Abstract
The purpose was to evaluate the outcome following the surgical management of a consecutive series of 26 adult patients with laryngotracheal stenosis of varied etiologies in a tertiary care center. Of the 83 patients who underwent surgery for laryngotracheal stenosis in the Department of Otorhinolaryngology and Head and Neck Surgery, University Hospital of Lausanne, Switzerland, between 1995 and 2003, 26 patients were adults (≥16 years) and formed the group that was the focus of this study. The stenosis involved the trachea (20), subglottis (1), subglottis and trachea (2), glottis and subglottis (1) and glottis, subglottis and trachea (2). The etiology of the stenosis was post-intubation injury ( n =20), infiltration of the trachea by thyroid tumor ( n =3), seeding from a laryngeal tumor at the site of the tracheostoma ( n =1), idiopathic progressive subglottic stenosis ( n =1) and external laryngeal trauma ( n =1). Of the patients, 20 underwent tracheal resection and end-to-end anastomosis, and 5 patients had partial cricotracheal resection and thyrotracheal anastomosis. The length of resection varied from 1.5 to 6 cm, with a median length of 3.4 cm. Eighteen patients were extubated in the operating room, and six patients were extubated during a period of 12 to 72 h after surgery. Two patients were decannulated at 12 and 18 months, respectively. One patient, who developed anastomotic dehiscence 10 days after surgery, underwent revision surgery with a good outcome. On long-term outcome assessment, 15 patients achieved excellent results, 7 patients had a good result and 4 patients died of causes unrelated to surgery (mean follow-up period of 3.6 years). No patient showed evidence of restenosis. The excellent functional results of cricotracheal/tracheal resection and primary anastomosis in this series confirm the efficacy and reliability of this approach towards the management of laryngotracheal stenosis of varied etiologies. Similar to data in the literature, post-intubation injury was the leading cause of stenosis in our series. A resection length of up to 6 cm with laryngeal release procedures (when necessary) was found to be technically feasible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the majority of patients, acquired stenosis of the subglottis and trachea is due to prolonged intubation and tracheostomy. This can be attributed to the increasing use of mechanical ventilation in the intensive care units with or without tracheostomy. In the otolaryngologic community, the traditional treatment of laryngotracheal stenosis (LTS) has been laryngofissure and laryngotracheal reconstruction (LTR). However, the results with these approaches have not often been favorable in many cases [23]. For tracheal stenosis, tracheal resection and anastomosis is now accepted as the procedure of choice with excellent results reported in many large series in the literature [8, 16]. However, when the subglottis is also involved, the surgical management becomes technically more difficult. Pearson [33] reported the technique of partial cricoid cartilage resection with primary thyrotracheal anastomosis with preservation of the recurrent laryngeal nerves in 1975, after which this procedure of partial cricotracheal resection (PCTR) also became the treatment of choice for the cure of subglottic stenosis resulting from prolonged intubation or trauma. The similarities and differences of PCTR in the adult and pediatric groups have been described earlier by the senior author [27]. In the present study, we report our experience and outcome following the surgical management of 26 adult patients with LTS of varied etiologies.
Materials and methods
Patients
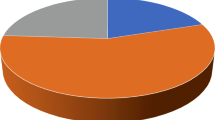
From January 1995 to December 2003, 83 laryngotracheal stenoses were treated in the Department of Otorhinolaryngology and Head and Neck Surgery, University Hospital of Lausanne, Switzerland. Fifty-seven PCTRs were done in infants and children and 26 PCTRs or tracheal resections in adults. This report focuses on all the adult cases (≥16 years). Data were retrospectively collected from hospital inpatient charts and outpatient clinic records. The latest follow-up information was assessed from questionnaires sent out to the patients and/or telephone interviews. The follow-up period ranged from 6 to 7 years (mean follow-up of 3.6 years). Data collection focused on the etiology and site of stenosis, length/type of resection, postoperative functional outcome and complications. In this study, there were 18 men and 8 women aged between 16 to 75 years (mean 51±18 years, median 53.5 years). Seventeen patients (65%) were referred cases. The stenosis involved the trachea in 20 patients, subglottis in 1 patient, subglottis and trachea in 2 patients, glottis and subglottis in 1 patient and the glottis, subglottis and trachea in 2 patients. The etiology of the LTS was post-intubation injury (20 patients), infiltration of trachea by thyroid tumor (3 patients), seeding from a laryngeal tumor at the site of tracheostoma (1 patient), idiopathic progressive subglottic stenosis (1 patient) and external laryngeal trauma (1 patient) (Fig. 1).
