Abstract
Background
According to the theory of fetal-derived adult diseases, abnormal fetal development might affect the occurrence of diseases in adulthood, and appropriate fetal growth status intrauterine might have a beneficial effect on it. To adapt properly for fetal development, there are numerous changes in the maternal physiology during pregnancy, including blood lipid metabolism. The aim of this study is to evaluate the association between lipid profiles in the second and third trimesters of normal pregnancy and fetal birth weight.
Materials and methods
The study population was derived from 5695 pregnant women, who maintained routine prenatal care at the women’s hospital of Zhejiang University, School of medicine January 1, 2014, and December 31, 2014. The pregnant women in this study all carried uncomplicated singleton pregnancies to at least 37 weeks.
Results
The mean (standard deviation) birth weight was 3361.00 (385.94) g; 413 (7.3%) of the infants were large for gestational age, and 330 (5.8%) were macrosomia. On multiple linear regression analysis, positive determinants of birth weight were gravidity, parity, gestational age at delivery, male infant, maternal height, and weight before pregnancy, weight gain during pregnancy, fasting blood glucose (FBG) level, second-trimester cholesterol (TC) and third-trimester triglyceride (TG), gestational albumin (ALB), and third-trimester high-density lipoprotein (HDL-C) levels were each negatively associated with birth weight. On logistic regression analysis, the significant metabolic lipid predictors of delivering a large-for-gestational-age infant were second- and third-trimester TG (aOR = 1.178, 95% CI 1.032–1.344, p = 0.015; aOR = 1.106, 95% CI 1.043–1.173, p = 0.001, respectively) and second- and third-trimester HDL-C level (aOR = 0.655, 95% CI 0.491–0.874, p = 0.004; aOR = 0.505, 95% CI 0.391–0.651, p < 0.001, respectively). Third-trimester TG and HDL-C were stable predictors of large-for-gestational-age infants in stratification analysis. High TG and low HDL-C level during third trimester could be considered as indicators of a high risk of large for gestational age (LGA) and macrosomia, regardless of infant gender.
Conclusion
These results suggest that future lifestyle programs in women of reproductive age with a focus on lowering TG levels (i.e., diet, weight reduction, and physical activity) may help to reduce the incidence of LGA and macrosomia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the theory of fetal-derived adult diseases [1], abnormal fetal development might affect the occurrence of diseases in adulthood, and appropriate fetal growth status intrauterine might have a beneficial effect on it. To adapt properly for fetal development, there are numerous changes in the maternal physiology during pregnancy, including blood lipid metabolism [2]. Maternal serum lipid may play an important role in fetal growth, and the levels begin to increase during the 9th–13th week of pregnancy, and gradually continue rising as the pregnancy progresses. Maternal serum lipid concentrations peak during 31–36 weeks of gestation, decrease markedly over 24 h after delivery, and return to pre-pregnancy levels in 4–6 weeks after birth [3].
Some studies have shown that altered lipid metabolism during pregnancy results in increased levels of TC, TG, and LDL-C, and decreased levels of HDL-C [4]. These lipid profiles seen in pregnancy might be due to the increased absorption of lipids in the gastrointestinal tract [5]. TG and TC concentrations markedly increase due to two factors: increased hepatic lipase activity, leading to enhanced hepatic triglyceride synthesis; and reduced lipoprotein lipase activity, resulting in decreased catabolism of adipose tissue [6].
Hyperlipidemia has numerous effects on the intrauterine environment, and can have a significant impact in fetal development [7]. For example, elevated TG concentrations provide additional fetal glucose, and elevated LDL-C levels exert an effect on placental steroidogenesis. These metabolic changes represent adaptations to maternal–fetal physiology during pregnancy.
Several studies have reported the association between maternal TG and fetal birth weight [8, 9]. Pregnant women with higher levels of TG and LDL-C, along with lower levels of HDL-C have been to be associated with an elevated risk for macrosomia and large-for-gestational-age (LGA) neonates [10, 11]. Elevated maternal TG levels lead to excessive fetal growth and ultimately macrosomia. In addition, previous studies have suggested that elevated lipid levels in pregnancy could be significantly associated with a higher risk of gestational diabetes mellitus (GDM) and pre-eclampsia (PE) in the mother [12]. Some studies have suggested that low TG levels in early pregnancy are protective against GDM and LGA, and that low LDL-C levels were protective against preterm birth. Additionally, elevated TG levels were related to an increased risk of PE, while elevated LDL-C levels were a risk factor for macrosomia [13]. It has been reported that the concentrations of TG in mothers with GDM are positively associated to fetal birth weight, neonatal body mass index, and fat mass. Furthermore, these overweight offspring may carry an increased risk of obesity and type 2 diabetes mellitus later in life [14].
