Abstract
Purpose
There is low evidence regarding the optimal treatment in patients with uterine sarcomas and malignant mixed Mullerian tumors (MMMTs). This study provides an overview of experience at our center with patients diagnosed with uterine sarcoma and MMMT, in relation to the clinical management and outcome.
Methods
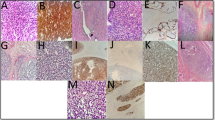
The medical records for 143 patients with low-grade endometrial stromal sarcoma (ESS), leiomyosarcoma (LMS), and high-grade (undifferentiated) endometrial sarcoma (UES) and MMMT were reviewed. All available clinical and pathological data were collected and analyzed. Putative prognostic factors were entered into a multivariate analysis using a Cox proportional hazards ratio model, and survival data were calculated.
Results
The 5-year overall survival rates were significantly different between patients with ESS, LMS, and UES and MMMT (86 vs. 40 vs. 57 vs. 45 %; P < 0.001). The multivariate analysis showed that the patients’ age, higher FIGO stage (III–IV), a history of smoking, prior pelvic radiation, diabetes, and residual tumor after surgery were associated with a poorer overall survival. Histological subtypes of LMS (HR 4.68; 95 % CI 1.35–16.17), UES (HR 1.21; 95 % CI 0.26–5.77) and MMMT (HR 1.63; 95 % CI 0.42–6.43) were also associated with a poorer overall survival than ESS (P = 0.008). Adjuvant therapies showed no associations with overall survival.
Conclusions
Adjuvant therapy has so far not shown any overall survival benefit, and the focus is therefore on primary surgery. In future studies, the entities should be investigated separately in relation to prognostic factors and effective therapeutic management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Uterine sarcomas are very rare malignancies of the uterus, representing up to 8 % of uterine malignancies [1, 2]. Their incidence increases with age and is reported to be 0.5–2.1 per 100,000 women per year between the ages of 35 and 64 [2].
Various histological subtypes are summarized under the term “uterine sarcoma.” The most common, occurring in 60–70 % of cases, is leiomyosarcoma (LMS), followed by low-grade endometrial stromal sarcoma (ESS) at about 15–20 %, and high-grade (undifferentiated) endometrial sarcoma (UES) and adenosarcoma (AS), which are rarer [1]. MMMTs are synonymous to carcinosarcomas and have a special position, as these lesions can consist of a malignant epithelial and a malignant mesenchymal part. They were also formerly classified as uterine sarcomas. Nowadays, there is general agreement that most MMMTs derive from sarcomatous differentiation in high-grade endometrial carcinoma [3, 4]. They are therefore staged analogously to endometrial carcinoma. By contrast, LMS, ESS, UES, and AS are staged using the recent 2009 FIGO staging system [5]. However, due to the poorer prognosis in comparison with the common endometrial lesions, MMMTs were included in retrospective studies of uterine sarcomas and for this reason also in this study.
In view of the usually very poor prognosis, with a survival rate often less than 50 %, the patients receive extended surgery followed by adjuvant chemotherapy, radiotherapy, or endocrine therapy, depending on the histological subtype [6–11]. Due to the rarity of uterine sarcomas, there is no consensus regarding the optimal treatment of the affected patients. Actually, in August 2015 a new good clinical practice guideline for the treatment of patients with uterine sarcomas and carcinosarcomas was published [12]. The present study provides an overview of experience with patients diagnosed with uterine sarcoma and MMMTs at the Gynecological Cancer Center in the Department of Gynecology and Obstetrics at Erlangen University Hospital, describing the clinical presentation, management, histological parameters, prognosis, and outcome.
Patients and methods
This retrospective study was conducted at the Gynecological Cancer Center in the Department of Gynecology and Obstetrics at Erlangen University Hospital. Using the institution’s database, a total of 163 women with a diagnosis of uterine sarcoma were identified who had been included in the clinical cancer registry at Erlangen–Nuremberg University between 1984 and 2013. The diagnoses recorded in the registry were compared with the patients’ medical records manually. No medical records were found in three cases. Six patients had to be excluded due to a diagnosis of endometrial cancer. A further 11 patients were excluded because of the rarity of the diagnosis (two with fibrosarcoma, one with Kaposi sarcoma, two with PEComa, three with rhabdomyosarcoma, and three with adenosarcoma). Finally, 143 patients with low-grade endometrial stromal sarcoma (ESS), leiomyosarcoma (LMS), high-grade (undifferentiated) endometrial sarcoma (UES) or malignant mixed Mullerian tumors (MMMT) remained.