Nine of these 26 patients (34.6%) had some form of prior treatment elsewhere, including laser surgery (2), tracheoplasty (1), LTR (5) and tracheal resection and LTR (1). Tracheostomy was present in 12 patients (46%), and the 14 other patients (54%) had severe dyspnea at rest before resection. Prior to surgery, 9 of the 26 patients had a significant restriction of vocal cord movement with complete fixation in 2 patients.
Operative technique
All patients underwent indirect laryngoscopy, direct laryngotracheoscopy and suspended microlaryngoscopy when needed before the surgical procedure. The cricotracheal/tracheal resection was performed in a similar fashion to the technique described by Grillo and Pearson [32, 12]. We did not plicate the membranous trachea to adapt it to the luminal difference in diameter between the subglottis and trachea as proposed by Pearson et al. [33]. Instead, the lumen was made compatible by widening the cricoid plate posteriorly and by using an additional inferior midline thyrotomy [25]. This additional subglottic enlargement procedure was routinely done in children, but only in some cases in adults [27].The triangular defect was then filled with a mucosa-lined cartilaginous wedge from the first normal tracheal ring below the resected stenosis. Thyrohyoid release was performed in 13 patients (50%) to decrease the tension on the suture line. Interrupted 4.0 Vicryl sutures were used for the posterior anastomosis, with the knots tied inside the lumen. Two lateral 2.0 Vicryl sutures were placed at the inferior and posterolateral edge of the cricoid plate to secure the trachea in place and to release the tension at the site of anastomosis. Fibrin glue was used in all cases to seal the anastomotic site. For thyrotracheal anastomosis, we used 2.0 Vicryl sutures with the knots tied outside the lumen. In tracheal resection with end-to-end anastomosis, we used 3.0 or 4.0 Vicryl for the membranous part and 2.0 Vicryl for the cartilaginous part.
Eighteen patients were extubated in the operating room, and six patients were extubated during a period of 12 to 72 h, postoperatively. Two patients were decannulated at 12 and 18 months, respectively. The criteria for extubation were based on the patency of the airway, bilateral recurrent laryngeal nerve function and absence of laryngeal edema. All patients were admitted in the surgical intensive care unit for at least 48 h postoperatively and were placed on antibiotics and anti-reflux medication for a minimum of 10 days. We did not use a chin-to-thorax suture to limit the extension of the neck in the postoperative period.
Results
In this series, 20 patients underwent tracheal resection and end- to-end anastomosis, and 5 patients had partial cricotracheal resection and thyrotracheal anastomosis. The length of resection varied from 1.5 to 6 cm, with a median length of 3.4 cm (Fig. 2). Laryngotracheal reconstruction was done for one patient because of insufficient length of the trachea due to prior resections. Of the 12 patients (46%) who had prior tracheostomy, the stoma was excised along with the primary procedure in 10 patients (83%), and 2 patients needed a second procedure before decannulation (12 and 18 months after primary surgery). One patient in this series had a tracheo-esophageal fistula, which was successfully repaired along with the resection-anastomosis. Additional laser arytenoidectomy was done in two patients for cricoarytenoid ankylosis at a later date. The recurrent laryngeal nerves were not injured during surgery in 25 patients, but the nerve had to be sacrificed unilaterally in one patient because of thyroid tumor infiltration. Pathological examination of the specimens in the tumor group revealed papillary carcinoma in three and squamous cell carcinoma (tracheal seeding by a laryngeal tumor) in one. Margins were free of tumor in all these cases.
There was no perioperative mortality in this series. The immediate postoperative period was complicated by pneumonia in three patients, which was treated with antibiotics (Table 1). Mild cervical emphysema was noticed in three patients, which was treated conservatively in two patients, while the third patient required re-intubation after 12 h. Subsequently, a silicone stent had to be introduced and kept for 1 week with an uneventful recovery. Follow-up endoscopic examinations done routinely for all patients 1 week after surgery revealed minimal granulations in three patients and were successfully managed by endoscopic CO2 laser. This series had one anastomotic dehiscence, which occurred 10 days after surgery. This patient, who was operated on for a papillary carcinoma of the thyroid with tracheal infiltration, needed a revision surgery. No patients had major dysphagia or aspiration, though one patient developed delayed upper esophageal sphincter spasm. This was successfully managed by muscle re-education. The outcome and main complications of this series are compared with those of world leaders in this field (Table 2).
