Abstract
Objective
To evaluate the safety in the first 12 h, efficacy and maternal satisfaction of a double balloon catheter (DBC) with vaginal prostaglandin (PGE) for induction of labour (IOL).
Methods
We conducted a multicentre randomised controlled study of 420 patients from 1st January 2016 to 31st December 2017 to evaluate the use of DBC in IOL in an Asian population looking at the adverse effects in the first 12 h after insertion. Women were assigned randomly to cervical ripening with either a DBC or a prostaglandin pessary. The adverse events in the 12 h after DBC or first prostaglandin inserted, the efficacy of a DBC to a prostaglandin in labour induction and maternal satisfaction were evaluated.
Results
There were significantly less women with uterine hyperstimulation in the DBC (2 vs 24, p ≤ 0.0001) compared to the prostaglandin group. There were no women with uterine hyperstimulation and non-reassuring foetal status in the DBC while there were 5 women with uterine hyperstimulation and foetal distress in the prostaglandin group. Use of entonox was significantly less in the DBC group (p = 0.009). There were no significant differences in both groups in caesarean section, vaginal deliveries and time to delivery, although significant less time was needed to achieve cervical os dilation more than 4 cm in the DBC group (p ≤ 0.0001). Neonatal birth outcomes were similar. Women’s pain scores were similar for both methods. 80.1% of women allocated the DBC and 76.8% of women allocated the PGE were keen to recommend their method of induction.
Conclusion
Double balloon catheter remains a good alternative method for inducing women in view of a good safety profile with low risk of hyperstimulation and high maternal satisfaction.
Clinical trial registration
ClinicalTrials.gov Identifier: NCT02620215.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In light of recent evidence in the literature showing benefits for elective induction of uncomplicated singleton pregnancies at 39 weeks of gestation, [1] we can expect that induction of labour (IOL), which is one of the most common procedures a woman may experience in pregnancy, will become even more frequently employed. As such, there is a pressing need to study the most optimal method of cervical ripening among pharmacological, mechanical or surgical methods.
There are increasing amounts of evidence of safety and efficacy of mechanical IOL including an updated publication of the Cochrane Database of Systematic Reviews in 2019 [2] and a NICE interventional procedure guidance on the double balloon catheter (DBC). [3] A well-conducted meta-analysis by Du et al. published in 2016 [4] demonstrated that mechanical IOL with cervical ripening balloons appeared to have similar efficacy profiles, greater safety and cost-effectiveness than prostaglandin (PGE) agents. A randomised controlled study on 98 women in 2018 specifically addressing patient experience between IOL methods found that pain during induction was significantly lower with the double balloon cervical ripening balloon while other satisfaction and acceptability scores were similar. [5, 6] Learning curve for the insertion of the DBC is short. [7]
To the best of our knowledge, current large randomised controlled trials have not directly examined the immediate effects or potential adverse events that occur in the first 12 h of double balloon catheter or first prostaglandin insertion in IOL. [8,9,10,11] Outcomes on the efficacy and safety during this period will be valuable to support its clinical application in high-risk pregnancies and fulfil a current void in offering safer outpatient induction. Existing Cochrane review [2] identified gaps in safety aspects for the neonate and maternal satisfaction. We conducted a multicentre study to specifically evaluate the use of DBC in IOL in a Southeast-Asian population with regards to adverse effects in 12 h after insertion while using a non-incremental balloon-filling regime, neonatal safety and maternal satisfaction.
Materials and methods
This is a prospective cohort randomised controlled study conducted at 2 tertiary hospitals each with an approximate 11,000 deliveries annually. The study was conducted from 1st January 2016 to 31st December 2017. Local institutional review board approval was achieved in both centers. 210 women were recruited in each center.
