Abstract
Purpose
This study aimed to analyze the hormone profiles, to detect the rate of hyperandrogenemia and to investigate the potential effect of Mayer–Rokitansky–Küster–Hauser syndrome (MRKHS) on ovarian reserve, as reflected by the serum Anti-Mullerian hormone (AMH) levels. Clinical implications were analyzed by including our own experiences with three patients after ovarian stimulation in preparation for uterus transplantation.
Methods
Serum samples of 100 patients with MRKHS (50 patients with MRKHS type 1 and 50 with type 2) were analyzed and compared to 50 individually age-matched healthy controls. Blood samples for hormone analyses were collected routinely during the clinical visit.
Results
The mean age was 20.0 years for MRKHS type 1, MRKHS type 2 and healthy controls. Compared to healthy controls, there was no significant difference in AMH values in the MRKH patients. As shown in previous studies, the proportion of hyperandrogenemia without clinical symptoms was significantly higher in MRKHS type 1 (52%; p < 0.001) and type 2 (56%; p < 0.001) patients when compared to age-matched controls. In preparation for uterus transplantation, three patients were stimulated with FSH/hMG for mean 14.2 days and the mean number of aspirated oocytes was 13.2 (3–22), while 8.3 (2–10) oocytes could be fertilized and cryopreserved. The mean fertilization rate was 51.2% (30–67%).
Conclusion
The rate of hyperandrogenemia was significantly higher in MRKH patients compared to healthy age-matched controls. Though, ovarian reserve (AMH level) was not reduced compared to controls. Future studies are needed to identify optimal ovarian stimulation protocols as well as to implement a systematic multicenter reporting system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
MRKHS, hyperandrogenemia and PCOS
MRKHS is characterized by uterovaginal agenesis, which can be found isolated (type 1, typical) or associated with renal, skeletal and other malformations (type 2, atypical). The prevalence is estimated at 1 in 5000 female live births [1, 19]. Patients are usually not diagnosed before adolescence and present with primary amenorrhea. Because of a normal female karyotype and functioning ovaries, patients show normal physical development, secondary sexual characteristics and a biphasic basal temperature curve in the vast majority of cases [15, 20]. However, abnormalities of the ovaries have been described in 15% [37] and 5.7% of MRKH patients [26] and ectopic ovaries in 41% of MRKH patients [17, 28].
From the embryological point of view and because of normal development of secondary sexual characteristics in MRKH patients, we would expect normal functioning ovaries and no higher rate of hormonal abnormalities compared to healthy controls. Nevertheless, there are several studies describing MRKH patients with aberrant gonadotrophin levels, hyperprolactinemia and hyperandrogenemia, leading to hormone phase irregularities with potentially longer follicular or luteal phases as well as probably low oocyte numbers [11, 16, 27, 28, 32, 38]. Recent studies showed that hyperandrogenemia is more often seen in women with MRKHS than in age-matched controls, but the biochemical findings are usually not associated with clinical symptoms like PCOS, hirsutism or acne [28, 32].
Polycystic ovary syndrome (PCOS) is the most frequent reproductive and metabolic disorder and affects 5–10% of women in their reproductive age [3]. Significantly higher AMH levels are shown in patients with PCOS [22, 40]. An increased prevalence of PCOS and Mullerian anomalies has already been described [39].
There is ongoing research about the etiology of the syndrome, which is mainly unknown. Several copy number variations have been detected recently, but were not found in larger groups of patients [4, 12, 23,24,25, 34]. WNT4 mutations have been found in an atypical form of MRKHS, always associated with clinical and biological signs of hyperandrogenism [5, 6, 30, 31, 38].
Ovarian reserve and motherhood options
AMH is secreted by granulosa cells during the woman’s fertile years. It reflects the remaining follicle pool and is used as a marker for ovarian reserve (OR). Its advantage over other fertility serum markers, such as follicle-stimulating hormone (FSH) or luteal hormone (LH), is its low variability throughout the menstrual cycle [18, 35, 41].