Long-term outcome
The long-term outcomes were classified into three categories: excellent (patient completely free of symptoms), good (dyspneic only during exertion) and failure (restenosis). In the benign group, three patients died of unrelated causes 5, 6 and 7 years after resection anastomosis, respectively. Among the surviving patients in this group, 14 patients had an excellent outcome, and 5 patients had a good outcome. No restenosis was noted in the whole series (Fig. 3). The patient in this series who had LTR was decannulated 1 year after surgery, but required multiple endoscopic procedures for better results. He was living a fully normal life at the 4-year follow-up, but complained of mild stridor on exertion. Among the four patients in the tumor group, one patient died of distant metastasis. Of the three surviving patients, outcomes were excellent in one and good in two patients, with no evidence of recurrence at the anastomotic site (mean follow-up: 2.7 years).
Preoperative and postoperative views of a grade IV subglottic stenosis secondary to external laryngeal trauma in a 28-year-old man. A Complete obstruction of the subglottis, reaching the under surface of the vocal cords. B Postoperative results at 2.5 months after PCTR: patent subglottic lumen with slight residual distortion of the posterior laryngeal commissure
Discussion
Management of laryngotracheal stenosis (LTS) is a challenging problem that demands a multidisciplinary approach performed by surgical teams well trained in this field. The various forms of treatment described for LTS include laser, repeated endoscopic dilatations, cryosurgery, prolonged stenting, laryngotracheal reconstruction and segmental resection with end-to-end anastomosis. Procedures that do not remove the diseased segment of the subglottis or trachea are associated with variable outcomes. The ideal treatment option should be individualized based on patient characteristics, as each procedure has its own advantages and disadvantages [32].However, cricotracheal/tracheal resection remains the most successful treatment for LTS [7, 16, 34] to date.
Principles of surgical management
Definitive laryngotracheal surgery should only be attempted after edema and inflammation have subsided for better anastomotic results. The principles of resection and anastomosis include meticulous dissection, avoidance of excessive anastomotic tension and preservation of tracheal blood supply and recurrent laryngeal nerves. Cricotracheal/tracheal resection helps in restoring a large lumen with a normal tracheal ring and no disruption of the cartilaginous framework, allowing full mucosal lining on both sides of the anastomosis. The tracheal ring used for the anastomosis should be normal and steady to prevent tracheomalacia at the site of the anastomosis [26]. The placement of stitches at the submucosal plane avoids granulation tissue at the suture line. Suprahyoid release, as described by Montgomery [29], increases the possibility of extended tracheal resection to almost half the length of the adult trachea. The other technique of laryngeal release, described by Dedo [9], involves cutting of the thyrohyoid membrane. We have preferred to utilize the latter technique in our resections and end-to-end anastomoses. A comparison of these two techniques by Kato et al. [19] showed that outcome regarding swallowing was better with the Montgomery technique. Contrary to the results of this study, our results show that deglutition was not a problem for all of the patients who underwent the Dedo technique. We also did not routinely perform “release” procedures in our patients, though this has been advocated by Peskind et al. [35].
Comparison of thyrotracheal and cricotracheal anastomosis by Laccourreye et al. showed increased morbidity with thyrotracheal anastomosis [21]. This was not evident in our data, with no significant differences in outcome between groups of adult patients with thyrotracheal ( n =5) and cricotracheal ( n =10) anastomosis. These data are confirmed by our larger experience in 78 pediatric PCTR patients (unpublished data). Similar to our results, Wolf et al. [42]have shown that the outcome in these groups is similar when the glottis is normal. In specific situations such as involvement of the intrinsic larynx, ancillary procedures might be indicated. These may be done combined with the primary resection or as a second procedure [28].Prolonged intubation is known to cause chondritis of the arytenoid cartilage, interarytenoid scarring and subsequent cricoarytenoid fixation [38]. This problem is not always easy to differentiate from recurrent laryngeal nerve paralysis preoperatively [4]and may necessitate a second surgery. Two patients in our series underwent laser arytenoidectomy at a later date for bilateral cricoarytenoid ankylosis. The management of this problem depends to a large extent on the surgeon’s experience with endoscopic laser treatments.