The main hypothesis is DBC that has no major adverse events including hyperstimulation and non-reassuring foetal status in a 12-h period after DBC insertion, and its efficacy is non-inferior to prostaglandin insertion. We attempt to address this hypothesis by monitoring the periods of regular uterine contractions (> 1:10) measuring the frequency, length of contractions and its association with adverse events during this period after intervention. We also examined the efficiency of DBC in achieving a favourable cervix i.e. cervical os dilated to at least 3 cm, which allowed rupture of membranes at the end of 12 h compared with PGE. Women were interviewed after the delivery, using a number scale from 1 to 10 for pre- and post- induction pain score and number scale 1–5 to rate their satisfaction on the method used for IOL. They were also asked if they would recommend it to other women and their preference for outpatient IOL.
NICE guidelines on induction of labour [12] defined uterine hyperstimulation as contractions more than 5 in 10 min for more than 20 min or contractions lasting more than 2 min in duration. A retrospective study involving prostaglandin induction of labour [13] showed that hyperstimulation occurred in 5.8% of cases. Arbitrarily, we considered a relative 80% decrease in hyperstimulation risk (estimated hyperstimulation with DBC 1%) as clinically significant. Hence, assuming a significance level of 5% and power of 80%, and allowing for a 5% dropout rate, we estimated that 210 subjects would be needed per group (one-sided test).
Written informed consent was obtained after the women had consented to IOL, this occurred either in antenatal outpatient clinics, labour ward triage or antenatal wards. Randomisation of the women was then achieved with third party sealed envelope allocation. 210 envelopes containing DBC allocation and another 210 identical envelopes containing prostaglandin pessary allocation were prepared by a third party. The 420 envelopes were shuffled according to a computer randomisation code after sealing and labelled with a randomisation allocation number from 1 to 420. Half of the envelopes were handed to the each center’s principal investigator, and kept locked in the clinical store on labour ward together with the stock of DBC and prostaglandin pessary.
Women requiring term IOL were identified in both centers and screened. Pregnant women aged from 21 to 40 years old, with a singleton pregnancy and no major foetal anomaly who were suitable for vaginal delivery and scheduled for a planned IOL from 37+0 to 41+6 weeks gestation were included into the study. Women with spontaneous labour at start of planned induction, bishop score more than 6 and cervical dilation more than or equal to 3 cm at the start of induction or with confirmed rupture of membranes were excluded. Women with abnormal cardiotocograph at the start of induction, with any indication for caesarean delivery or a previous scarred uterus were also excluded. Once the written informed consent was obtained a research assistant would disclose the intervention allocation.
In the group allocated the DBC, the catheter (Cook cervical ripening balloon) was inserted into the cervical canal either under direct visualisation with a sterile speculum examination or via vaginal examination. After both balloons have entered the cervical canal, the uterine balloon was filled with 40 ml of saline, the catheter was then retracted and a vaginal examination is done to ensure the DBC is in the cervical canal and the vaginal balloon is inflated to 40 ml of saline. Both balloons were then inflated to 80 ml each. The tubing was then taped to the woman’s thigh. After the DBC was put in place, a cardiotocogram was performed for 60–120 min and the woman was allowed to ambulate. The double balloon catheter was left in place for a maximum of 12 h as per the manufacturer’s advice. Failed induction of labour was defined when labour was not initiated after removal of the DBC.
In the group allocated the vaginal prostaglandin pessary, the 3 mg dinoprostone pessary (Prostin) was inserted and placed in the posterior vaginal fornix. After insertion of the pessary, a cardiotocogram was performed for 60–120 min and the woman was allowed to ambulate. After 6 h, if the woman is not in labour and the bishop score was still less than 6, a second dose of prostaglandin was inserted and monitored as previously described. Failed induction of labour was defined when labour was not initiated after insertion of 2 pessaries.
The women were continuously monitored for uterine activity and non-reassuring foetal status. During the first 12 h of the intervention, women were monitored for hyperstimulation defined when there was more than 5 contractions for 10 min and hypertonus defined as a single contraction lasting for more than 2 min. The type of pain relief use was recorded (entonox, intramuscular pethidine or epidural). Any vaginal bleeding that was more than a “show” was recorded. Features of any non-reassuring heart rate was recorded and this was defined in accordance to the NICE intrapartum care guidelines [14]. Decisions for caesarean section based on cardiotocographs were made by obstetrician consultants on labour ward.