In the past, the majority of articles on MRKHS have focused on different techniques for the creation of a neovagina to enable the patients to have sexual intercourse. Although assisted reproductive techniques in these patients, aiming at becoming parents through gestational surrogacy has been available for over 25 years, the number of published studies on the clinical outcome in these patients is relatively limited [16]. The reproductive capabilities of the affected women have been investigated and described in a number of reports, but these, according to a recent review, include only 140 patients and do not contain systematic investigations of larger groups of patients [16].
Until recently, the only available motherhood options for women with this disorder were adoption or pregnancy with the help of a gestational surrogate carrier [9]. However, surrogacy is not allowed in many countries and has therefore not been a realistic option for the majority of affected women. The fact that uterus transplantation has been possible and successful in clinical trials opens up the chance to treat many young women with absolute uterine factor infertility worldwide and makes the need for data and experience concerning ovarian stimulation in MRKH patients even more obvious [7, 8].
Two previous studies showed reduced OR and a lower response rate after ovarian stimulation in MRKH type 2 patients [29, 33]. However, a recent comprehensive review found that the knowledge regarding expected success rates for MRKH patients undergoing in vitro fertilization (IVF) with a gestational carrier is not sufficient to draw conclusions and a systematic multicenter reporting system will be necessary [16].
The aim of the present study was to examine the impact of the two types of MRKHS on OR measured by the serum AMH levels and its relationship with hyperandrogenemia or other hormonal findings and certain life style factors. Potential clinical implications are shown by including our experiences from the first three patients undergoing ovarian stimulation in preparation of uterus transplantation.
Methods
Study design and participants
50 patients suffering from MRKHS type 1 and 50 suffering from MRKHS type 2 as well as 50 healthy controls were included in the study. All groups were individually age-matched. Age-matching was by year up to 25 years of age and due to small numbers in classes of 26–27, 28–30, and 31–35 years. All patients were recruited during routine clinical visits by the outpatient clinic of the Center for Rare Female Genital Malformations at the Department of Women´s Health at the Women´s University Hospital of Tuebingen. Patients included had proven MRKHS, a normal female 46, XX karyotype, normal pubertal development and normal secondary sexual characteristics. There were no MRKH patients with clitoral hypertrophy or hirsutism. Patients having received previous systemic cytotoxic treatment or with other known reasons with negative impact on OR, were excluded.
The healthy controls were recruited from the personal and professional environment of the conducting gynecologists.
We received prior approval from the Ethics Committee of Tuebingen University Hospital (No.: 392/2016BO1) with special approval concerning the recruitment of minors, as the MRKHS diagnosis is made in adolescence. All participants of the study gave written informed consent. In the case of minor age, written informed consent of at least one parent or legal guardian was obligatory.
All controls filled in a questionnaire on menstrual irregularities, lifestyle and obstetrical data and were asked if they used hormonal contraception (HC). From the MRKH patients, this data had already been collected during clinical visits.
Biochemical analyses
All patient serum samples were collected at the time of initial diagnosis, or at regular gynecological exams. Hormonal work-up (normal ranges are given in brackets) included total testosterone (11–19 years of age: 0.35–1.4 nmol/l, 20–39 years of age: 0.4–2.1 nmol/l), luteinizing hormone (LH) (follicle phase: 1.9–12.5 IU/l, midcyclical: 8.7–76.3 IU/l, luteal phase: 0.5–16.1 IU/l), follicle-stimulating hormone (FSH) (follicle phase: 2.5–10.2 IU/l, midcyclical: 3.4–33.4 IU/l, luteal phase: 1.5–9.1 IU/l), dehydroepiandrosterone sulfate (DHEAS) (18–19 years of age: 3.9–11.9 umol/l, 20–60 years of age: 0.8–11.5 umol/l), progesterone (luteal phase: 16–2000 nmol/l), estradiol (follicle phase: 70–530 pmol/l, midcyclical: 230–1300 pmol/l, luteal phase: 200–800 pmol/l), sex hormone-binding globulin (SHBG) (15–55 years of age: 30–90 nmol/l) and prolactin (< 21 ug/l).