Proper maternal lipid profiles may provide suitable condition for fetal development. Rare studies had studied the relationship between maternal lipid levels of different trimester and fetal birth weight in normal pregnancy. The aim of our study is to shed more light on the alteration of lipid profiles in second and third trimester, and to analyze the relationship between maternal lipid levels and perinatal outcomes (LGA and macrosomia).
Methods
Study population
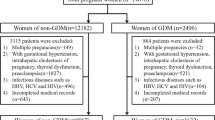
Between 1 Jan 2014 and 31 Dec 2014, pregnant women who attended regular prenatal health care and would be given birth in Women’s Hospital, Zhejiang University School of Medicine were invited to participate in the study. Before enrollment, approval of the study was obtained from the hospital’s Clinical Research Ethics Committee (the reference number: 20170160) and written informed consent was signed by every participant. We established the study cohort based on inclusion and exclusion criteria. Inclusion criteria of pregnant women were: (1) maternal age at delivery between 19 and 44 years; (2) had integrated medical records; and (3) singleton pregnancy. Exclusion criteria of pregnant women were: (1) had malignant tumor, diabetes mellitus, chromosomal abnormalities, and inherited metabolic diseases before pregnancy; (2) experienced serious infection during early pregnancy; (3) used tobacco, consumed alcohol, or drugs that affect blood lipid metabolism during pregnancy; and (4) pregnancy complications such as GDM, PE, and intrahepatic cholestasis of pregnancy (ICP).
All the women included were requested to complete a general medical record about sociodemographic characteristics, including maternal age, gravidity, parity, height, pre-pregnancy weight, and other important information. Gestational age was calculated based on the last menstrual period and was confirmed by an ultrasonographic examination performed before 20 weeks of gestation. Fasting blood glucose (FBG) and lipid concentrations upon entry into the study were assessed and pregnancy complications (GDM, PE, ICP, etc.) were collected from medical records during gestation. Information on maternal weight before delivery, delivery mode, gestational age, newborn sex, birth weight, Apgar scores, and perinatal outcomes were recorded by midwives or obstetricians upon delivery and retrieved from medical records after delivery. Inclusion criteria for newborns were singleton and 5-min postpartum Apgar scores ≥ 7. Exclusion criteria for newborns were preterm births (before 37 completed weeks) or expired delivery (more than 41 completed weeks), chromosomal abnormalities, inherited metabolic diseases, and congenital abnormalities. In total, 5695 pairs of mothers and neonates were included in our study.
Biochemical analyses
Venous blood samples for lipid assessment were taken after overnight fasting from all the participants at the second (24–26 gestational weeks) and third (30–32 gestational weeks) trimester of pregnancy. Every sample was assayed for TC, TG, HDL-C, and LDL-C concentrations. TC and TG were assayed with the cholesterol oxidase-phenol aminophenazone method, and glycerol-3-phosphatase oxidase-phenol aminophenazone method, respectively. HDL-C and LDL-C were measured by homogeneous enzymatic colorimetric assays. All the lipid measurements were performed on an automatic biochemical analyser (Abbott Architect C16000, Abbott Laboratories, USA), respectively, with TC, TG, HDL-C, and LDL-C detection kits (Abbott Diagnostic Kit, Abbott Laboratories, USA).
Definitions
BMI was calculated by dividing weight in kilograms by the square of height in meters. Maternal pre-pregnancy BMI was calculated from pre-pregnancy height and weight, and categorized into underweight (< 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥ 30.0 kg/m2) groups on the basis of World Health Organization BMI classification [15]. Gestational weight gain (GWG) was calculated as pre-pregnancy weight subtracted from the measured weight recorded at the last prenatal visit before delivery. According to the new recommendations from American Institute of Medicine, GWG was stratified into appropriate, inadequate, and excessive groups [16]. Based on different pre-pregnancy BMIs, appropriate GWG was defined as 12.5–18.0 kg in underweight women, 11.5–16.0 kg in normal-weight women, 7.0–11.5 kg in overweight women, and 5.0–9.0 kg in obese women. Falling below the thresholds was defined as inadequate GWG, while exceeding the thresholds was defined as excessive GWG.