After the DBC was removed or expelled, and if vaginal examination revealed that the cervical os was more than 3 cm, membranes were ruptured and oxytocin infusion was started for women who were not in labour. For the prostaglandin group, during a vaginal examination, if the cervical os was more than 3 cm, membranes were ruptured and oxytocin infusion started 6 h after the last dose of prostaglandin. Oxytocin was administered using a standard regime in each hospital. Once in active labour, standardised intrapartum care was given according to hospital protocol.
All decisions for caesarean sections were made by obstetrician consultants on labour ward. Women who failed to prime the cervix with the randomised induction method were counselled by obstetrician consultants for further prostaglandin insertion or a caesarean section. Failure to progress in first stage of labour was defined as the absence of cervical change for 4 h or more in the presence of adequate uterine contractions and cervical dilation of at least 4 cm. During second stage of labour women who were undelivered with no progress with active pushing after at least 2 h in multiparous women and 3 h in nulliparous women were diagnosed as failure to progress.
Statistical analysis of outcomes data was performed with chi-squared test and R software.
Results
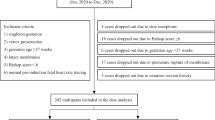
During the study period, 420 patients were recruited, 210 from each center. (Fig. 1. Study Enrolment flowchart).
In the DBC group, 3 women were excluded because of age criteria and deviation from study protocol. One patient was excluded because of prelabour rupture of membranes after randomisation and before the DBC was inserted and 4 patients had incomplete data. During labour, 5 patients had malpresentation and had to undergo a caesarean section, these patients were excluded from the analysis. In the prostaglandin group, 4 patients were excluded because of age criteria and deviation from study protocol, 4 patients were dilated to more than 3 cm after the randomisation and before the insertion of the vaginal prostaglandin and excluded. One patient was not induced as she declined induction of labour after the randomisation. During labour, 3 patients had malpresentation and had to undergo a caesarean section, they were also excluded from the analysis. The demographics and baseline characteristics were similar in both groups (Table 1). Indications for induction of labour were not significantly different in both groups.
The use of entonox is significantly more in the prostaglandin group than the DBC group, while the use of intramuscular pethidine and epidural was similar in both groups (Table 2). Although there was a shorter interval for requiring pain relief in the DBC group (7.60 ± 2.72, n = 55) versus (6.57 ± 2.83, n = 75) hours in the prostaglandin group, there were less women in the DBC group who needed pain relief. In the DBC group, 141 patients (71.9%) did not need pain relief during the first 12 h of induction.
Adverse events during the first 12 h of induction were recorded (Table 3). All patients who had hyperstimulation had intrauterine resuscitation with a change to left lateral position and intravenous hydration. Three patients needed tocolysis with intravenous terbutaline, none required delivery due to persistent non-reassuring foetal status. There were two cases of hyperstimulation occurred in the DBC arm, but none had an impact on the foetal status. There were no incidences of intrauterine deaths in both groups.
Ten women in the DBC group still required prostaglandin while 28 women in the PGE group needed more prostaglandins to prime the cervix after the initial 12 h. The outcomes of both groups were analysed with the intention to treat. There was no difference in the time to delivery in both groups (22.42 h ± 8.84 vs. 23.78 h ± 13.4); however, the time for dilation to 4 cm was significantly less in the DBC group than the vaginal prostaglandin group (13.87 ± 7.51 vs. 19.08 ± 10.59, p < 0.0001), as demonstrated in the Kaplan–Meier survival curves (Fig. 2.). In the DBC group, oxytocin use for labour was significantly higher (152 vs. 109, p < 0.0001). 52 patients in the prostaglandin group, underwent spontaneous rupture of membranes (p < 0.0001) while the rest had artificial rupture of membranes. There were no significant differences in the mode of delivery in both groups (Table 4). A significant number of women in the prostaglandin group had a caesarean section because of failed IOL (3 vs. 12, p = 0.0369), while a significant number of patients who had the DBC allocation had a caesarean for failure to progress in the first stage of labour (41 vs. 16, p = 0.0160).