The medical records for these patients were examined retrospectively for demographic data, clinical and pathological data, and management. Their medical records and the registry at Erlangen–Nuremberg University were used to trace follow-up and outcome. The FIGO stage was reassessed retrospectively for each patient using the latest recommendations for the FIGO staging system [5]. All the data were entered into a database and analyzed using IBM SPSS Statistics for Windows, Version 22.0 (IBM Corporation, Armonk, NY, USA).
Data were collected on the following aspects: age, postmenopausal status, body mass index (BMI), history of smoking, symptoms at diagnosis, sonographic findings, history of prior cancer, tamoxifen administration, pelvic radiotherapy, obstetric history, history of comorbidities such as hypertension and diabetes, surgical procedures, histological subtype, FIGO stage, grade, surgical margins, adjuvant treatments, recurrences, and survival status.
In addition to a general statistical description of the population, analysis of variance (ANOVA) was used to analyze continuous characteristics (age, BMI), the Kruskal–Wallis test for ordinal categorical characteristics (FIGO stage, previous pregnancies, previous births, grade); the χ 2 test for categorical characteristics; and Fisher’s exact test for categorical characteristics if the expected frequency for the χ 2 test was less than 20 % or less than five cases (pain at diagnosis, tamoxifen intake, prior pelvic radiotherapy, prior cancer, history of diabetes and smoking, lymph-node status, primary distant metastases, histological subtype, hysterectomy, salpingo-oophorectomy, and adjuvant endocrine therapy).
Known general prognostic factors and specific prognostic factors (if known) for the different histological subtypes of sarcoma were subsequently entered into a multivariate analysis using the Cox proportional hazards ratio model. The disease-free survival (DFS) was calculated in patients with remission from the date of remission to the date of first recurrence. Overall survival (OS) was calculated in all patients from the date of diagnosis to the date of death or last contact. Kaplan–Meier curves were generated from the survival data. A P value <0.05 was considered to be statistically significant.
Results
Clinical data
Data for a total of 143 patients with uterine sarcoma were collected (Table 1; further data are also provided in the supplement). The median age at diagnosis was 58.2 years (range 23–90 years). Forty-nine patients had MMMT, 23 had ESS, 57 had LMS, and 14 had UES. The median ages of the patients in the four subgroups were 64.7 years with MMMT, 49.6 years with ESS, 53.3 years with LMS, and 59.7 years with UES. The mean body mass index in the groups was 25.8–27.4 kg/m2. The patients’ postmenopausal status differed significantly between the four groups.
Vaginal bleeding was most common in UES, MMMT, and ESS, in 81–92 % of cases. Pain as a symptom was most frequently reported by patients with LMS, in 32 % of cases. Abnormal sonographic findings, like mixed echogenic and poor echogenic parts, central necrosis, and color Doppler findings of irregular vessel distribution were most commonly noted in patients with ESS and LMS, in 38 % of cases.
A total of four patients had a history of tamoxifen administration. Three patients (6 %) with MMMT had undergone pelvic radiotherapy (one each for bladder cancer, anal cancer, and cervical cancer) before the diagnosis of sarcoma. Eleven patients (22 %) with MMMT had medical histories including previous cancer diagnosis, like malignant melanoma, anal cancer, colorectal cancer, bladder cancer, cervical cancer (each once), ovarian cancer (twice) and breast cancer (four times). Diabetes was most common in patients with MMMT (24 %) and UES (31 %). The patients had hypertension in 32–49 % of cases and a history of smoking in 12–36 %.
Surgical treatment and pathological findings
The diagnosis of sarcoma was known before surgery, due to curettage or biopsy, in 66 cases (46 %). In all other cases diagnosis of uterine sarcoma or MMMT was an incidental finding. Surgery was indicated on spec of uterus myomatosus or adenomyosis uteri due to bleeding irregularity or pain symptomatic. In two patients with ESS and three patients with LMS, enucleation of a putative myoma had been carried out primarily.
