were mostly seen during swallowing with water (87.6%) and dry swallowing (81.8%). Type II and III curves occurred foremost during Valsalva (25.3 and 44.6%). Yawning manoeuvres occurred foremost with the plateau and also with the spike type (46.2 and 32.3%).
The performance of a certain manoeuvre resulted on the other hand not exclusively in one sonotubogram type. The combination of two different shaped curves resulting from the same manoeuvre could be seen in 32 (80.0%) probands. These combinations occurred frequently during yawning (44.8%) and Valsalva (44.8%). In swallowing this phenomenon was rare. Only in 10.3% (3.4% dry swallowing, 6.9% swallowing with fluid) of the probands a combination was found.
Decongestion with xylometazoline lead to more pronounced sonotubogram curves (Fig. 6). Yet, the statistical analysis of the results before and after decongestion (median 459.0 ms, average 701.6 ms, SD ± 698.6; median 13,0 dB, average 14.7 dB, SD ± 7.8; median 455.0 ms, average 708.8 ms, SD ± 722.9; median 15 dB, average 15.7 dB, SD ± 7.8) showed that there was no statistic significance (P < 0.89 NS, P < 0.31 NS) between the two settings.
There was no statistic significant difference of all the results between the two ears in the same individual (P < 0.77 NS, P < 0.97 NS).
Fifty-five percent measurements performed were eligible for evaluation. The manoeuvre with the most failures was yawning (32.6%). Also Valsalva manoeuvres were susceptible for a failure of the sonotubometric measurement. The nostrils with the inserted tube have to be compressed to generate sufficient nasopharyngeal pressure for the provocation of a tube opening. In all Valsalva manoeuvres (n = 156) a tube opening was reported by the probands but sonotubometry was able to record an event in only 53.2 %.
Another reason for failures was the occurrence of a strong noise pollution. This was the case in 279 (44.8%) measurements. A false positioning of the tube in the nose or the ear probe in the ear may also have played a role.
Discussion
Eustachian tube activity can be detected by the application of an acoustic signals. A real-time monitoring of the dynamic of ET tube function under physiological conditions is possible with the method applied [24]. A number of characteristically shaped sonotubograms can be found [18, 25]. It can be assumed that the different patterns reflect at least in part the highly differentiated muscular activity of the tubal muscles.
Direct monitoring of this activity is only possible by EMG, which is an invasive procedure [13]. Magnetic resonance imaging is able to visualize muscular function but is costly and not always tolerated by the patient [14, 23]. Although sonotubograms reflect muscular activity only indirectly the results show an intra- and interindividual variability in the muscular activation that was also described with alternative methods by other groups [7, 12, 19]. There was little variability in the duration of the tubal opening during dry and liquid swallowing. This may be explained by the fact that swallowing is a reflex that cannot be stopped once triggered. The fact that spike-shaped sonotubograms were mostly found suggests that a similar muscle activation pattern occurs in this manoeuvre.
The variability of tubal opening was much higher in forced manoeuvres such as yawning (2.8 ms–5.0 s). The onset and duration of this kind of opening can be actively influenced by the proband. This is also true in part for Valsalva, the least physiologic manoeuvre investigated. The occurrence of two different types sonotubograms in the same manoeuvre reflects the forced nature of these manoeuvres. Opening and the duration of the pressure increase can be easily controlled. Since closure of the tube requires a passive decompression of the middle ear this part of tubal motility cannot be influenced. In Valsalva manoeuvre we saw most of the descending sonotubogram types. This may reflect an impaired relaxation, an individually increased rigidity or a clinically not apparent stenosis. Yet, further studies are necessary.
Sonotubometry with a 8 kHz pure-tone signal failed to demonstrate tubal opening in only 2.5% normal patients but in 45% manoeuvres. Not all manoeuvres triggered a detectable tube opening. This shows that the application of an acoustic signal is useful for ET diagnostic. Yet it also clearly demonstrates the limited sensitivity of the signal used in this study. First experiences with a new generation of acoustic signals, so-called perfect sequences, shows that other signals significantly enhance the use of sonotubometry for clinical application [2, 5, 6].
Little more than half of the measurements (55.2%) were assessable for evaluation, but there was a learning curve in the application of this method. Factors such as nasal fluid and cerumen were systematically eliminated during the course of the study. The compression of the nostrils that caused most problems during Valsalva is hard to be controlled. The dislocation of the nasal tube or the ear probe that may lead to false-negative result cannot always be avoided. Noise pollution during pharyngeal activity could not be totally eliminated by the described setting.
Since ET function is known to be influenced by various factors such as physical activity, age, body position and blood flow [15, 27], a long-term registration like a Holter ECG recording would be desirable.
Although sonotubometry offers a number of desirable advantages when compared to other methods, the results of this study demonstrate clearly that in practice the reliability of applying an 8 kHz pure-tone signal is too limited for both a short-term and a long-term registration. Further technical refinements are necessary to increase the use of this method for clinical application.
