Abstract
The purpose of this study was to assess the feasibility of sentinel lymph node (SLN) biopsy in thyroid neoplasms. Ten patients with uninodular thyroid disease and no evidence of lymph node metastases were examined. Lymph node mapping was performed by preoperative lymphoscintigraphy and intraoperative use of a hand-held gammaprobe. Following thyroidectomy, the SLN(s) were selectively excised and worked-up histologically for occult metastases. Overall detection of SLNs was possible in 50% of the cases with lymphoscintigraphy and in 100% with the gammaprobe. All SLNs in the lateral compartment and upper mediastinum were accurately detected with lymphoscintigraphy. One patient with a papillary carcinoma showed a metastasis in the SLN. One patient experienced temporary lesion of the recurrent laryngeal nerve. In conclusion, sentinel lymph node biopsy is technically feasible. The combination of lymphoscintigraphy and gammaprobe accurately reveals SLNs in the central and lateral compartment and in the mediastinum. Search for SLNs in the lower central compartment enhances the risk of injuring the recurrent laryngeal nerve. The clinical relevance of SLN biopsy in papillary thyroid cancer is unclear, and the subgroup of patients benefiting from it has still to be defined.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
It is well known that papillary thyroid carcinoma predominantly metastasizes into regional lymph nodes [24]. In cases with clinically or radiographically apparent lymph node involvement, there is no debate about the prognostic benefit of a neck dissection in addition to the total thyroidectomy [16, 24]. The management of nodal negative tumors is still controversial. From "wait and see" as the most conservative attitude to "node picking" or even prophylactic neck dissection as the most aggressive option, all suggestions are found in the current literature [4, 16, 24]. For the decision for or against prophylactic neck dissection in papillary thyroid carcinoma, the high incidence (10–15%) of recurrent disease in the regional lymph nodes [15, 18] and the impressive rate of occult nodal disease (40–90%) [3, 19] found in elective neck dissections stand in contrast to large scale studies that were not able to attribute the status of an independent prognostic factor to nodal involvement [13, 16, 24]. To date, there is no evidence in the literature proving a general benefit of prophylactic neck dissection for papillary thyroid cancer, though some studies suggest a decrease of regional recurrence and improvement of survival for high risk patients [6, 10, 14, 16, 21, 22, 23, 25, 29]. With regard to the lack of data, the costs, the inconvenience for the patients and the potential risks of this procedure, e.g., lesion of the recurrent laryngeal nerve during dissection of the central compartment, most centers currently are favoring a conservative policy. Our policy for well-differentiated thyroid cancer staged cN0 is not to dissect the cervical lymph nodes as, based on the available data, we doubt that there is any benefit of elective treatment for the patient in terms of outcome.
The sentinel lymph node (SLN) concept has been successfully introduced in the field of surgical oncology for different tumors with predominantly nodal spread and high risk for occult disease [1, 12, 17, 26, 28]. Analogously, for papillary thyroid tumors the sentinel node biopsy has the potential to identify and stage regional lymph node disease without performing a prophylactic neck dissection. Its accuracy and safety has been addressed in several studies by the use of a blue dye as a tracer, as well as in a few trials using a radioisotope [2, 5, 7, 8, 11, 20]. Most probably, SLN biopsy will never achieve clinical relevance as a standard treatment for all patients with thyroid papillary cancer, but might play a role in a subgroup of high-risk patients. As a center with a particular research interest and experience in sentinel node biopsy, we had to define our attitude towards this topic. In order to gain personal experience, we conducted a pilot study to assess the feasibility and detect possible technical pitfalls of the preoperative lymphatic mapping by lymphoscintigraphy and the sentinel lymph node biopsy guided by the intraoperative use of a hand-held gammaprobe in patients with uninodular thyroid neoplasms.
Subjects and methods
The protocol of this study has been approved by the local Ethics Committee, and the patients were entered into the study after they had given written informed consent.
Patients with uninodular thyroid disease suspicious for malignancy on fine-needle aspiration biopsy and no evidence of lymph node disease as assessed by B-mode ultrasonography were eligible for the study. Exclusion criteria were prior radiotherapy or surgery in the neck, pregnancy or lactation.