The World Health Organization (WHO) defined anemia during pregnancy as a hemoglobin concentration below 110 g/L at any time point in the pregnancy [17]. Newborns were classified into appropriate for gestational age (AGA), small for gestational age (SGA), and large for gestational age (LGA) on the basis of Neonatal Birth Weight for Gestational Age and Percentile in 23 Cities of China [18]. Infants with birth weight above 90th percentile for gestational age were classified as LGA, and SGA was defined as the lowest 10th percentile; those having weight between 10 and 90th percentile were AGA. According to the birth weight, neonates could be stratified into low birth weight (< 2500 g), normal birth weight (2500 to < 4000 g), and macrosomia (≥ 4000 g) groups.
Statistical analysis
The data on continuous variables with normal distribution were presented as mean ± SD, and median with inter-quartile range for variables not normally distributed. Categorical data were shown as counts and percentages. Characteristics between LGA group and AGA group were compared using one-way ANOVA (for continuous variables) or Chi-square test (for categorical variables). Serum TC, TG, LDL-C, and HDL-C concentrations at the second and third trimesters between LGA group and AGA group were compared using Mann–Whitney test. Maternal lipid (TC, TG, LDL-C, and HDL-C) increases from the second to third trimester were compared using Wilcoxon matched-pairs signed-rank test. The relationships between lipids (continuous) in pregnancy and fetal birth weight were estimated by linear regression models. Logistic regression analysis was applied to explore the associations between maternal dyslipidemia and perinatal outcomes (LGA, macrosomia, SGA, and LBW). In the multivariable adjusted model, maternal age, marriage status, race, gravidity, parity, gestational age at birth, infant gender, height, pre-pregnancy weight, gestational weight gain, anemia, FBG, and ALB levels were regarded as confounding variables. All the analyses were performed with R version 3.4.3 for Windows (The R Project; http://www.r-project.org). p values < 0.05 were defined as statistically significant.
Results
Characteristics of the study sample
The process of inclusion and exclusion is shown in Supplementary Fig. S1, and the maternal and neonatal characteristics of our study population are shown in Table 1. According to the Institute of Medicine (IOM) recommendations for gestational weight gain, 53.9% met, 18.7% fell below, and 27.4% exceeded the criteria. The newborns in our study had a mean (SD) birth weight of 3361.00 (385.94) g. 87.1% of them were AGA, 7.3% were LGA and 5.8% were macrosomia. The mean (SD) gestational age at birth was 39.69 (1.05) weeks. In addition, 2925 (51.4%) infants were boys.
Maternal factors associated with infant birth weight
The unadjusted associations between maternal and fetal factors and birth weight are shown in Table 2. Maternal age at delivery, gravidity, parity, gestational age at delivery, male infant, maternal height and weight before pregnancy, weight gain during pregnancy, FBG level, second-trimester TG and LDL-C, and third-trimester TG were all associated with higher birth weight. After adjustment for covariates, positive determinants of birth weight were gravidity, parity, gestational age at delivery, male infant, maternal height and weight before pregnancy, weight gain during pregnancy, FBG level, second-trimester TC, and third-trimester TG. Gestational ALB and third-trimester HDL-C were each negatively associated with birth weight. This model explained 30.2% of the variance in birth weight.
Comparison of maternal and neonatal characteristics across LGA and AGA group
Table 3 shows maternal and neonatal characteristics of our study population across LGA and AGA group. Compared to AGA group, maternal age at delivery, maternal height, pre-pregnancy weight, gestational weight gain, gravidity, parity, gestational ALB/FBG levels, gestational age at birth, and infant sex is significantly different in LGA group.
Table 4 shows maternal lipid profile by trimester. TG in the second and third trimester is higher in LGA group, while HDL-C in the second and third trimester is lower in LGA group. In addition, in LGA and AGA groups, Serum TC, TG, and LDL-C levels were increased in the third trimester compared to the second trimester, while HDL-C decreased as pregnancy advanced (p < 0.001), the same scenery was discovered in AGA group. (Supplementary Table S2). Supplementary Table S1 shows maternal lipid profile in percentiles by trimester.