Almost all of the patients (86–100 %) underwent hysterectomy. In eight cases the reason not to perform a hysterectomy was an inoperable situs or extra-abdominal primary distant metastases. Salpingo-oophorectomy was carried out in only 65 and 74 %, respectively, of patients with LMS and ESS. Omentectomy was carried out in 7–35 % of the patients. Lymphadenectomy was performed in case of suspicious lymph nodes and depending of the histological type, though the variable indication is a weak point and purely owed to limited data in early time of recruiting between 1984 until 2013. Two-thirds of patients with MMMT underwent pelvic lymphadenectomy, in comparison with 57 % of those with UES, 17 % of those with ESS, and 37 % of those with LMS. Aortic lymphadenectomy was performed in 43 % of patients with MMMT, 29 % of those with UES, 21 % of those with LMS, and 9 % of those with ESS. The mean number of lymph nodes removed was 35 (range 4–76). Eighty patients (63 %) were in FIGO stage I, eight (6 %) in stage II, 23 (18 %) in stage III, and 17 (13 %) in stage IV (Table 2; further data are also provided in the supplement).
The groups differed with regard to lymph-node status. Primary distant metastases (for example peritoneal) were found in 9–21 % of cases. There was residual tumor after surgery in 15 patients (13 %), which is defined as macroscopic abdominal tumor rest during surgery.
Adjuvant therapy
Patients with UES (43 %) or MMMT (35 %) most often received chemotherapy. Applied chemotherapy was ifosfamid and taxane, ifosfamid and anthracycline, gemcitabine and taxane, the CYVADIC regimen, which consists of cyclophosphamide, vincristine, doxorubicin, and dacarbazine and combinations with platin. Patients with UES and MMMT also underwent radiotherapy most often (in 43 and 51 % of cases, respectively). Endocrine therapy was administered most often in patients with ESS (18 %) (Table 2; further data are also provided in the supplement).
Patients without hysterectomy received chemotherapy (ifosfamid and paclitaxel or ifosfamid and anthracycline; one patient each), endocrine therapy (once) and radiotherapy (three times). Three patients of these received no further therapy.
Outcome and prognostic factors
The median follow-up period of 108 patients was 119 months/9.9 years (range 1–415 months/0.1–34.1 years). A total of 35 patients (24 %) were lost to follow-up for calculating the disease-free survival. The 5-year disease-free survival rates were 43 % in patients with MMMT, 66 % in those with ESS, 41 % in those with LMS, and 79 % in those with UES (P = 0.179), and the median disease-free survival was 44 months/3.6 years in patients with MMMT, 92 months/7.5 years in patients with ESS, and 37 months/3.0 years in patients with LMS (Fig. 1). The median disease-free survival was not reached in patients with UES. Forty-six of 108 patients (42 %) developed recurrences: 13 of 35 with MMMT (37 %), eight of 22 with ESS (36 %), 22 of 40 with LMS (55 %), and three of 11 with UES (27 %; P = 0.226).
Disease-free survival relative to the histological subtype of uterine sarcoma and malignant mixed Mullerian tumor. MMMT malignant mixed Mullerian tumor, ESS endometrial stromal sarcoma, LMS leiomyosarcoma, UES high-grade (undifferentiated) endometrial sarcoma, censored, each tick mark represents the time one patient was censored
The overall 5-year survival rates were significantly different between patients with MMMT, ESS, LMS, and UES (45 vs. 86 vs. 40 vs. 57 %; P < 0.001) (Fig. 2). The median overall survival was 50 months/4.1 years with MMMT, 233 months/19.1 years with ESS, 30 months/2.5 years with LMS, and 110 months/9.0 years with UES.