The lymph node mapping was performed by preoperative lymphoscintigraphy and intraoperative use of a hand-held gammaprobe (Neo 2000, Neoprobe Corporation, Dublin, Ohio). Patients underwent lymphoscintigraphy 2 h before surgery. A sulfur colloid with a particle size of 20 to 80 nm labeled with Technetium-99m (Nanocoll, Nycomed Amershan, Sorin, Italy) was used for scintigraphy. Under ultrasound guidance one single injection of 20 MBq in a volume of 0.2 ml normal saline was administered. According to the technique used in mucosal squamous cell carcinoma [1, 26, 28] and malignant melanoma [17], we initially injected four peritumoral spots of normal appearing thyroid tissue. As this technique turned out to be very difficult and resulted in spillage of the radiotracer outside the thyroid, we changed the protocol and proceeded with a single intratumoral injection. The lymphatic drainage was monitored dynamically with a gamma camera (Siemens Diacam, Germany) in the anteroposterior projection from the time of injection on until accumulation of the radiotracer in the SLN occurred. Then, static imaging in both the anterioposterior and lateral views were performed, and the location of the SLN was marked on the patient's skin surface.
In the operating room a formal hemithyroidectomy through a low collar incision was performed to resect the nodule. The recurrent laryngeal nerve was monitored throughout the entire procedure with intralaryngeal wire electrodes. No frozen sections of the thyroid specimens were taken. With the aid of the gammaprobe the central compartment was searched for hot spots through the cervical incision. The lateral compartments of the neck were bilaterally scanned with the gammaprobe through the intact skin. Hot nodes were selectively excised. The activity of the lymphatic bed had to drop to background level after excision of the SLN(s). The location of the SLN(s) was noted. No prophylactic neck dissection was performed. The extensive histologic work-up of the SLN and the description of occult metastases were carried out according to the technique described in previous studies by Stoeckli et al. [27] and Hermanek et al. [9]. All step-sections were stained for H and E and cytokeratin.
Results
As approved by the local Ethics Committee, a total of ten consecutive patients (eight females) with a mean age of 50 years (age range: 20–74 years) meeting the inclusion criteria were prospectively enrolled in this pilot study.
In the first four patients, the radiotracer was injected under ultrasound guidance in four peritumoral spots of normal appearing thyroid tissue. In none of these cases could a SLN be detected by lymphoscintigraphy. Intraoperatively, high levels of radioactivity were found in both the thyroid lobe and the perithyroid muscular tissue, impeding detection of a SLN with the gammaprobe. Therefore, the protocol was changed and the radiotracer injected intratumorally in the remaining six cases. Out of these six cases, lymphoscintigraphy was able to detect the SLN in three patients (50%). With the aid of the gammaprobe, the SLN was finally found in all six patients. The SLN was located in the ipsilateral central compartment (level VI) in three cases, and in the ipsilateral lateral compartment in three cases, of which two were in level IV (near the jugular vein) and one in level II (the jugulodigastric node). Lymphoscintigraphy correctly identified the SLN in level II and two SLNs in the lower level VI. SLNs localized very close to the thyroid tumor as the two SLNs in level IV and one SLN in the upper level VI were missed by lymphoscintigraphy. Three patients revealed three and the other three only one SLN. In one of the latter patients, remaining radioactivity was detected with the gammaprobe after excision of one SLN in the deep ipsilateral level VI. This potential node could not be reached through the collar incision and was left behind.
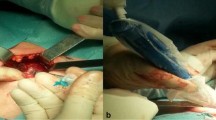
Histologic work-up of the thyroid specimens of the latter six patients revealed three patients with minimally invasive follicular carcinoma, two with follicular adenoma and one with a papillary carcinoma. One of the three SLNs in the patient with a papillary carcinoma showed metastatic disease (Fig. 1). All other SLNs were free of tumor.
As to procedure-related complications, one patient experienced a temporary lesion of the recurrent laryngeal nerve during dissection of the lower central compartment for the search for a SLN. This patient recovered completely from hoarseness within 6 weeks, showing normal vocal cord motility as assessed by direct laryngoscopy and videostroboscopy at that time. No further intra- or postoperative complications occured.