References
Andreasson L, Ivarson A, Luttrup S, Mollerstrom B, Tjernstrom O (1984) Eustachian tube function measured as pressure equilibration and sound transmission capacity. A comparison in healthy ears. J Otorhinolaryngol Relat Spec 46:74–83
Antweiler C, Antweiler M (1995) System identification with perfect sequences based on the NLMS Algorithm. AEÜ 49:129–134
Bluestone CD, Cantekin EI (1981) Panel on experiences with testing Eustachian tube function. Current clinical methods, indications and interpretation of Eustachian tube function tests. Ann Otol Rhinol Laryngol 90:552–562
Bunne M, Falk B, Magnusson B, Hellström S (2000) Variability of Eustachian tube function comparison of ears with retraction disease and normal ears. Laryngoscope 110:1389–1395
Di Martino E, Thaden R, Krombach GA, Westhofen M (2004) Eustachian tube function tests current knowledge. HNO 52:1029–1040
Di Martino E, Antweiler C, Kellner A, Vary P, Westhofen M (2004) Einsatz neuer akustischer Signale zur Tubenfunktionsuntersuchung. HNO Inf 29:104
Di Martino E, Walter LE, Westhofen M (2005) Endoscopic examination of the Eustachian Tube A step by step approach. Otol Neurootol 26:1112–1117
Filipo R, De Seta E (1991) Sonotubometry in the postoperative evaluation of tympanoplasty. In: Sade J (ed) The Eustachian tube, clinical aspects. Kugler & Ghedini, Amsterdam, pp S353–S357
Honjo I (1988) Evaluation of static and dynamic functions of the Eustachian tube. In: Honjo I (ed) The Eustachian tube in middle ear diseases. Springer, Tokyo, pp S25–S38
Ivarson A (1980) A new impedance method for measuring middle ear mechanics and Eustachian tube function. Ann Otol Rhinol Laryngol Suppl 89:207–210
Jonathan DA (1990) The predictive value of Eustachian tube function measured with sonotubometry in the successful outcome of myringoplasty. Clin Otolaryngol 15:431–434
Krombach GA, Di Martino E, Nolte-Ernsting C, Schmitz-Rode T, Prescher A, Westhofen M, Gunther RW (2000) Kernspintomografische Darstellung und Funktionsdiagnostik der Tuba auditiva Eustachii. Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 172:748–752
Leuwer R (1996) EMG analysis of muscular dysfunction in the Eustachian tube. PhD thesis, Medical Faculty University of Hamburg, Germany
Leuwer R, Schubert R, Kucinski T, Liebig T, Maier H (2002) The muscular compliance of the auditory tube—a model based survey. Laryngoscope 112:1791–1795
Malm L, Tjernstrom O, White P, Ivarsson A (1987) Effect of body position, epinephrine, and a surface-tension-lowering substance on the Eustachian tube opening in the rat. ORL J Otorhinolaryngol Relat Spec 49:138–144
Manning SC, Cantekin EI, Kenna MA, Bluestone CD (1987) Prognostic value of Eustachian tube function in pediatric tympanoplasty. Laryngoscope 103:212–216
McBride TP, Dekray C, Cunningham M, Doyle W (1988) Evaluation of noninvasive Eustachian tube function tests in normal adults. Laryngoscope 98:655–658
Mondain M, Vidal D, Bouhanna S, Uziel A (1997) Monitoring Eustachian tube opening: preliminary results in normal subjects. Laryngoscope 107:1414–1419
Muenker G (1972) Function analysis of the Eustachian tube. Methods and clinic. PhD thesis, University of Freiburg, Germany
Munro KJ, Benton CL, Marchbanks RJ (1999) Sonotubometry findings in children at high risk from middle ear effusion. Clin Otolaryngol 24:223–227
Murti KG, Stern R, Cantekin E, Bluestone CD (1980) Sonometric evaluation of Eustachian tube function using broadband stimuli. Ann Otol 89:S68, 178–184
Palva T, Virtanen H (1984) Sonotubometry in chronic ear disease. Arch Otolaryngol 110:596–599
Robert Y, Rocourt N, Gaillandre L, Lemaitre L, Francke JP (1994) Serial anatomy of the auditory tube correlation to CT and MR imaging. Surg Radiol Anat 16:63–69
Virtanen H (1977) Eustachian tube sound conduction: an acoustic method for objective measurement of auditory tubal opening. PhD thesis, Medical Faculty, University of Helsinki, Finland
Virtanen H (1978) Sonotubometry. Acta Otolaryngol 86:93–103
Virtanen H, Palva T, Jauhinen T (1980) Comparative preoperative evaluation of Eustachian tube function in pathological ears. Ann Otol 89:366–371
Virtanen H (1983) Relation of body posture to Eustachian tube function. Acta Otolaryngol 95:63–67
Acknowledgment
Part of this work was supported by the Deutsche Forschungsgemeinschaft (DFG), grant MA 3917/1–1
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Di Martino, E.F.N., Thaden, R., Antweiler, C. et al. Evaluation of Eustachian tube function by sonotubometry: results and reliability of 8 kHz signals in normal subjects. Eur Arch Otorhinolaryngol 264, 231–236 (2007). https://doi.org/10.1007/s00405-006-0172-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-006-0172-1