Overall survival relative to the histological subtype of uterine sarcoma and malignant mixed Mullerian tumor. MMMT malignant mixed Mullerian tumor, ESS endometrial stromal sarcoma, LMS leiomyosarcoma, UES high-grade (undifferentiated) endometrial sarcoma, censored, each tick mark represents the time one patient was censored
The multivariate analysis (Table 3)—adjusting for age, histological subtype, FIGO stage (I–II vs. III–IV), grade, residual tumor after surgery, adjuvant therapy (chemotherapy, radiotherapy, endocrine therapy), and patient history (pelvic radiation, diabetes, smoking)—showed that the patients’ age, higher FIGO stage (III–IV), history of smoking, prior pelvic radiation, diabetes, and residual tumor after surgery were associated with a poorer overall survival. Histological subtypes of uterine sarcomas, like LMS (HR 4.68; 95 % CI 1.35–16.17) and UES (HR 1.21; 95 % CI 0.26–5.77), just as MMMT (HR 1.63; 95 % CI 0.42–6.43), were also associated with a poorer overall survival in comparison with ESS (P = 0.008). Adjuvant radiotherapy showed a statistical trend toward better overall survival (HR 0.43; 95 % CI 0.18–1.03, P = 0.059). The other adjuvant therapies showed no associations with overall survival.
Discussion
In the present study, patients with different uterine sarcomas and MMMT presented at different ages and with different symptoms at diagnosis. Some of the surgical and adjuvant treatments for uterine sarcomas differed.
The data show that different histological subgroups of uterine sarcomas and MMMT are associated with different 5-year overall survival rates, ranging from 40 to 86 %. The multivariate analysis showed that poorer overall survival was associated with the patients’ age, a higher FIGO stage (III–IV), residual tumor after surgery, diabetes, a history of smoking, and prior pelvic radiotherapy. Histological subtypes of LMS and UES, just as MMMT were also associated with a poorer overall survival than ESS.
Patients with ESS or LMS are usually younger then patients with MMMT or UES, as this study shows (median ages 49.6 and 53.5 years vs. 64.7 and 59.7 years) [11]. The most frequent symptom at diagnosis was vaginal bleeding in patients with MMMT, ESS and UES in 81–92 % of the present group. Similar findings have also been reported in other studies [1, 13]. Most patients with MMMT (98 %) were postmenopausal, in comparison with 45 % of those with ESS and 62 % of those LMS, a finding that is also consistent with other studies [1, 13].
Hysterectomy with bilateral salpingo-oophorectomy is considered to be an effective treatment for uterine sarcoma [14]. However, the benefits of salpingo-oophorectomy are not seen in patients with LMS and ESS [15, 16]. Ovarian preservation can be considered in premenopausal women with early LMS and ESS [17]. Most of the patients in the present study underwent hysterectomy (86–100 %). Salpingo-oophorectomy was performed in 94 % of patients with MMMT and 86 % of those with UES. Patients with ESS and LMS underwent salpingo-oophorectomy in 74 and 65 % of cases, respectively.
Pelvic and aortic lymphadenectomy is not routinely indicated in patients with LMS, as the incidence of lymphatic spread is only approximately 3 % in the early stages [14, 18]. The rate of nodal metastases in ESS varies up to 10 %, and resection of suspicious lymph nodes is therefore an accepted procedure. Systematic lymphadenectomy in patients with clinically negative nodes is a matter of controversy [19, 20]. The same also applies to UES. Systematic pelvic and aortic lymphadenectomy is recommended in patients with MMMT [8, 9, 14]. In the present study, 67 % of patients with MMMT underwent pelvic lymphadenectomy and 43 % received aortic lymphadenectomy. Fewer patients received these treatments with LMS and EES (37 % pelvic and 21 % aortic, 17 % pelvic and 9 % aortic, respectively).
The present study did not identify any overall survival benefit in association with adjuvant chemotherapy, radiotherapy, or endocrine therapy in any of the histological groups. In another retrospective study of 49 patients with uterine sarcoma and MMMT there was benefit in five-year overall survival in patients with radiotherapy [21].