Neonatal outcomes were similar in both study groups. The average birthweight of the babies in the DBC group was 3058.88 g ± 447.74, while the PGE group was 3069.94 g ± 467.13, p = 0.4053. One baby in the PGE group had an Apgar score of less than 7 at 5 min, none in the DBC group. Both groups had 4 babies who had neonatal intensive care admission.
The average pain scores at the start of IOL and during the process of IOL were similar. Both groups expressed good satisfaction scores (DBC 3.64 ± 1.0 vs. PGE 3.30 ± 1.2, p = 0.9960), and the majority of the women said they would recommend their method of IOL (DBC 80.1% vs. PGE 76.8%, p = 0.2720). Minority of women were keen for the option of having outpatient induction (DBC 14.8% vs. PGE 10.6%).
Discussion
This study was undertaken to evaluate the safety of the DBC as well as the efficacy of the DBC compared to the vaginal prostaglandin. Use of prostaglandin in the induction of labour [13] showed that hyperstimulation occurred in 5.8% of cases. Our findings show that the number of adverse events in hyperstimulation and the use of entonox were significantly less in the women allocated to the DBC group. These findings are similar to Du et al. [4] who also showed a 10 times lower risk of hyperstimulation in the double balloon catheter group to the prostaglandin group. However, the time to first use of pain relief was significantly earlier in the PGE group compared to the DBC group, this may be explained as likely an inherent development in labour induction and the effect of the medication.
There was a significantly higher use of syntocinon in the DBC group (n = 152) vs the PGE group (n = 109), p < 0.0001. This has also been seen in several studies [4, 6]. This may be explained with the study protocol, the use of syntocinon is started 6 h after the insertion of prostaglandin while it can be started immediately after removal of DBC and rupture of membranes. Use of syntocinon can be a disadvantage as there are complications from its use. Hence the use DBC has to be weighed against using prostaglandin and its risk of hyperstimulation during cervical priming.
A recent systematic review [15] on the safety of the balloon catheter used a random effects model. It included 26 studies (8292 women) which estimated the prevalence of adverse events to be 0–0.26%, “pain and discomfort’ being most common. In this study, none of the included studies used a double balloon catheter. Our study provides more data to support the good safety profile of the double balloon catheter. Solt et al. [16] compared the Bishop score increment between a DBC and a single balloon catheter, he concluded that the DBC was more effective that the single balloon catheter with decreased time to delivery and decreased caesarean section rates. The usage of a single balloon catheter in induction of labour is off-licensed, and also requires traction.
Outpatient cervical ripening can be an attractive option because of the potential for lower costs and patient satisfaction. This is only possible if the method does not have an adverse effect on the foetus and does not require medical interventions. Less foetal monitoring may be required when DBC is used. In this regard, it may still be difficult for the double catheter balloon to fulfil this role fully, even without hyperstimulation, given the requirement for analgesia in the first 12 h in 28.1% of the patients. In our study, majority of women did not prefer outpatient induction as an option.
Our study aimed to fill the gap of knowledge as mentioned in the latest Cochrane review [2]. We showed that women are equally satisfied with the DBC compared to the prostaglandin for induction of labour. In addition to our study, another local study [5] also showed that the use of DBC showed similar satisfaction and acceptability in the Singapore population, with 71% of patients recommending the DBC as the mode for IOL. Although minority of our women preferred outpatient induction as an option, Wilkinson et al. [11] ran a pilot randomised trial comparing inpatient and outpatient balloon induction, they found that patients in the outpatient arm felt less isolated and emotionally alone, while medical staff including midwives and doctors were more comfortable with the use of a catheter as an option for outpatient ripening with 90% supporting outpatient ripening with the catheter.