Associations between maternal lipid profile and perinatal outcomes (LGA and macrosomia)
Tables 5, 6 display the associations between maternal second- and third-trimester lipid profile and LGA. In our study, the incidence of LGA was 7.3%. Table 5 shows that there was positive association between second- and third-trimester TG and LGA, negative association between second- and third-trimester HDL-C, third-trimester LDL-C and LGA, and no significant association between second- and third-trimester TC and LGA. However, Table 6 reports different associations between maternal lipids levels and LGA. Multivariate analysis discovered that adjusted for maternal age, gravidity, parity, maternal height, weight before pregnancy, gestational weight gain, infant gender, anemia, ALB and FBG, and second- and third-trimester TG level was associated with an increased risk for LGA (aOR = 1.178, 95% CI 1.032–1.344, p = 0.015; aOR = 1.106, 95% CI 1.043–1.173, p = 0.001, respectively), while second- and third-trimester HDL-C level was associated with a decreased risk for LGA (aOR = 0.655, 95% CI 0.491–0.874, p = 0.004; aOR = 0.505, 95% CI 0.391–0.651, p < 0.001, respectively) (Fig. 1, top panel). In contrast, there were no significant associations between second- and third-trimester TC and LDL-C levels and LGA in multivariate analysis.
Independent predictors of having a large-for-gestational-age or macrosomia infant among pregnancy women. An odds ratio greater than 1.00 is associated with an increased risk of having a large-for-gestational-age or macrosomia infant. Odds ratios for blood lipids were adjusted for maternal age, gravidity, parity, gestational age at birth, infant gender, maternal height, weight before pregnancy, gestational weight gain, anemia, ALB, and FBG. For example, the adjusted odds ratio for having a large-for-gestational-age infant increased by 1.178 per 1 mmol/L increase in TG during second trimester. aOR adjusted odds ratio, Tri. Trimester, CI confidence interval, TC total cholesterol, TG triglycerides, LDL-C/HDL-C low-density/high-density lipoprotein-cholesterol, LGA large for gestational age
Table S3 and Table S4 display the associations between maternal second- and third-trimester lipid profile and macrosomia. After adjustment for covariates, second- and third-trimester LDL-C level was associated with an increased risk for macrosomia (aOR = 1.093, 95% CI 1.033–1.155, p = 0.002; aOR = 1.271, 95% CI 1.009–1.601, p = 0.042; aOR = 1.224, 95% CI 1.064–1.409, p = 0.005, respectively), while second- and third-trimester HDL-C level was associated with a decreased risk for macrosomia (aOR = 0.551, 95% CI 0.394–0.772, p = 0.001; aOR = 0.432, 95% CI 0.322–0.580, p < 0.001, respectively) (Fig. 1, bottom panel).
Because pregnancy women delivered male infant were found to have a greater risk of gender-specific large-for-gestational-age infants compared with women delivered female infant, we repeated the logistic regression analysis stratified by infant gender (Table 7). In this analysis, third-trimester TG and HDL-C again emerged as significant predictors of large-for-gestational-age infants in both male and female infant layer; second- and third-trimester LDL-C level also reached significance in female infant layer. Stratification analysis were also conducted by different gestational weight gain (GWG) and different pre-pregnancy BMIs (Supplementary Table S5 and S6). In adequate and appropriate GWG layers, second- and third-trimester TG again emerged as significant predictors of large-for-gestational-age infants, while in excessive GWG layer, second- and third-trimester HDL-C were the protective predictors. Across different pre-pregnancy BMI layers, third-trimester HDL-C was the stable protective factor.
The stratified analyses identified the same independent predictors (third-trimester TG and HDL-C) on multiple linear regression and logistic regression as those in Table 2 and Fig. 1, respectively.
Finally, we got the results that the significant metabolic lipid predictors of delivering a large-for-gestational-age infant were second- and third-trimester TG and HDL-C level. Third-trimester TG and HDL-C were stable predictors of large-for-gestational-age infants in stratification analysis. High TG and low HDL-C level during third trimester could be considered as indicators of a high-risk of large for gestational age (LGA) and macrosomia, regardless of infant gender.