In patients with LMS and ESS, adjuvant radiotherapy does not offer any benefit in relation to overall survival [22]. Two randomized studies in patients with LMS did not show any overall survival benefit with adjuvant chemotherapy with doxorubicin (60 mg/m2, every 3 weeks, eight cycles) or with four cycles of adjuvant chemotherapy with doxorubicin (50 mg/m2, d1), ifosfamide (3 g/m2, d1–2), and cisplatin (75 mg/m2, d3) [23, 24]. A meta-analysis has shown that the prognosis is improved by a combination of chemotherapies, mainly with doxorubicin and ifosfamide [25]. However, it is difficult to draw conclusions in a proportion of non-LMS lesions. Chemotherapy is not useful in patients with ESS; hormonal therapy may be an option in those with advanced stages of ESS [26]. Data for UES are lacking. A randomized study has shown that there is no overall survival benefit for patients with MMMT with adjuvant radiotherapy of the pelvis, in comparison with observation alone [22]. In a retrospective study of the Surveillance, Epidemiology, and End Results (SEER) database, multivariate analysis showed an association with overall survival for adjuvant radiotherapy in patients with MMMT at all stages [27]. Another analysis of the SEER database also showed improvement in the overall survival after radiotherapy in patients with MMMT in stages I and II [28]. In a randomized study of 232 patients with MMMT, adjuvant chemotherapy with cisplatin and ifosfamide showed a reduction in the risk of recurrence by 29 % in comparison with whole-abdomen radiotherapy, but the overall survival did not improve [29].
The multivariate analysis showed that the histological subtype of uterine sarcoma has a significant effect on the overall survival. The literature data are contradictory here. Some authors have only identified a difference for ESS [30]; other studies have reported that MMMT is associated with a poorer prognosis in comparison with the other uterine sarcomas [13]. In contrast, it has also been shown that LMS is associated with a poorer prognosis than MMMT [31]. In the present study, LMS showed the poorest prognosis, with a 5-year overall survival rate of 40 %, followed by MMMT at 45 %, UES at 57 %, and ESS at 86 % (P < 0.001). In the multivariate analysis, LMS was found to be associated with the highest risk for death (HR 4.68; 95 % CI 1.35–16.17), followed by MMMT (HR 1.63; 95 % CI 0.42–6.43) and UES (HR 1.21; 95 % CI 0.26–5.77), in comparison with ESS (P = 0.008).
As in other studies, the present study also shows that the FIGO stage is independently associated with overall survival [1, 13, 14]. Higher age was also associated with a poorer prognosis in this study; this has also been demonstrated in other studies [32], although some studies have not confirmed the finding [33, 34]. Residual tumor after surgery, a history of diabetes, a history of smoking, and prior pelvic radiotherapy were found to be independent prognostic factors in the present study.
Various studies have been conducted on LMS, without consistent findings regarding survival and patient age, clinical stage, tumor size, presence of necrosis, mitotic rate, degree of nuclear pleomorphism, or vascular invasion [18, 35–37]. Several clinicopathologic factors have been described to help predict the outcome in patients with ESS, such as age, ethnicity, FIGO stage, depth of myometrial invasion, tumor grade, mitotic activity, and DNA ploidy [1, 38, 39]. In UES, vascular invasion has been found to be a prognostic factor [40]. In addition to the surgical stage in MMMT, depth of myometrial invasion in particular is the most important prognostic factor [41].
A strength of the present study is the median follow-up period of 119 months in 108 patients (35 patients were lost of follow up). The study is of course retrospective. Uterine sarcomas and MMMT are today regarded as different tumor entities; studies on the single entities are important but rare, due to the small numbers of patients with uterine sarcoma.
In conclusion, the present study confirms that uterine sarcomas and MMMTs are very rare tumors with a very poor prognosis. The prognosis appears to depend on the tumor stage and tumor entity. The role of adjuvant therapy is not clearly defined. Until now, no overall survival benefit has been demonstrated with adjuvant therapy, and the focus is therefore on primary surgery. In future studies, the entities should be investigated separately in relation to the prognostic factors involved and effective therapeutic management.