Most LTS series include a significant proportion of salvage surgeries as a result of single/multiple procedures for stenosis done in smaller centers before referral to multidisciplinary centers. In our series, 35% of the patients had had one or more surgeries before referral. It is a well-accepted fact that management of recurrent stenosis becomes more complex after previous surgical procedures. In our series, six of the eight patients (75%) undergoing salvage surgery needed laryngeal release procedures; this was higher than in the group that underwent primary surgery. However, the final functional outcome of this difficult group was similar to the results of the primary surgery group in our series. This has also been the experience with other large series reported in the literature [43, 10]. Despite the good outcome of the salvage surgery group, the postoperative course of two of these patients was prolonged, and decannulation could only be achieved after 12 and 18 months following a second procedure.
Complications and outcome
The major complication that occurred in our series was an anastomotic dehiscence for one patient (4% of the series). This patient had undergone resection of 3 cm of trachea (the mean resection length in our series was 3.4 cm). Dehiscence is usually attributed to excessive tension at the anastomotic site or to an infected airway at the time of surgery. No specific factor in the surgical technique or postoperative management of this patient could be identified as contributing to the dehiscence. The rate of dehiscence (4%) in our series is similar to that reported in the literature, which ranges between 5 and 7.5% [6, 16]. In a review of complications of 416 primary tracheal surgeries (including 279 post intubation lesions), suture line granulation was found to decrease markedly with the use of absorbable Vicryl sutures [14]. In our study, only three patients were found to have granulations, which were treated with endoscopic CO2 laser ablation and mitomycin-C application. The low rate of granulations in our series is a result of using absorbable sutures that were placed in the submucosal plane.
A study of 35 patients with chronic tracheal stenosis (thyroid tumor invasion, 18 patients; prolonged intubation/trauma, 17 patients) revealed a successful outcome for all patients after segmental resection with end-to-end anastomosis [19]. In a study comparing primary and revised procedures for segmental resection and anastomosis of LTS, Wolf et al. [42] showed a decannulation rate of 95.6%, with no major differences in the two subgroups studied. Similar excellent results were documented in the series of Macchiarini et al. (93% of 45 patients with CTR) and Rea et al. (95% of 65 patients with tracheal resection) [22, 36]. Contrary to these results of resection with anastomosis, laryngotracheal reconstructions (LTR) have not been as successful especially in grade III and IV subglottic stenoses according to the Myer and Cotton classification [30]. In a group of 15 patients described by Rhee et al. who underwent a single stage LTR, decannulation was possible in 14, and one patient died in the peri-operative period [37]. However, most of these patients needed 1 to 15 additional surgeries before decannulation could be achieved. In our series of 25 patients with cricotracheal or tracheal resection, 21 surviving patients live without a tracheostomy, and none of the patients has developed restenosis. The only patient who had an LTR (due to an insufficient length of trachea due to prior resections) needed multiple interventional endoscopies before successful decannulation. Overall, the excellent result of resection and primary anastomosis makes it more effective and reliable in managing LTS.
Post-intubation stenosis
Post intubation injury (prolonged endotracheal tube/tracheostomy) was the predominant cause of LTS (20 of 26 patients) in our series. Inflammation of the mucosa, submucosa and cartilage of the subglottis and trachea leads to thickening and scarring of the epithelium and submucosa, resulting in stenosis [31]. The use of low pressure, large volume cuffs has been noted to reduce the incidence of LTS [13]. The incidence of subglottic stenosis in intubated neonates has been reported to be 0–2% and found to have decreased compared to previous years [41]. Zietek et al. [44] have reported on 36 cases of stenosis comprising 14 of the larynx and 22 of the trachea with prolonged intubation as the cause of stenosis in 47% and tracheostomy in 36% of cases.
In one patient of our series, the stenosis was secondary to a percutaneous dilatational tracheostomy (PDT). Klussmann et al. [20]. reported a case of complete stenosis of the trachea following a second PDT in one patient. Incidence of tracheal stenosis secondary to PDT ranges from 0 to 5% in the few studies reported in the literature [5, 24]. Briche et al. have reported two cases of tracheal stenosis secondary to PDT [3], which was treated by resection anastomosis and endoluminal conformer, respectively. The patient in our series with tracheal stenosis secondary to PDT was effectively managed with segmental resection and cricotracheal anastomosis.