Discussion
The aim of our pilot study was to assess the technical feasibility of sentinel lymph node biopsy with a radiotracer in patients presenting with uninodular thyroid disease suspicious for malignancy. As we were conducting a technical feasibility study for a procedure and not a clinical outcome trial, not only patients with proven papillary carcinomas, but also a series of patients with uninodular thyroid neoplasms, were included. SLN biopsy has been introduced in the field of malignant melanoma, breast cancer, oral squamous cell carcinoma and other tumors with great reliability and accuracy [1, 12, 17, 26, 28]. It allows the histological staging of the lymphatic drainage without excising the whole lymphatic basin. By doing this, patients who benefit from extended lymphatic dissection can be selected, and the others can be spared the risks and costs of this procedure. In contrast to most other malignancies with preferentially lympatic spread, the stage of lymph node involvement seems not to be a general prognosticator in differentiated thyroid cancer [4, 16, 24]. Therefore, we can not expect any benefit with regard to survival from disclosing occult metastatic neck disease by SLN biopsy in all patients. However, more recent studies have come up demonstrating an elevated regional failure rate and prognostic impact of neck metastases in a subset of high-risk patients [6, 10, 14, 16, 21, 22, 23, 25, 29]. Unfortunately, all these studies only address palpable or imaging-detectable lymph nodes or macrometastatic disease as discovered by neck dissection. The impact of occult metastatic lymph node involvement on recurrence and survival has not yet been elucidated prospectively. The question still remains: is a cN0 neck that turns out to be a pN+ (mi) (sn) [9] neck rather comparable to a pN0 neck or to a pN+ neck? Or, in other words, is occult metastatic lymph node disease in high-risk groups an independent prognosticator that should be therapeutically addressed? Though the high-risk cohort of patients with advanced age, gross tumor extent, distant metastases or large tumor size might be the group to study for a potential benefit of SLN biopsy, the trial to resolve this question is very unlikely to succeed. With regard to the high cure rate and the slow growing pattern of papillary thyroid cancer, the number of patients and the duration of such a study probably exceeds by far what is feasible. Further, occult metastases as an independent prognosticator would have to compete in this high-risk setting with all the aforementioned strong prognosticators. In conclusion, we think that the benefit of SLN biopsy is hard to prove, but it could be the way to go for those who believe in prophylactic neck dissections in papillary thyroid cancer.
Most previous studies used the intraoperative injection of a blue dye to trace the lymphatics to the SLN [2, 7, 8, 11]. There are several disadvantages of this technique. First of all, lymphatics that run out of the central compartment can not be followed through the collar incision for thyroidectomy. Further, dissection of the thyroid node for injection, even if done very gently, bares the risk of interrupting important lymphatic vessels, and finally, to recognize a node as being blue is not always that easy. To overcome these drawbacks in our study we used a preoperative ultrasound guided injection of a radiocolloid instead of a blue dye to trace the SLN. The combination of lymphoscintigraphy and the intraoperative use of a hand-held gammaprobe were used to localize the SLN. This technique allows the assessment of the entire neck and mediastinum, and all the surgical dissection is done after accumulation of the tracer in the SLN. The sensitivity of lymphoscintigraphy turned out to be only 50%. This result is in agreement with the findings of two previous studies [5, 20], which both reported a sensitivity of lymphoscintigraphy of 66%. In contrast to other entities like malignant melanoma, breast carcinoma or squamous cell carcinoma of the oral cavity, lymphscintigraphy seems not to be equally successful in SLN biopsy for thyroid malignancies. But, all the SLNs missed by lymphoscintigraphy were very close to the injection site and most probably hidden behind the thyroid in the paratracheal space. In contrast, all distant SLNs (lateral compartment or lower central compartment) were adequately revealed. Therefore, the role for lymphoscintigraphy is mainly to address SLNs that might not be localized in the vicinity of the thyroid tumor. SLNs close to the primary are easily detected with the gammaprobe after removal of the thyroid. The information about the need to extend the skin incision or even to perform additional skin incisions for nodes in the lateral compartments or about the increased risk of nerve damage during the search for nodes in the lower central compartment are crucial for the patient and the surgeon. It is always much easier to handle the gammaprobe when the surgeon has a rough idea where to look for the SLN. Therefore, despite the low overall sensitivity, we still recommend the performance of preoperative lymphoscintigraphy.
In order to perform lymphoscintigraphy we injected the radiotracer preoperatively under ultrasound guidance. The initial attempt to inject four spots of healthy tissue around the tumor as suggested for all other cancers showed up to be detrimental because of spillage of the colloid into the surrounding tissue, impeding any further evaluation. According to the published studies [2, 5, 7, 11, 20, 27] about SLN biopsy for thyroid cancer, we changed our protocol and continued with direct intratumoral injections. This technique worked out very well, and with the aid of the handheld gammaprobe the detection and excision of the SLN was possible in all remaining cases.