References
D’Angelo E, Prat J (2010) Uterine sarcomas: a review. Gynecol Oncol 116(1):131–139. doi:10.1016/j.ygyno.2009.09.023
Brooks SE, Zhan M, Cote T, Baquet CR (2004) Surveillance, epidemiology, and end results analysis of 2677 cases of uterine sarcoma 1989–1999. Gynecol Oncol 93(1):204–208. doi:10.1016/j.ygyno.2003.12.029
Kernochan LE, Garcia RL (2009) Carcinosarcomas (malignant mixed Mullerian tumor) of the uterus: advances in elucidation of biologic and clinical characteristics. J Natl Compr Cancer Netw 7(5):550–556
Lopez-Garcia MA, Palacios J (2010) Pathologic and molecular features of uterine carcinosarcomas. Semin Diagn Pathol 27(4):274–286
Prat J (2009) FIGO staging for uterine sarcomas. Int J Gynaecol Obstet 104(3):177–178. doi:10.1016/j.ijgo.2008.12.008
Barney B, Tward JD, Skidmore T, Gaffney DK (2009) Does radiotherapy or lymphadenectomy improve survival in endometrial stromal sarcoma? Int J Gynecol Cancer 19(7):1232–1238. doi:10.1111/IGC.0b013e3181b33c9a
Callister M, Ramondetta LM, Jhingran A, Burke TW, Eifel PJ (2004) Malignant mixed Mullerian tumors of the uterus: analysis of patterns of failure, prognostic factors, and treatment outcome. Int J Radiat Oncol Biol Phys 58(3):786–796. doi:10.1016/S0360-3016(03)01561-X
Garg G, Shah JP, Kumar S, Bryant CS, Munkarah A, Morris RT (2010) Ovarian and uterine carcinosarcomas: a comparative analysis of prognostic variables and survival outcomes. Int J Gynecol Cancer 20(5):888–894. doi:10.1111/IGC.0b013e3181dc8292
Nemani D, Mitra N, Guo M, Lin L (2008) Assessing the effects of lymphadenectomy and radiation therapy in patients with uterine carcinosarcoma: a SEER analysis. Gynecol Oncol 111(1):82–88. doi:10.1016/j.ygyno.2008.05.016
Pelmus M, Penault-Llorca F, Guillou L, Collin F, Bertrand G, Trassard M, Leroux A, Floquet A, Stoeckle E, Thomas L, MacGrogan G (2009) Prognostic factors in early-stage leiomyosarcoma of the uterus. Int J Gynecol Cancer 19(3):385–390. doi:10.1111/IGC.0b013e3181a1bfbc
Schick U, Bolukbasi Y, Thariat J, Abdah-Bortnyak R, Kuten A, Igdem S, Caglar H, Ozsaran Z, Lossl K, Schleicher U, Zwahlen D, Villette S, Vees H (2012) Outcome and prognostic factors in endometrial stromal tumors: a Rare Cancer Network study. Int J Radiat Oncol Biol Phys 82(5):e757–e763. doi:10.1016/j.ijrobp.2011.11.005
Sarcoma of the uterus. Guideline of German Society of Gynecology and Obstetrics (S2 k-Leve, AWMF Registry No. 015/074, August 2015). http://www.awmf.org/leitlinien/detail/II/015-074.html
Benito V, Lubrano A, Arencibia O, Andujar M, Alvarez E, Medina N, Falcon JM, Falcon O (2009) Clinicopathologic analysis of uterine sarcomas from a single institution in the Canary Islands. Int J Gynaecol Obstet 107(1):44–49. doi:10.1016/j.ijgo.2009.05.020
Gadducci A, Cosio S, Romanini A, Genazzani AR (2008) The management of patients with uterine sarcoma: a debated clinical challenge. Crit Rev Oncol Hematol 65(2):129–142. doi:10.1016/j.critrevonc.2007.06.011
El-Khalfaoui K, du Bois A, Heitz F, Kurzeder C, Sehouli J, Harter P (2014) Current and future options in the management and treatment of uterine sarcoma. Ther Adv Med Oncol 6(1):21–28. doi:10.1177/1758834013513314
Harter P, El-Khalfaoui K, Heitz F, du Bois A (2014) Operative and conservative treatment of uterine sarcomas. Geburtsh Frauenheilk 74(3):267–270. doi:10.1055/s-0034-1368204