Serum concentrations of SHBG and DHEAS were determined using the solid-phase chemiluminescent immunoassay system Immulite XPI and progesterone, LH, FSH, estradiol and testosterone concentrations were measured using the acridinium ester-based chemiluminescent immunoassay system ADVIA Centaur XPT (both from Siemens Healthineers, Eschborn, Germany). Concentrations of AMH were determined on the cobas e 411 electrochemiluminescence immunoassay analyzer. The normal ranges of AMH depending on age were: 20–24 years of age: 1.66–9.49 ng/ml, 25–29 years of age: 1.18–9.16 ng/ml, 30–34 years of age: 0.67–7.55 ng/ml, 35–39 years of age: 0.77–5.24 ng/ml.
Cycle phases were determined by progesterone values, whereas below 2.5 ng/ml was defined as follicular phase and above 5 ng/ml as luteal phase. Progesterone values between 2.5 ng/ml and 5 ng/ml and a LH/FSH ratio ≤ 1.5 corresponded to follicular phase, whereas LH/FSH ratio > 1.5 corresponded to the luteal phase. As a possible sign for PCOS, the LH/FSH ratio was calculated and defined pathological when > 2.
Statistical analyses
All statistical analyses were done using R version 3.3.2 (The R foundation for Statistical Computation, Vienna, Austria). We show numbers and percentages or means with ranges as appropriate. Differences in numbers for nominal data were tested by Fisher's exact test, differences in values for ordinal or continuous data were assessed by Wilcoxon Rank test. The association between AMH and age or BMI was estimated by the Pearson correlation coefficient. The significance level in all tests was chosen as 5%.
Results
Study cohort characteristics
The main clinical parameters are given in Table 1.
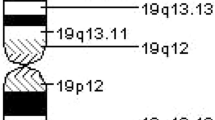
AMH
Compared to healthy controls (mean 3.5 (range 0.6–8.7) ng/ml), there was no significant difference in AMH values in patients with MRKHS type 1 (mean 2.9 (0.3–9.4) ng/ml; p = 0.094) or MRKHS type 2 (mean 3.8 (0.6–10.4) ng/ml; p = 0.831), and no significant difference was seen between the two MRKHS groups (p = 0.079) (Fig. 1, Table 2).
The rate of low, normal or high AMH values was not significantly different between the groups (type 1 versus control: p = 0.194, type 2 versus control: p = 0.845).
Within the control group, the use of HC had no significant influence on AMH values (p = 0.534).
Smoking had no significant effect on AMH in MRKH patients (only one control was a smoker) (p = 0.884).
None of the controls had previous ovarian surgery compared to 3/50 (6%) in MRKHS type 1 and 6/50 (12%) in type 2. There was no significant relation detected between previous surgery and AMH levels in MRKHS patients (p = 0.763).
One or both ovaries were elongated in 7/100 MRKH patients and cranialized in 20/100. These ovarian abnormalities were not associated with a higher rate of hormonal abnormalities.
Dependence of AMH on age was not as obvious as it would have been expected (correlation coefficient r = − 0.01, p = 0.834).
The BMI had no obvious effect on AMH (correlation coefficient r = 0.12, p = 0.114).
There was no significant difference in AMH values with or without hyperandrogenemia (all groups: p = 0.982).
Hyperandrogenemia- possible signs for PCOS
A significant higher rate of patients with hyperandrogenemia (elevated testosterone) was found in MRKHS type 1 (52%; p < 0.001) and type 2 (56%; p < 0.001) compared to healthy controls (8%). This was also true when controls under HC were excluded (MRKHS type 1 and type 2 versus control; p < 0.001) (Fig. 2, Table 2).
The LH/FSH ratio in controls without HC was not significantly different in comparison to MRKHS type 1 (mean 1.33 (range 0.17–5.86); p = 0.961) and MRKHS type 2 (mean 1.09 (range 0–3.89); p = 0.372). The rate of pathological LH/FSH ratios above 2 was 20% in MRKHS type 1 and 12% in type 2 patients, compared to 8.3% in controls without HC, which was different, but not on a significant level (p = 0.053). The free androgen index (FAI = total testosterone (nmol/l) × 100/SHBG (nmol/l) was significantly higher in controls without HC compared to controls using HC (p < 0.001). There was no significant difference of FAI between MRKHS type 1 and controls without HC (p = 0.961) or between MRKHS type 2 and controls without HC (p = 0.372).