In conclusion, where lymphatic mapping is concerned, the combination of preoperative lymphoscinitigraphy and intraoperative gammaprobe is recommended. The injection of the radiotracer should be intratumoral and is best performed preoperatively under ultrasound guidance. With regard to the good results reported with the use of a blue dye, the combination of a radiotracer and a blue dye might enhance the identification rate of the SLN [5].
Irrespective of the localization techniques, the excision of all SLNs was not always possible. In one particular case a second SLN was detected with the gammaprobe deep in the fatty tissue of the retrosternal central compartment. Excision of this node was not possible through the low collar approach so that it had to be left behind. This problem was also encountered by Kelemen et al. [11] and Dixon et al. [7]. In their studies the blue staining lymphatics ran to the mediastinum in 2 out of 17, and 2 out of 40 patients, respectively, impeding the excision of these SLNs.
As to procedure-related complications in our series, one patient experienced a temporary lesion of the recurrent laryngeal nerve. Intraoperative nerve stimulation proved the nerve to be intact after thyroidectomy. Exploration of the lower central compartment for a SLN caused bleeding from a small blood vessel, which was controlled by bipolar cautery. After this maneuvre the answers of the recurrent laryngeal nerve to the nerve stimulator were lost. We assume that the nerve underwent thermal damage during coagulation. These cases illustrate that the SLN of a thyroid cancer can be located in the lower central compartment and that its excision might be difficult or even impossible in some cases and bare the risk of injuring the recurrent laryngeal nerve.
Even in our small series with only one thyroid nodule turning out to be a papillary cancer, occult metastatic disease of the considerable size of 4.2 mm in diameter was disclosed by sentinel node biopsy, underlining the potential of this technique.
With regard to the results of the currently available studies about SLN biopsy in differentiated thyroid cancer, it can be stated that this technique is feasible with a high chance of detecting the SLN. The accuracy as elucidated by studies performing neck dissections after SLN biopsy is also fairly high [2, 8, 11]. Centers favoring prophylactic treatment of the lymph nodes in papillary thyroid cancer patients might think about performing SLN biopsy to reduce the number of unnecessary neck dissections.
Though technically feasible and a minor procedure, in our opinion SLN biopsy remains an overtreatment for N0 papillary carcinoma, unless a subset of high-risk patients is defined that will benefit from elective neck treatment in terms of survival. The SLN concept works out well only in tumors in which detection and treatment of lymph node metastases has an impact on outcome. With regard to this and the potential risks of the procedure we will not change our current policy.
References
Alex JC, Sasaki CT, Krag DN, Wenig B, Pyle PB (2000) Sentinel lymph node radiolocalization in head and neck squamous cell carcinoma. Laryngoscope 110: 198–203
Arch-Ferrer J, Velazquez D, Fajardo R, Gamboa-Dominguez A, Herrera MF (2001) Accuracy of sentinel lymph node in papillary thyroid carcinoma. Surgery 130: 907–913
Attie JN, Khafif RA, Steckler RM (1971) Elective neck dissection in papillary carcinoma of the thyroid. Am J Surg 22: 464–471
Ballantyne AJ (1991) Neck dissection for thyroid cancer. Semin Surg Oncol 7: 100–106
Catarci M, Zaraca F, Angeloni R, Mancini B, De Filippo MG, Massa R, Carboni M, Pasquini G (2001) Preoperative lymphoscintigraphy and sentinel lymph node biopsy in papillary thyroid cancer. A pilot study. J Surg Oncol 77: 21–24
Coburn MC, Wanebo HJ (1992) Prognostic factors and management considerations in patients with cervical metastases of thyroid cancer. Am J Surg 164: 671–676
Dixon E, McKinnon GJ, Pasieka JL (2000) Feasibility of sentinel lymph node biopsy and lymphatic mapping in nodular thyroid neoplasms. World J Surg 24: 1396–1401