Li AJ, Giuntoli RL 2nd, Drake R, Byun SY, Rojas F, Barbuto D, Klipfel N, Edmonds P, Miller DS, Karlan BY (2005) Ovarian preservation in stage I low-grade endometrial stromal sarcomas. Obstet Gynecol 106(6):1304–1308. doi:10.1097/01.AOG.0000185511.91694.1e
Giuntoli RL 2nd, Metzinger DS, DiMarco CS, Cha SS, Sloan JA, Keeney GL, Gostout BS (2003) Retrospective review of 208 patients with leiomyosarcoma of the uterus: prognostic indicators, surgical management, and adjuvant therapy. Gynecol Oncol 89(3):460–469
Reich O, Winter R, Regauer S (2005) Should lymphadenectomy be performed in patients with endometrial stromal sarcoma? Gynecol Oncol 97(3):982. doi:10.1016/j.ygyno.2005.01.034
Riopel J, Plante M, Renaud MC, Roy M, Tetu B (2005) Lymph node metastases in low-grade endometrial stromal sarcoma. Gynecol Oncol 96(2):402–406. doi:10.1016/j.ygyno.2004.10.021
Soumarova R, Horova H, Seneklova Z, Ruzickova J, Horova I, Budikova M, Slampa P, Kalabova R (2002) Treatment of uterine sarcoma. A survey of 49 patients. Arch Gynecol Obstet 266(2):92–95
Reed NS, Mangioni C, Malmstrom H, Scarfone G, Poveda A, Pecorelli S, Tateo S, Franchi M, Jobsen JJ, Coens C, Teodorovic I, Vergote I, Vermorken JB, European Organisation for R, Treatment of Cancer Gynaecological Cancer G (2008) Phase III randomised study to evaluate the role of adjuvant pelvic radiotherapy in the treatment of uterine sarcomas stages I and II: an European Organisation for Research and Treatment of Cancer Gynaecological Cancer Group Study (protocol 55874). Eur J Cancer 44 (6):808–818. doi:10.1016/j.ejca.2008.01.019
Omura GA, Blessing JA, Major F, Lifshitz S, Ehrlich CE, Mangan C, Beecham J, Park R, Silverberg S (1985) A randomized clinical trial of adjuvant adriamycin in uterine sarcomas: a Gynecologic Oncology Group Study. J Clin Oncol 3(9):1240–1245
Pautier P, Floquet A, Gladieff L, Bompas E, Ray-Coquard I, Piperno-Neumann S, Selle F, Guillemet C, Weber B, Largillier R, Bertucci F, Opinel P, Duffaud F, Reynaud-Bougnoux A, Delcambre C, Isambert N, Kerbrat P, Netter-Pinon G, Pinto N, Duvillard P, Haie-Meder C, Lhomme C, Rey A (2013) A randomized clinical trial of adjuvant chemotherapy with doxorubicin, ifosfamide, and cisplatin followed by radiotherapy versus radiotherapy alone in patients with localized uterine sarcomas (SARCGYN study). A study of the French Sarcoma Group. Ann Oncol 24(4):1099–1104. doi:10.1093/annonc/mds545
Pervaiz N, Colterjohn N, Farrokhyar F, Tozer R, Figueredo A, Ghert M (2008) A systematic meta-analysis of randomized controlled trials of adjuvant chemotherapy for localized resectable soft-tissue sarcoma. Cancer 113(3):573–581. doi:10.1002/cncr.23592
Amant F, De Knijf A, Van Calster B, Leunen K, Neven P, Berteloot P, Vergote I, Van Huffel S, Moerman P (2007) Clinical study investigating the role of lymphadenectomy, surgical castration and adjuvant hormonal treatment in endometrial stromal sarcoma. Br J Cancer 97(9):1194–1199. doi:10.1038/sj.bjc.6603986
Clayton Smith D, Kenneth Macdonald O, Gaffney DK (2008) The impact of adjuvant radiation therapy on survival in women with uterine carcinosarcoma. Radiother Oncol 88(2):227–232. doi:10.1016/j.radonc.2007.11.029
Wright JD, Seshan VE, Shah M, Schiff PB, Burke WM, Cohen CJ, Herzog TJ (2008) The role of radiation in improving survival for early-stage carcinosarcoma and leiomyosarcoma. Am J Obstet Gynecol 199(5):536.e1–8. doi:10.1016/j.ajog.2008.04.019