Discussion
In our population-based study, we comprehensively explored the relationship of maternal fasting glucose and lipid concentrations with fetal birth weight in Chinese reproductive-age women without pregnancy complications. Gestational age at delivery, male infant, maternal height, weight before pregnancy, weight gain during pregnancy, FBG level, second-trimester TC, and third-trimester TG were directly associated with newborn size in our study. And gestational ALB and third-trimester HDL-C levels were each negatively associated with birth weight. Third-trimester TG and HDL-C were stable predictors of LGA infants in stratification analysis.
Our findings of maternal fasting glucose levels within a non-diabetic range and higher birth weight are consistent with previous report by the HAPO studies [19, 20]. Tessa’s study also reported that maternal glucose levels in late pregnancy are particularly important for neonatal fat accretion and that this association is not confounded or modified by maternal BMI [21]. During the last third of gestation, due to the demands of the placental-fetal unit and rapid depletion of glycogen stores, the mother switches to a catabolic state in which glucose is the predominant nutrient crossing the placenta and maternal adipose tissue lipolytic activity is enhanced [22]. This result was also supported by experiment that among pregnant women infused with glucose labeled with stable isotopes several hours before delivery, was shown that 95% of infant plasma glucose after birth was from maternal plasma [23]. Since our maternal fasting glucose levels were tested in the second trimester, we believed that this interaction began earlier.
Our study found that maternal TG levels in the second and third trimester were positively associated with fetal birth weight, especially the third-trimester TG was stable predictor of large-for-gestational-age infants. Previous studies also had shown a similar correlation between maternal TG levels and neonatal birth weight [8, 14]. These results suggested that TG had a prolonged influence on fetal growth. Misra et al. [24] assessed the relationship between maternal serum lipid levels and birth weight among 143 women-infant pairs from Michigan and reported TG levels were positively associated with birth weight, although only among normal-weight women. The Pune Maternal Nutrition Study [25] found that maternal glucose, total cholesterol, and TG levels at both 18 and 28 week gestation were associated with higher birth weight among a population of women with low pre-pregnancy BMI. Crume’s study reported that TG levels in late pregnancy were associated with birth weight, but were not independent of pre-pregnancy BMI [21].
Furthermore, maternal HDL-C levels in the second and third trimester were found to have an inverse relationship with neonatal birth weight, and third-trimester HDL-C was stable predictor of large-for-gestational-age infants. Consistent with our results, Misra et al. [24] also reported an inverse relationship between HDL-C levels and birth weight among overweight/obese women, but not normal-weight women. In a nested case–control study of risk factors associated with macrosomia in Oslo, Norway, Clausen et al. [26] found that HDL-C were associated with an increased risk of macrosomia. While Boghossian et al. [19] found that HDL-C was associated with reduced neonatal size, and that TC and TG may be associated with larger size, they concluded that using these lipids as biomarkers may not be clinically useful and is unlikely to change clinical decision-making.
The mechanism of how HDL-C concentrations linked to abnormal fetal birth weight has not yet been studied. The fundamental function of HDL-C is to remove cholesterol and other lipids from peripheral tissues [27]. In our study, the inverse correlation between HDL-C and triglycerides in the second and third trimester was observed which has been well demonstrated in the previous research [28]. This correlation in the first half of pregnancy (17–19 weeks) has also been reported by Clausen et al. [26] in a large cohort of non-diabetic women. Hence, it can be hypothesized that the effect of dyslipidemia on abnormal fetal growth, especially the stable effect of HDL-C and TG, continued throughout the whole pregnancy even before pregnancy. Early monitoring of lipid metabolism disorder might prevent the fetus from overgrowth of weight. However, the standard normal maternal lipid levels were difficult to establish and it still remained controversial over the world. Some studies have shown that altered lipid profiles in mothers are associated with adverse pregnancy outcomes, such as GDM, PE, spontaneous preterm delivery, ICP, LGA, and macrosomia [29,30,31], which made it hard to predict neonatal size only by lipid levels. We assume that lipid levels in pregnancy without any complications and chronic diseases giving birth to appropriate weight infants can be defined as normal range of maternal lipid levels. Lipid profiles in pregnant women with GDM should also be analyzed in future studies to enlarge the reference range of lipids levels because of the interaction of maternal glucose and lipids. And cesarean section rate might also be reduced in China since the controlling fetal weight by early intervention of maternal lipids levels.