There was no association of polycystic ovaries with hyperandrogenemia in MRKH patients on routine MRI or during laparoscopy.
Additional hormone analyses
Testosterone, LH, FSH and DHEAS were significantly higher in MRKHS type 1 and type 2 groups compared to all the controls and to those without HC. Prolactin was elevated in MRKH patients as well, but on a significant level only for type 1 and 2 compared to all the controls and for type 1 compared to non-HC controls (Table 2).
Ovarian stimulation (Table 3)
In preparation for a planned uterus transplantation, five ovarian stimulations in three MRKH type 1 patients were conducted at our department so far.
The patients had a mean age of 26.7 (23–34) years. Mean AMH was 2.92 (0.82–5.64) ng/ml. Hormone analyses were unremarkable in all the three patients. The patient´s partners showed normozoospermia. Depending on the AMH values, patients were stimulated with mean 201 (25–325) IE FSH/hMG per day, in total 2870 (2200–3950) IE per patient. The mean duration of treatment was 14.2 (11–18) days and the mean number of aspirated oocytes was 13.2 (3–22). 10.2 (3–17) oocytes could be used for intracytoplasmatic sperm injection (ICSI) and 8.3 (2–10) oocytes could be fertilized and cryopreserved. The mean fertilization rate was 51.2 (30–67)%. Oocyte retrieval was performed without any problems by the vaginal (neovaginal) route guided by ultrasound and with the patient under general anesthesia in the first two and under sedation and analgesia in the last one. There were no complications with ovarian stimulation or oocyte retrieval. The cryopreserved embryos were all of good quality.
Discussion
Very little is published about AMH levels in MRKHS [27] and no comparative studies between different ovarian stimulation protocols in MRKH patients exist. Therefore, the optimal protocol cannot be identified so far [16]. In contrast to Ozekinci et al., in our cohort AMH levels were not statistically significantly reduced in type 1 and not reduced in type 2 MRKHS [29]. There was no significant influence of smoking, BMI or previous ovarian surgery on AMH values in MRKH patients and no significant influence of HC in controls. In contrast to our results, Kallio et al. have shown a significant decrease of serum AMH during the use of all the combined hormonal contraceptives [21].
Because of functioning ovaries, MRKH patients show generally similar hormone levels as healthy controls and can be grouped into cyclic phases [11, 14, 32, 36]. On the other hand, there are several studies describing MRKH patients with aberrant gonadotrophin levels, hyperprolactinemia and hyperandrogenemia [11, 16, 27, 28, 32, 38].
The present study showed a significantly higher rate of hyperandrogenemia in type 1 and 2 MRKHS compared to individually age-matched controls. Prolactin was elevated significantly in type 1 and not significantly in type 2 MRKHS. As shown previously, PCOS is not likely to be responsible for the hyperandrogenemia of MRKH patients [32]. According to our preceding study, we could not detect significantly higher LH/FSH ratios or FAI in MRKH patients compared to controls. Hyperandrogenemia was not associated with polycystic ovaries (on MRI and laparoscopically). The presented high numbers with hyperandrogenemia cannot be easily explained. Like Oppelt et al. have reported recently, it is known that a steroid hormone exchange between the ovaries and uterus contributes to key regulatory mechanisms, especially during the menstrual cycle [13, 28]. The missing essential hormone crosstalk and regulation between ovary and uterus in MRKH patients, which was previously proposed [36], can be one explanation. The clinical implications of these results could also be a worse ovarian response after ovarian stimulation. But this still has to be shown, as our three cases had unremarkable hormone profiles.
Due to potentially ectopic location of the ovaries, difficulties in oocyte retrieval are possible and an abdominal approach might be necessary. Although the ovaries were located more cranially than normal in our three patients, vaginal oocyte retrieval was possible in all three cases, under general anesthesia in two of them and sedation and analgesia in the last one.