Idiopathic progressive subglottic stenosis
Our series also included a 54-year-old male patient with idiopathic progressive subglottic stenosis (IPSS). The diagnosis was made after excluding causes of stenosis such as infection, inflammation, trauma, gastroesophageal reflux disease, relapsing polychondritis or Wegner’s granulomatosis. The site of stenosis was at the level of the upper trachea and measured 2 cm. This patient was treated successfully with resection and end-to- end anastomosis after failed prior attempts at laser resection at another center. Grillo et al. have reported single-stage resection and anastomosis in 39 patients with IPSS, with good results in 32 patients [15]. The use of laser in the management of IPSS has also been reported by Benjamin et al. [1]. Based on an analysis of 30 patients with IPSS, Giudice et al. have suggested that open neck surgery should be considered only if endoscopic laser resection and dilatation fails [11]. The chances of failure of endoscopic laser treatment in the management of IPSS are known to be associated with thicker stenosis [40]. Though thinner stenosis responds well to laser resection, repeated laser treatment for larger lesions can increase the extent of injury with restenosis in most of the patients. Our patient with IPSS had an excellent outcome with resection anastomosis with no restenosis (follow-up period: 6 months).
Tumors infiltrating the trachea
This series also included three patients with thyroid carcinoma and one patient with seeding of a laryngeal cancer at the tracheostoma site (10 months after partial laryngectomy). All of them presented with stridor and hemoptysis and underwent resection and primary anastomosis. The earlier treatment of “shaving” the tumor off the trachea is associated with high recurrence rates. Ishihara et al. [18] have documented that the survival rate of patients treated by complete resection are better than those treated by inadequate tumor resections. Yang et al. [43]have reported resection management in eight patients with thyroid cancer infiltrating the trachea, with no evidence of disease in five patients with a mean follow-up of 91 months. Good results have also been shown by Hammoud et al. [17], who have suggested that tracheal resection and reconstruction should be considered for thyroid tumors with airway involvement, which might provide long-term palliation or cure in most patients. All of the tumor patients in our series had an immediate disappearance of symptoms of obstruction after surgery. Margins were free of tumor in all cases. One patient died after 6 months because of distant metastasis, and the other three are asymptomatic after a mean follow-up period of 2.7 years. We believe that for malignant stenotic lesions, radical resection procedures should be the treatment of choice, when technically feasible.
External laryngeal trauma
Blunt trauma to the larynx requires early diagnosis and treatment to avoid acute complications and long-term sequelae. The one patient in our series who developed subglottic stenosis secondary to direct laryngeal trauma presented to us 4 years after the injury. Despite 14 interventions at multiple centers, decannulation could not be achieved. Following PCTR with primary resection of the tracheostoma at our center, a satisfactory lumen could be achieved, which allowed extubation (Fig. 3). At the follow-up evaluation 2 years after surgery, the patient only had slight dyspnea on exertion. Other clinical case series have stressed the importance of early intervention to avoid the complications and progression to LTS in external laryngeal trauma [2, 39]. The treatment of choice for established stenosis will be a PCTR or tracheal resection and primary anastomosis similar to post-intubation stenosis. The use of the laser should be restricted to a non-circular scar or an arytenoidectomy for vocal cord paralysis or cricoarytenoid joint ankylosis. The outcome of laryngeal trauma to a large extent depends on the severity of the initial injury and the timing and quality of the primary treatment. Recent improvements in management have allowed improved outcome, even in severe injuries.
Conclusion
The excellent functional results of cricotracheal/tracheal resection and primary anastomosis in our series demonstrate the efficacy and reliability of this approach towards the management of laryngotracheal stenosis of varied etiologies. Similar to data reported in the literature, post-intubation injury was the leading cause of stenosis in our series. A resection length of up to 6 cm with laryngeal release procedures (when necessary) was found to be technically feasible. The functional results of patients undergoing salvage surgery were as good as those after primary surgery in our series; however, the surgery and the postoperative clinical course were more complex in the salvage surgery group. This underlines the importance of offering the ideal surgical treatment at the first instance. The choice of the treatment option for a particular patient should be carefully made based on the severity and extent of stenosis.