Du et al.’s systemic review [4] of nine randomised controlled studies concluded similar efficacy profiles between the double balloon catheter and the prostaglandin E2. Our study also showed similar labour outcomes in both groups with regards to recourse to caesarean deliveries, but identified the difference in indications. Caesarean delivery for failed induction was more common in the prostaglandin group and failure to progress in the first stage of labour more common in the DBC group. Average time to eventual delivery in both groups was similar. Our study, in particular, demonstrated a more predictable course of induction and significantly shorter time required with the DBC from the initiation of IOL to achieving a cervical dilation of more than 4 cm (91.3% vs 67.6%, p ≤ 0.0001), although artificial rupture of membranes and syntocinon are more frequently required. There were more failed cervical priming in the PGE group (28 vs 12). We believe this could offer significant advantage to the average busy obstetricians in planning inductions for their patients, as well as better patient satisfaction. A cost-efficacy study may be useful in evaluating a best method of induction.
Currently, there are nine randomised controlled trials [9, 17,18,19,20,21,22] involving a double balloon catheter. The balloon-filling regime is not standardised. In this trial, we used a standardised non-incremental balloon-filling regime prescribed according to the manufacturer’s advice. This decreased delays in achieving full inflation and decreased the time requiring intensive monitoring of the foetus; hence, we would recommend this as the standard balloon-filling regime for the double balloon catheter.
A limitation of the study was that it was impossible to blind the allocation to the investigator or the patient. However, the investigator had no part in observing any adverse events. The CTGs were interpreted and the need for intervention determined by the attending clinicians who although were not possible to blind, had no interest in the study. Hyperstimulation was specifically defined and recorded by a third party studying the CTGs and blinded to the patient’s allocated group. The patient also reported contractions intervals, pain scores, satisfaction scores with validated standard pain and satisfaction assessment tools to minimise potential bias. Allocations were omitted from the database so as to blind the analyst.
Conclusion
Our study shows low-uterine hyperstimulation and a good safety profile of the double balloon catheter in the induction of labour, with a more predictable and shorter course of induction. Women were equally satisfied after DBC and prostaglandin induction. DBC may have a place in high-risk pregnancies such as growth-restricted foetuses.
Availability of data and material
Data available on request from the authors.
References
Grobman WA, Rice MM, Reddy UM, Tita AT, Silver RM, Mallet G et al. (2018) Labor induction versus expectant management for low-risk nulliparous women. New Engl J Med
De Vaan MDT, ten Eikelder MLG, Jozwiak M, Palmer KR, Davies-Tuck M, Bloemenkamp KWM, Mol BWJ Boulvain M (2019) Mechanical methods for induction of labour. Cochrane Database Syst Rev 10.
National Institute for Health and Clinical Excellence (NICE) (2015) Insertion of a double balloon catheter for induction of labour in pregnant women without previous caesarean section: Interventional procedures guidance. National Institute for Clinical Excellence, London
Du YM, Zhu LY, Cui LN, Jin BH, Ou JL (2016) Double-balloon catheter versus prostaglandin E2 for cervical ripening and labour induction: a systematic review and meta-analysis of randomised controlled trials. BJOG. https://doi.org/10.1111/1471-0528.14256. Epub 2016 Aug 17
Lim SE, Tan TL, Ng GYH, Tagore S, Kyaw EEP, Yeo GSH (2018) Patient satisfaction with the cervical ripening balloon as a method for induction of labour: a randomised controlled trial. Singapore Med J 59(8):419–424
Tan TL, Ng GYH, Lim S, Tagore S, Kyaw E, Yeo G (2015) Cervical ripening balloon as an alternative for induction of labour: a randomised controlled trial. BJMP 8(1):a806.
Ng GYH, Tan TL, SE Lim, S Tagore, Yeo GSH (2017) Learning curve in the use of cervical ripening balloon for induction of labour. Singapore J Obstet Gynaecol 48(1):15–19
Løkkegaard E, Lundstrøm M, Kjær MM, Christensen IJ, Pedersen HB, Nyholm H (2015) Prospective multi-centre randomised trial comparing induction of labour with a double-balloon catheter versus dinoprostone. J Obstet Gynaecol. 18:1–6.