However, the present study still exited some limitations. There is outlier in birth weight and missing values in lipid measurements. However, because of our large sample, we think that this would have minor influence on our results, although we cannot rule out some residual confounding. We were not able to adjust for physical activity during pregnancy or family history of gestational diabetes, two factors that could confound our results. Our study collected the serum in the second trimester (24th–26th gestational age) and third trimester (30th–32th gestational age), which was suggested to be better to collect the maternal lipids concentrations across the whole pregnancy and even before pregnancy. It is important to pay attention to the possible impact of pre-gestational lipid levels on lipid profiles during pregnancies, particularly in obese patients which were not explored in this study. Furthermore, umbilical blood lipid levels could be collected for further investigation into the mechanisms behind the associations discussed in our study. More underlying physiology and molecular mechanisms should be provided by further basic research to make the markers more credible.
References
Sakuyama H, Katoh M, Wakabayashi H, Zulli A, Kruzliak P, Uehara Y (2016) Influence of gestational salt restriction in fetal growth and in development of diseases in adulthood. J Biomed Sci 23:12. https://doi.org/10.1186/s12929-016-0233-8
Brizzi P, Tonolo G, Esposito F, Puddu L, Dessole S, Maioli M, Milia S (1999) Lipo-protein metabolism during normal pregnancy. Am J Obstet Gynecol 181(2):430
Saarelainen H, Laitinen T, Raitakari OT, Juonala M, Heiskanen N, Lyyra-Laitinen T, Viikari JS, Vanninen E, Heinonen S (2006) Pregnancy-related hyperlipidemia and endothelial function in healthy women. Circ J 70(6):768–772
Ryckman KK, Spracklen CN, Smith CJ, Robinson JG, Saftlas AF (2015) Maternal lipid levels during pregnancy and gestational diabetes: a systematic review and meta-analysis. BJOG 122(5):643–651
Mankuta D, Elami-Suzin M, Elhayani A, Vinker S (2010) Lipid profile in consecutive pregnancies. Lipids Health Dis 5(9):58
Herrera E (2000) Metabolism adaptations in pregnancy and their implications for the availability of substrates to the fetus. Eur J Cin Nutr 5(4):47–51
Olmos PR, Rigotti A, Busso D, Berkowitz L, Santos JL, Borzone GR, Poblete JA, Vera C, Belmar C, Goldenberg D, Samith B, Acosta AM, Escalona M, Niklitschek I, Mandiola JR, Mertens N (2014) Maternal hypertriglyceridemia: A link between maternal overweight-obesity and macrosomia in gestational diabetes. Obesity 22(10):2156–2163
Di Cianni G, Miccoli R, Volpe L, Lencioni C, Ghio A, Giovannitti MG, Cuccuru I, Pellegrini G, Chatzianagnostou K, Boldrini A, Del Prato S (2005) Maternal triglyceride levels and newborn weight in pregnant women with normal glucose tolerance. Diabet Med 22(1):21–25
Whyte K, Kelly H, O’ Dwyer V, Gibbs M, O’ Higgins A, Turner MJ (2013) Offspring birth weight and maternal fasting lipids in women screened for gestational diabetes mellitus (GDM). Eur J Obstet Gynecol Reprod Biol 170(1):67–70
Haugen AC, Schug TT, Collman G, Heindel JJ (2015) Evolution of DOHaD: the impact of environmental health sciences. J Dev Orig Health Dis 6(2):55–64
Fleming TP, Velazquez MA, Eckert JJ (2015) Embryos, DOHaD and David Barker. J Dev Orig Health Dis 6(5):377–383
Jin WY, Lin SL, Hou RL, Chen XY, Han T, Jin Y, Tang L, Zhu ZW, Zhao ZY (2016) Associations between maternal lipid profile and pregnancy complications and perinatal outcomes: a population-based study from China. BMC pregnancy and Childbirth 16(3):60–69
Wang C, Zhu W, Wei Y et al (2017) The associations between early pregnancy lipid profiles and pregnancy outcomes. J Perinatol 37(2):127–133. https://doi.org/10.1038/jp.2016.191
Herrera E, Ortega-Senovilla H (2010) Disturbances in lipid metabolism in diabetic pregnancy—are these the cause of the problem? Best Pract Res Clin Endocrinol Metab 24(4):515–525
Obesity: preventing and managing the global epidemic (2000) Report of a WHO consultation. World Health Organ Tech Rep Ser 894:i–253
Rasmussen KM, Yaktine AL, et al (2009) Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines. Weight Gain During Pregnancy: Reexamining the Guidelines. National Academies Press (US), Washington (DC)
WHO (2017) Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System. Geneva: World Health Organization. (WHO/NMH/NHD/MNM/11.1). http://www.who.int/vmnis/indicators/haemoglobin.pdf.