Raziel et al. reported superior ovarian response and embryo quality in type 1 compared to type 2 MRKH patients, while pregnancy rates in surrogate recipients were comparable [16, 33]. Nevertheless, pregnancy rates per cycle were nearly 50% lower compared to the general population [16]. In our cases, we had good ovarian responses using high stimulation doses with a common duration and a good oocyte number. Two of the patients had prior laroscopically assisted creation of a neovagina at our institution as described before [10] and the last one was after self-dilatation. Oocyte retrieval was uneventful and there were no complications during transplantation in the first patient. As with our surgical technique, no autotransplanted tissue is needed from other locations for vaginoplasty and as surgery does not result in neovaginal scar tissue, this technique might be one of the methods of choice, when ovarian stimulation and retrieval is planned and also concerning future uterus transplantation. The fertilization rate was lower compared to Raziel et al. [33], and to the German registry [2]. This aspect might have been influenced by the high oocyte number with a likely high number of immature oocytes.
The stimulation dose in our first three cases was selected to be higher than usual to generate sufficient oocytes, because there was only a minimal risk for ovarian hyperstimulation syndrome as a fresh embryo transfer was of course not possible. Because of resulting high numbers of immature and low-quality oocytes, there will be a modification in the future stimulation protocols including lower doses and resigning from step-up.
One of the strengths of this study is the large number of MRKH 1 and 2 patients as well as the inclusion of individually age-matched controls. As MRKHS is not a homogenous disease, the separate analysis of type 1 and 2 patients is obligatory for all kinds of studies and represents another strength of the present study.
One of the limitations of this study though is that nearly half of the controls were on HC, which made subgroup analyses necessary and these have disrupted the accuracy of the age-matching. Nevertheless, the use of HC in the control group could be excluded as a confounder on AMH values and it had no influence on the statistical significance in most of the other parameters (Table 2). Controls without HC were younger than MRKH patients and those on HC slightly older, but the range was comparable between all the groups (Table 2).
To our knowledge, this is the first study correlating hormone profiles with AMH levels in large cohorts of both types of young MRKH patients separately and comparing them to individually age-matched healthy controls. Like Oppelt et al. [28], we conclude that it is necessary to implement a more detailed hormone evaluation of MRKH patients and if necessary perform a corrective intervention for deregulated hormones, especially if assisted reproductive techniques are planned.
The results of three ovarian stimulation protocols from type 1 MRKH patients with unremarkable hormone profiles in preparation for the first uterus transplantations in Germany show uneventful retrieval procedures after good ovarian responses, but lower fertility rates compared to other groups, which will result in modifications to the stimulation protocols.
References
Aittomaki K, Eroila H, Kajanoja P (2001) A population-based study of the incidence of Mullerian aplasia in Finland. Fertil Steril 76:624–625
Anonymous (2016) Deutsches IVF Register (DIR), Jahrbuch 2015. modif. Reprint from J Reproduktionsmed Endokrinol 13
Balen A (2004) The pathophysiology of polycystic ovary syndrome: trying to understand PCOS and its endocrinology. Best Pract Res Clin Obstet Gynaecol 18:685–706
Bernardini L, Gimelli S, Gervasini C et al (2009) Recurrent microdeletion at 17q12 as a cause of Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome: two case reports. Orphanet J Rare Dis 4:25