Fukui Y, Yamakawa T, Taniki T, Numoto S, Miki H, Monden Y (2001) Sentinel lymph node biopsy in patients with papillary carcinoma. Cancer 92: 2868–2874
Hermanek P, Hutter RVP, Sobin LH, Wittekind C (1999) Classification of isolated tumor cells and micrometastasis. Cancer 86: 2668–2673
Hughes CJ, Shaha AR, Shah JP, Loree TR (1996) Impact of lymph node metastasis in differentiated carcinoma of the thyroid: A matched pair analysis. Head Neck 18: 127–132
Kelemen PR, Van Herle AJ, Giuliano AE (1998) Sentinel lymphadenectomy in thyroid malignant neoplasms. Arch Surg 133: 288–292
Krag DN (1993) Surgical resection and radiolocalization of the SLN in breast cancer using a gamma probe. Surg Oncol 2: 335–340
Lin JD, Liou MJ, Chao TC, Weng HF, Ho YS (1999) Prognostic variables of papillary and follicular thyroid carcinoma patients with lymph node metastases. Endocr Relat Cancer 6: 109–115
Mazzaferri EL, Jhiang SM (1994) Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 97: 418–428
McConahey WM, Hay ID, Woolner LB, van Heerden JA, Taylor WF (1986) Papillary thyroid cancer treated at the Mayo Clinic 1946 through 1970. Mayo Clin Proc 61: 978–996
McHenry CR, Rosen IB, Walfish PG (1991) Prospective management of nodal metastases in differentiated thyroid cancer. Am J Surg 162: 353–356
Morton DL, Wen DR, Wong JH, Economou JS, Cagle LA, Storm FK, Foshag LJ, Cochran AJ (1992) Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 127: 392–399
Noguchi M, Kinami S, Kinoshita K, Kitagawa H, Thomas M, Miyazaki I, Michigishi T, Mizukami Y (1993) Risk of bilateral cervical lymph node metastases in papillary thyroid cancer. J Surg Oncol 52: 155–159
Noguchi S, Noguchi A, Murakami N (1970) Papillary carcinoma of the thyroid. The value of prophylactic lymph node excision. Cancer 26: 1061–1064
Rettenbacher L, Sungler P, Gmeiner D, Kässmann H, Galvan G (2000) Detecting the sentinel lymph node in patients with differentiated thyroid carcinoma. Eur J Nucl Med 27: 1399–1401
Sanders LE, Cady B (1998) Differentiated thyroid cancer. Reexamination of risk groups and outcome of treatment. Arch Surg 133: 419–425
Scheumann GFW, Gimm O, Wegener G, Hundeshagen H, Dralle H (1994) Prognostic significance and surgical management of locoregional lymph node metastases in papillary thyroid cancer. World J Surg 18: 559–567
Sellers M, Beenken S, Blankenship A, Soong SJ, Turbat-Herrera E, Urist M, Maddox W (1992) Prognostic significance of cervical lymph node metastases in differentiated thyroid cancer. Am J Surg 164: 578–581
Shaha AR (1998) Management of the neck in thyroid cancer. Otolaryngol Clin North Am 31: 823–831
Sherman SL, Brierley JD, Sperling M, Ain KB, Bigos ST, Cooper DS, Haugen BR, Ho M, Ladenson PW, Robbins J, Ross DS, Specker B, Taylor T, Maxxon HR (1998) Prospective multicenter study of thyroid carcinoma treatment. Cancer 83: 1012–1021
Shoaib T, Soutar DS, Prosser JE, Dunaway DJ, Gray HW, McCurrach GM, Bessent RG, Robertson AG, Oliver R, MacDonald DG (1999) A suggested method for sentinel node biopsy in squamous cell carcinoma of the head and neck. Head Neck 21: 728–733
Stoeckli SJ, Pfaltz M, Steinert H, Schmid S (2002) Histopathological features of occult metastasis detected by sentinel lymph node biopsy in oral and oropharyngeal squamous cell carcinoma. Laryngoscope 112: 111–115
Stoeckli SJ, Steinert H, Pfaltz M, Schmid S (2001) Sentinel lymph node evaluation in squamous cell carcinoma of the head and neck. Otolaryngol Head Neck Surg 125: 221–226
Tennvall J, Biorklund A, Moller T, Ranstam J, Akerman M (1998) Is the EORTC prognosis index of thyroid cancer valid in differentiated thyroid carcinoma?: a retrospective multivariate analysis of differentiated thyroid carcinoma with long follow-up. Cancer 57: 1405–1414
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stoeckli, S.J., Pfaltz, M., Steinert, H. et al. Sentinel lymph node biopsy in thyroid tumors: a pilot study. Eur Arch Otorhinolaryngol 260, 364–368 (2003). https://doi.org/10.1007/s00405-003-0594-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-003-0594-y