Li Z, Rong Z, Shulian Z et al (2015) Chinese neonatal birth weight curve for different gestational age. Chin J Pediatrics 53(2):97–103
HAPO Study Cooperative Research Group, Metzger BE, Lowe LP et al (2008) Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 358(19):1991–2002
HAPO Study Cooperative Research Group (2009) Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study: associations with neonatal anthropometrics. Diabetes 58(2):453–459
Crume TL, Shapiro AL, Brinton JT et al (2015) Maternal fuels and metabolic measures during pregnancy and neonatal body composition: the healthy start study. J Clin Endocrinol Metab 100(4):1672–1680
Herrera E (2000) Metabolic adaptations in pregnancy and their implications for the availability of substrates to the fetus. Eur J Clin Nutr 54(Suppl 1):S47–S51
Staat BC, Galan HL, Harwood JE et al (2012) Transplacental supply of mannose and inositol in uncomplicated pregnancies using stable isotopes. J Clin Endocrinol Metab 97(7):2497–2502
Misra VK, Trudeau S, Perni U (2011) Maternal serum lipids during pregnancy and infant birth weight: the influence of prepregnancy BMI. Obesity (Silver Spring) 19(7):1476–1481
Kulkarni SR, Kumaran K, Rao SR et al (2013) Maternal lipids are as important as glucose for fetal growth: findings from the Pune Maternal Nutrition Study. Diabetes Care 36(9):2706–2713
Clausen T, Burski TK, Øyen N, Godang K, Bollerslev J, Henriksen T (2005) Maternal anthropometric and metabolic factors in the first half of pregnancy and risk of neonatal macrosomia in term pregnancies. A prospective study. Eur J Endocrinol 153(6):887–894
Brown WV (2007) High-density lipoprotein and transport of cholesterol and triglyceride in blood. J Clin Lipidol 1(1):7–19
Patsch W, Sharrett AR, Sorlie PD, Davis CE, Brown SA (1992) The relation of high density lipoprotein cholesterol and its subfractions to apolipoprotein A-I and fasting triglycerides: the role of environmental factors. The Atherosclerosis Risk in Communities (ARIC) Study. Am J Epidemiol 136(5):546–557
Boghossian NS, Mendola P, Liu A, Robledo C, Yeung EH (2017) Maternal serum markers of lipid metabolism in relation to neonatal anthropometry. J Perinatol 37(6):629–635
Martineau MG, Raker C, Dixon PH et al (2015) The metabolic profile of intrahepatic cholestasis of pregnancy is associated with impaired glucose tolerance, dyslipidemia, and increased fetal growth. Diabetes Care 38(2):243–248
Moayeri M, Heida KY, Franx A, Spiering W, de Laat MW, Oudijk MA (2017) Maternal lipid profile and the relation with spontaneous preterm delivery: a systematic review. Arch Gynecol Obstet 295(2):313–323
Acknowledgements
The authors would like to thank Mr. Jing Guo for his contribution in data analysis.
Funding
None.
Author information
Authors and Affiliations
Contributions
FFX: project development, data collection, and manuscript writing; HQC: data analysis; QQC, DQC, and YC: data collection; MS and BHZ: manuscript revise; QL: protocol. All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by FX, HC, QC, DC, and YC. The first draft of the manuscript was written by FX and all authors commented on previous versions of the manuscript. The manuscript was revised by BZ and MS. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xi, F., Chen, H., Chen, Q. et al. Second-trimester and third-trimester maternal lipid profiles significantly correlated to LGA and macrosomia. Arch Gynecol Obstet 304, 885–894 (2021). https://doi.org/10.1007/s00404-021-06010-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-021-06010-0