Biason-Lauber A, De Filippo G, Konrad D et al (2007) WNT4 deficiency–a clinical phenotype distinct from the classic Mayer-Rokitansky-Kuster-Hauser syndrome: a case report. Hum Reprod 22:224–229
Biason-Lauber A, Konrad D, Navratil F et al (2004) A WNT4 mutation associated with Mullerian-duct regression and virilization in a 46, XX woman. N Engl J Med 351:792–798
Brannstrom M, Bokstrom H, Dahm-Kahler P et al (2016) One uterus bridging three generations: first live birth after mother-to-daughter uterus transplantation. Fertil Steril 106:261–266
Brannstrom M, Johannesson L, Bokstrom H et al (2015) Livebirth after uterus transplantation. Lancet 385:607–616
Brannstrom M, Johannesson L, Bokstrom H et al (2015) Livebirth after uterus transplantation. Lancet 385:607–616
Brucker SY, Gegusch M, Zubke W et al (2008) Neovagina creation in vaginal agenesis: development of a new laparoscopic Vecchietti-based procedure and optimized instruments in a prospective comparative interventional study in 101 patients. Fertil Steril 90:1940–1952
Carranza-Lira S, Forbin K, Martinez-Chequer JC (1999) Rokitansky syndrome and MURCS association—clinical features and basis for diagnosis. Int J Fertil Womens Med 44:250–255
Chen MJ, Wei SY, Yang WS et al (2015) Concurrent exome-targeted next-generation sequencing and single nucleotide polymorphism array to identify the causative genetic aberrations of isolated Mayer-Rokitansky-Kuster-Hauser syndrome. Hum Reprod 30:1732–1742
Cicinelli E, Einer-Jensen N, Cignarelli M et al (2004) Preferential transfer of endogenous ovarian steroid hormones to the uterus during both the follicular and luteal phases. Hum Reprod 19:2001–2004
Folch M, Pigem I, Konje JC (2000) Mullerian agenesis: etiology, diagnosis, and management. Obstet Gynecol Surv 55:644–649
Fraser IS, Baird DT, Hobson BM et al (1973) Cyclical ovarian function in women with congenital absence of the uterus and vagina. J Clin Endocrinol Metab 36:634–637
Friedler S, Grin L, Liberti G et al (2016) The reproductive potential of patients with Mayer-Rokitansky-Kuster-Hauser syndrome using gestational surrogacy: a systematic review. Reprod Biomed Online 32:54–61
Hall-Craggs MA, Kirkham A, Creighton SM (2013) Renal and urological abnormalities occurring with Mullerian anomalies. J Pediatr Urol 9:27–32
Hansen KR, Knowlton NS, Thyer AC et al (2008) A new model of reproductive aging: the decline in ovarian non-growing follicle number from birth to menopause. Hum Reprod 23:699–708
Herlin M, Bjorn AM, Rasmussen M et al (2016) Prevalence and patient characteristics of Mayer-Rokitansky-Kuster-Hauser syndrome: a nationwide registry-based study. Hum Reprod 31:2384–2390
Jb B (1959) Preliminary observation on urinary oestrogen excretion in certain gynaecological disorders. J Obstet Gynaecol Br Commonw 66:177–211
Kallio S, Puurunen J, Ruokonen A et al (2013) Antimullerian hormone levels decrease in women using combined contraception independently of administration route. Fertil Steril 99:1305–1310
Kim JY, Tfayli H, Michaliszyn SF et al (2017) Anti-Mullerian Hormone in Obese Adolescent Girls With Polycystic Ovary Syndrome. J Adolesc Health 60:333–339
Ledig S, Schippert C, Strick R et al (2011) Recurrent aberrations identified by array-CGH in patients with Mayer-Rokitansky-Kuster-Hauser syndrome. Fertil Steril 95:1589–1594
Morcel K, Watrin T, Pasquier L et al (2011) Utero-vaginal aplasia (Mayer-Rokitansky-Kuster-Hauser syndrome) associated with deletions in known DiGeorge or DiGeorge-like loci. Orphanet J Rare Dis 6:9
Nik-Zainal S, Strick R, Storer M et al (2011) High incidence of recurrent copy number variants in patients with isolated and syndromic Mullerian aplasia. J Med Genet 48:197–204
Oppelt P, Renner SP, Kellermann A et al (2006) Clinical aspects of Mayer-Rokitansky-Kuester-Hauser syndrome: recommendations for clinical diagnosis and staging. Hum Reprod 21:792–797
Oppelt P, Strissel PL, Kellermann A et al (2005) DNA sequence variations of the entire anti-Mullerian hormone (AMH) gene promoter and AMH protein expression in patients with the Mayer-Rokitanski-Kuster-Hauser syndrome. Hum Reprod 20:149–157