Wolfson AH, Brady MF, Rocereto T, Mannel RS, Lee YC, Futoran RJ, Cohn DE, Ioffe OB (2007) A gynecologic oncology group randomized phase III trial of whole abdominal irradiation (WAI) vs. cisplatin-ifosfamide and mesna (CIM) as post-surgical therapy in stage I–IV carcinosarcoma (CS) of the uterus. Gynecol Oncol 107(2):177–185. doi:10.1016/j.ygyno.2007.07.070
Wolfson AH, Wolfson DJ, Sittler SY, Breton L, Markoe AM, Schwade JG, Houdek PV, Averette HE, Sevin BU, Penalver M et al (1994) A multivariate analysis of clinicopathologic factors for predicting outcome in uterine sarcomas. Gynecol Oncol 52(1):56–62
Olah KS, Gee H, Blunt S, Dunn JA, Kelly K, Chan KK (1991) Retrospective analysis of 318 cases of uterine sarcoma. Eur J Cancer 27(9):1095–1099
Kokawa K, Nishiyama K, Ikeuchi M, Ihara Y, Akamatsu N, Enomoto T, Ishiko O, Motoyama S, Fujii S, Umesaki N (2006) Clinical outcomes of uterine sarcomas: results from 14 years worth of experience in the Kinki district in Japan (1990–2003). Int J Gynecol Cancer 16(3):1358–1363. doi:10.1111/j.1525-1438.2006.00536.x
Peters WA 3rd, Kumar NB, Fleming WP, Morley GW (1984) Prognostic features of sarcomas and mixed tumors of the endometrium. Obstet Gynecol 63(4):550–556
Park JY, Kim DY, Suh DS, Kim JH, Kim YM, Kim YT, Nam JH (2008) Prognostic factors and treatment outcomes of patients with uterine sarcoma: analysis of 127 patients at a single institution, 1989–2007. J Cancer Res Clin Oncol 134(12):1277–1287. doi:10.1007/s00432-008-0422-2
D’Angelo E, Spagnoli LG, Prat J (2009) Comparative clinicopathologic and immunohistochemical analysis of uterine sarcomas diagnosed using the World Health Organization classification system. Hum Pathol 40(11):1571–1585. doi:10.1016/j.humpath.2009.03.018
Denschlag D, Masoud I, Stanimir G, Gilbert L (2007) Prognostic factors and outcome in women with uterine sarcoma. Eur J Surg Oncol 33(1):91–95. doi:10.1016/j.ejso.2006.11.012
Nordal RR, Kristensen GB, Kaern J, Stenwig AE, Pettersen EO, Trope CG (1996) The prognostic significance of surgery, tumor size, malignancy grade, menopausal status, and DNA ploidy in endometrial stromal sarcoma. Gynecol Oncol 62(2):254–259. doi:10.1006/gyno.1996.0224
Chan JK, Kawar NM, Shin JY, Osann K, Chen LM, Powell CB, Kapp DS (2008) Endometrial stromal sarcoma: a population-based analysis. Br J Cancer 99(8):1210–1215. doi:10.1038/sj.bjc.6604527
Blom R, Malmstrom H, Guerrieri C (1999) Endometrial stromal sarcoma of the uterus: a clinicopathologic, DNA flow cytometric, p53, and mdm-2 analysis of 17 cases. Int J Gynecol Cancer 9(2):98–104
Abeler VM, Royne O, Thoresen S, Danielsen HE, Nesland JM, Kristensen GB (2009) Uterine sarcomas in Norway. A histopathological and prognostic survey of a total population from 1970 to 2000 including 419 patients. Histopathology 54(3):355–364. doi:10.1111/j.1365-2559.2009.03231.x
Ferguson SE, Tornos C, Hummer A, Barakat RR, Soslow RA (2007) Prognostic features of surgical stage I uterine carcinosarcoma. Am J Surg Pathol 31(11):1653–1661. doi:10.1097/PAS.0b013e3181161ba3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Burghaus, S., Halmen, S., Gass, P. et al. Outcome and prognosis in uterine sarcoma and malignant mixed Mullerian tumor. Arch Gynecol Obstet 294, 343–351 (2016). https://doi.org/10.1007/s00404-015-3993-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3993-6