References
Benjamin B, Jacobson I, Eckstein R (1997) Idiopathic subglottic stenosis: diagnosis and endoscopic laser treatment. Ann Otol Rhinol Laryngol 106:770–774
Bent JP, Silver JR, Porubsky ES (1993) Acute laryngeal trauma: a review of 77 patients. Otolaryngol Head Neck Surg 109:441–449
Briche T, Manach YL, Pats B (2001) Complications of percutaneous tracheostomy. Chest 119:1282–1283
Carrat X, Verhulst J, Duroux S, Pescio P, Devars F, Traisac L (2000) Postintubation interarytenoid adhesion. Ann Otol Rhinol Laryngol 109:736–740
Cigalia P, Graniero KD (1992) Percutaneous dilatational tracheostomy: results and long-term follow-up. Chest 101:464–467
Couraud L, Bruneteau A, Martigne C, Meriot S (1982) Prevention and treatment of complications and sequelae of tracheal resection anastomosis. Int Surg 67:235–239
Couraud L, Brichon PY, Velly JF (1988) The surgical treatment of inflammatory and fibrous laryngotracheal stenosis. Eur J Cardiothorac Surg 2:410–415
Couraud L, Jougon J, Velly JF, Klein C (1994) Sténoses iatrogènes de la voie respiratoire. Evolution des indications therapeutiques. Ann Chir Thoracic Cardiovasc 48:277–283
Dedo HH, Fishman NH (1969) Laryngeal release and sleeve resection for tracheal stenosis. Ann Otol Rhinol Laryngol 78:285–289
Donahue DM, Grillo HC, Wain JC, Wright CD, Mathisen DJ (1997) Reoperative tracheal resection and reconstruction for unsuccessful repair of post intubation stenosis. J Thorac Cardiovasc Surg 114:934–939
Giudice M, Piazza C, Foccoli P, Toninelli C, Cavaliere S, Peretti G (2003) Idiopathic subglottic stenosis: management by endoscopic and open neck surgery in a series of 30 patients. Eur Arch Otorhinolaryngol 260:235–238
Grillo HC (1969) The management of tracheal stenosis following assisted respiration. J Thorac Cardiovasc Surg 57:52–71
Grillo HC, Cooper JD, Geffin B, Pontoppidan H (1971) Low pressure cuff for tracheostomy tubes to minimise tracheal injury: a comparative clinical trail. J Thorac Cardiovasc Surg 62:898–907
Grillo HC, Zannini P, Michelassi F (1986) Complications of tracheal reconstruction. Incidence, treatment, and prevention. J Thorac Cardiovasc Surg 91:322–328
Grillo HC, Mark EJ, Mathisen DJ, Wain JC (1993) Idiopathic laryngotracheal stenosis and its management. Ann Thorac Surg 56:80–87
Grillo HC, Donahue DM, Mathisen DJ, Wain JC, Wright CD (1995) Post intubation tracheal stenosis: treatment and results. J Thorac Cardiovasc Surg 109:486–492
Hammoud ZT, Mathisen DJ (2003) Surgical management of thyroid carcinoma invading the trachea. Chest Surg Clin N Am 13:359–367
Ishihara T, Kobayashi K, Kikuchi K, Kato R, Kawamura M, Ito K (1991) Surgical treatment of advanced thyroid carcinoma invading the trachea. J Thorac Cardiovasc Surg 102:717–720
Kato I, Iwatake H, Tsutumi K, Koizuka I, Suzuki H, Nakamura T (2003) End-to-end anastomosis in chronic tracheal stenosis. Auris Nasus Larynx 30:S69–S73
Klussmann JP, Brochhagen HG, Sittel C, Eckel HE, Wassermann K (2001) Atresia of the trachea following repeated percutaneous dilatational tracheotomy. Chest 119:961–964
Laccourreye O, Bransu D, Seckin S, Hans S, Biacabe B, Laccourreye H (1997) Cricotracheal anastomosis for assisted ventilation –induced stenosis. Arch Otolaryngol Head Neck Surg 123:1074–1077
Macchiarini P, Verhoye JP, Chapelier A, Fadel E, Dartevelle P (2001) Partial cricoidectomy with primary thyrotracheal anastomosis for post intubation subglottic stenosis. J Thorac Cardiovasc Surg 121:68–76