Oppelt PG, Mueller A, Stephan L et al. (2017) Hyperandrogenemia and high prolactin in congenital utero-vaginal aplasia patients. Reproduction
Ozekinci M, Erman Akar M, Senol Y et al (2015) Comparison of markers of ovarian reserve between patients with complete mullerian agenesis and age-matched fertile and infertile controls. Fertil Steril 104:176–179
Philibert P, Biason-Lauber A, Gueorguieva I et al (2011) Molecular analysis of WNT4 gene in four adolescent girls with mullerian duct abnormality and hyperandrogenism (atypical Mayer-Rokitansky-Kuster-Hauser syndrome). Fertil Steril 95:2683–2686
Philibert P, Biason-Lauber A, Rouzier R et al (2008) Identification and functional analysis of a new WNT4 gene mutation among 28 adolescent girls with primary amenorrhea and mullerian duct abnormalities: a French collaborative study. J Clin Endocrinol Metab 93:895–900
Rall K, Conzelmann G, Schaffeler N et al (2014) Acne and PCOS are less frequent in women with Mayer-Rokitansky-Kuster-Hauser syndrome despite a high rate of hyperandrogenemia: a cross-sectional study. Reprod Biol Endocrinol 12:23
Raziel A, Friedler S, Gidoni Y et al (2012) Surrogate in vitro fertilization outcome in typical and atypical forms of Mayer-Rokitansky-Kuster-Hauser syndrome. Hum Reprod 27:126–130
Sandbacka M, Halttunen M, Jokimaa V et al (2011) Evaluation of SHOX copy number variations in patients with Mullerian aplasia. Orphanet J Rare Dis 6:53
Sowers M, Mcconnell D, Gast K et al (2010) Anti-Mullerian hormone and inhibin B variability during normal menstrual cycles. Fertil Steril 94:1482–1486
Strissel PL, Oppelt P, Cupisti S et al (2009) Assessment of pituitary and steroid hormones and members of the TGF-beta superfamily for ovarian function in patients with congenital uterus and vaginal aplasia (MRKH syndrome). Horm Metab Res 41:408–413
Strubbe EH, Willemsen WN, Lemmens JA et al (1993) Mayer-Rokitansky-Kuster-Hauser syndrome: distinction between two forms based on excretory urographic, sonographic, and laparoscopic findings. AJR Am J Roentgenol 160:331–334
Sultan C, Biason-Lauber A, Philibert P (2009) Mayer-Rokitansky-Kuster-Hauser syndrome: recent clinical and genetic findings. Gynecol Endocrinol 25:8–11
Ugur M, Karakaya S, Zorlu G et al (1995) Polycystic ovaries in association with mullerian anomalies. Eur J Obstet Gynecol Reprod Biol 62:57–59
Verma AK, Rajbhar S, Mishra J et al (2016) Anti-mullerian hormone: a marker of ovarian reserve and its association with polycystic ovarian syndrome. J Clin Diagn Res 10:QC10–QC12
Visser JA, De Jong FH, Laven JS et al (2006) Anti-Mullerian hormone: a new marker for ovarian function. Reproduction 131:1–9
Acknowledgements
The authors thank all patients who participated in this study and Sabine Hofmeister for her help with the biobank. The present data/results were part of the MD thesis work of Ludmila Jurow (L. Jurow, unpublished thesis work). She fully agreed to include the present data.
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Contributions
MH: protocol/project development, data analysis, manuscript writing/editing. KR: protocol/project development, data collection, data analysis, manuscript writing/editing. LJ: data collection, data analysis. AP: hormone analyses. BS: age-matching, data analysis (statistics). FAT: critical revision of manuscript. MH: critical revision of manuscript. HS: archiving of blood samples, critical revision of manuscript. SYB: data collection, critical revision of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors state that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Henes, M., Jurow, L., Peter, A. et al. Hyperandrogenemia and ovarian reserve in patients with Mayer–Rokitansky–Küster–Hauser syndrome type 1 and 2: potential influences on ovarian stimulation. Arch Gynecol Obstet 297, 513–520 (2018). https://doi.org/10.1007/s00404-017-4596-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4596-1