Wilkinson C, Bryce R, Adelson P, Turnbull D (2015) A randomised controlled trial of outpatient compared with inpatient cervical ripening with prostaglandin E2 (OPRA study). BJOG 122(1):94–104
Howard K, Gerard K, Adelson P, Bryce R, Wilkinson C, Turnbull D (2014) Women’s preferences for inpatient and outpatient priming for labour induction: a discrete choice experiment. BMC Health Serv Res 30(14):330
Wilkinson C, Bryce R, Adelson P, Turnbull D (2015) A comparison of inpatient and outpatient balloon catheter cervical ripening pilot randomised controlled trial. BMC 15:126
National Institute for Health and Clinical Excellence (NICE) (2008) Induction of labor: clinical guideline no. 70. National Institute for Clinical Excellence, London
Egarter CH, Husslein PW, Rayburn WF (1990) Uterine hyperstimulation after low-dose prostaglandin E2 therapy: tocolytic treatment in 181 cases. ACOG 163(3):794–879
National Institute for Health and Clinical Excellence (NICE) (2014) Intrapartum care for healthy women and babies: clinical guideline no. 190. National Institute for Clinical Excellence, London
Diederen M, Gommers J, Wilkinson C, Turnbull D, Mol B (2018) Safety of the balloon catheter for cervical ripening in outpatient care: complications during the period from insertion to expulsion of a balloon catheter in the process of labour induction: a systematic review. BJOG 125(9):1086–1095
Solt I, Wolf MF, Ben-Haroush S, Kaminskyi S, Ophir E, Bornstein J (2019) Foley catheter versus cervical double balloon for labor induction: a prospective randomized study. J Matern Fetal Neonatal Med 11:1–8
Salim R, Zafran N, Nachum Z, Garmi G, Kraiem N, Shalev E (2011) Single-balloon compared with double balloon catheters for induction of labor: a randomized controlled trial. Obstet Gynecol 118(1):79–86
Mei-Dan E, Walfisch A, Suarez-Easton S, Hallak M (2012) Comparison of two mechanical devices for cervical ripening: a prospective quasi-randomized trial. J Matern Fetal Neonatal Med 25(6):723–727
Pennell C, Henderson J, O’Neill M, McCleery S, Doherty D (2009) Induction of labour in nulliparous women with an unfavourable cervix: a randomised controlled trial comparing double and single balloon catheters and PGE2 gel. BJOG 116:1443–1452
Kehl S, Ziegler J, Schleussner E, Tuschy B, Berlit S, Kirscht J et al (2015) Sequential use of double-balloon catheter and oral misoprostol versus oral misoprostol alone for induction of labour at term (CRBplus trial): a multicentre, open-label randomised controlled trial. BJOG 122(1):129–136
Cromi A, Ghezzi F, Uccella S, Agosti M, Serati M, Marchitelli G et al (2012) A randomized trial of preinduction cervical ripening: dinoprostone vaginal insert versus double-balloon catheter. ACOG 207:125–127
Atad J, Hallak M, Auslender R, Porat-Packer T, Zarfati D, Abramovici H (1996) A randomized comparison of prostaglandin E2, oxytocin, and the double-balloon device in inducing labor. Obstet Gynecol 87:223–227
Acknowledgements
We would like to thank all the participants of the trial and KK Women and Children’s Hospital and UMC hospital labour ward staff providing assistance in data collection. We will like to thank Dr. Janice Tung for her input to the study.
Funding
Funding for the study was supported by SingHealth Duke-NUS OBGYN Academic Clinical Program (ACP) Grant.
Author information
Authors and Affiliations
Contributions
YHGN Project development, recruitment of participants, data collection manuscript writing and editing. AAA: Recruitment and data collection and manuscript editing. TLT: Project development, manuscript editing. R: Project development, manuscript editing. ST: Project development, manuscript editing. GSHY: Project development, manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest declared.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Grace Ng, Y.H., Aminuddin, A.A., Tan, T.L. et al. Multicentre randomised controlled trial comparing the safety in the first 12 h, efficacy and maternal satisfaction of a double balloon catheter and prostaglandin pessary for induction of labour. Arch Gynecol Obstet 305, 11–18 (2022). https://doi.org/10.1007/s00404-021-06090-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-021-06090-y