Maddaus MA, Toth JL, Gullane PJ, Pearson FG (1992) Subglottic tracheal resection and synchronous laryngeal reconstruction. J Thorac Cardiovasc Surg 104:1443–1450
McFarlane C, Denholm SW, Sudlow CL, Moralee SJ, Grant IS, Lee A (1994) Laryngotracheal stenosis: a serious complication of percutaneous tracheostomy. Anaesthesia 49:38–40
Monnier P, Savary M, Chapuis G (1993) Partial cricoid resection with primary tracheal anastomosis for subglottic stenoses in infants and children. Laryngoscope 103:1273–1283
Monnier P, Savary M, Chapuis G (1995) Cricotracheal resection for pediatric subglottic stenosis. Update of the Lausanne experience. Acta Otorhinolaryngol Belg 49:373–382
Monnier P, Lang F, Savary M (1999) Cricotracheal resection for adult and pediatric subglottic stenoses: similarities and differences. Operative techniques. Otolaryngol Head Neck Surg 10:311–315
Monnier P, Lang F, Savary M (2003) Partial cricotracheal resection for pediatric subglottic stenosis: a single instituition’s experience in 60 cases. Eur Arch Otorhinolaryngol 260:295–297
Montgomery WW (1974) Suprahyoid release for tracheal stenosis. Arch Otolaryngol 99:255
Myer CM, O’Connor DM, Cotton RT (1994) Proposed grading system for subglottic stenosis based on endotracheal tube sizes. Ann Otol Rhinol Laryngol 103:319–323
Parkins JL, Stevens MH, Jung AL (1976) Acquired and congenital subglottic stenosis in the infant. Ann Otol Rhinol Laryngol 85:573–581
Pearson FG, Andrews MJ (1971) Detection and management of tracheal stenosis following cuffed tube tracheostomy. Ann Thoracic Surg 12:359–374
Pearson FG, Cooper JD, Nelems JM, Van Nostrand AWP (1975) Primary tracheal anastomosis after resection of the cricoid cartilage with preservation of recurrent laryngeal nerves. J Thorac Cardiovasc Surg 70:806–816
Pearson FG, Brito-Filomeno L, Cooper JD (1986) Experience with partial cricoid resection and thyrotracheal anastomosis. Ann Otol Rhinol Laryngol 95:582–585
Peskind SP, Stanley RB, Thangadurai D (1993) Treatment of compromised trachea with sleeve resection and primary repair. Laryngoscope 103:203–211
Rea F, Callegaro D, Loy M, et al (2002) Benign tracheal and laryngotracheal stenosis: surgical treatment and results. Eur J Cardiothorac Surg 22:352–356
Rhee JS, Toohill RJ (2001) Single-stage adult laryngotracheal reconstruction without stenting Laryngoscope 111:765–768
Rovo L, Jori J, Brazozka M, Czigner J (1999) Minimally invasive surgery for posterior glottic stenosis. Otolaryngol Head Neck Surg 121:153–156
Schaefer SD (1992) The acute management of external laryngeal trauma. A 27-year experience. Arch Otolaryngol Head Neck Surg 118:598–604
Valdez TA, Shapshay SM (2002) Idiopathic subglottic stenosis revisited. Ann Otol Rhinol Laryngol 111:690–695
Walner DL, Loewen MS, Kimura RE (2001) Neonatal subglottic stenosis—incidence and trends. Laryngoscope 111:48–51
Wolf M, Shapira Y, Talmi YP, Novikov I, Kronenberg J, Yellin A (2001) Laryngotracheal anastomosis: primary and revised procedures. Laryngoscope 111:622–627
Yang CC, Lee CH, Wang LS, Huang BS, Hsu WH, Huang MH (2000) Resectional treatment for thyroid cancer with tracheal invasion. Arch Surg 135:704–707
Zietek E, Matyja G, Kawczynski M (2001) Stenosis of the larynx and trachea:diagnostics and treatment. Otolaryngol Pol 55:515–520
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
George, M., Lang, F., Pasche, P. et al. Surgical management of laryngotracheal stenosis in adults. Eur Arch Otorhinolaryngol 262, 609–615 (2005). https://doi.org/10.1007/s00405-004-0887-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-004-0887-9