Abstract
Purpose
To compare the subjective and objective cure rates, postoperative pain, postoperative complications, and postoperative quality of life of adjustable single-incision sling (Ajust®) versus tension-free vaginal tape-obturator (TVT-O™) in the treatment of female stress urinary incontinence (SUI).
Methods
Female patients with SUI (N = 368) were randomized to receive either Ajust® (N = 184) or TVT-O™ procedure (N = 184) between January 2012 and October 2013. Efficacy was evaluated using cure rate, postoperative complications, postoperative pain profile (using Visual Analogue Scale), Patient Global Impression of Improvement Scale, and International Consultation on Incontinence Questionnaire-Short Form.
Results
The patients from Ajust® and TVT-O™ groups had no statistically significant difference in subjective and objective cure rates (94.4 vs 90.7 %, P = 0.171; 97.2 vs 90.7 %, P = 0.195). Compared with the TVT-O™ group, patients in the Ajust® group had significantly less postoperative pain, shorter operative duration, and less intraoperative blood loss (all P values < 0.05). No significant difference in perioperative complications was observed between these two groups. Patients in Ajust® group had shorter recovery time (P < 0.001) compared to TVT-O™ group. The postoperative quality of life of patients in these two groups was significantly improved compared to baseline; however, no significant difference was observed in the average improvement of life between these two groups (P = 0.115).
Conclusions
Ajust® procedure is simple, safe, and effective for the treatment of SUI. Compared with TVT-O™, patients receiving Ajust® had less intraoperative blood loss, less postoperative pain, and shorter recovery time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress urinary incontinence (SUI) is the most common type of urinary incontinence in perimenopause women, with an incidence as high as 50 % [1]. The symptoms of SUI include leakage of urine at cough, sneeze, or even during walk or recumbent, which seriously affect a woman’s daily life and mental health.
Therapy for SUI includes physical and surgical treatments. Conservative treatment includes pelvic floor muscle training (PFMT) and biofeedback and electrical stimulation. Recent studies [2] have suggested that early surgical treatment is superior to physical treatment alone. Currently, the surgical treatment for SUI is more common, and had shown good curative effects. The most common procedure for surgical treatment of SUI is the standard mid-urethral slings (SMUS), including retropubic tension-free vaginal tape (RP-TVT) and transobturator tension-free vaginal tape (TO-TVT) [3–5]. The main complication of RP-TVT is the intraoperative bladder injury, and the main concern of TO-TVT is the postoperative pain in the inner thigh.
Introduction of minimally invasive mid-urethral slings has changed the surgical approach of SUI [6]. Adjustable single-incision sling (Ajust®) procedure is a more advanced surgical approach for the treatment of SUI. The sling is a non-absorbable polypropylene material with a width about 1.2 cm. The sling is inserted through a single incision in the anterior vaginal wall and suspends the middle part of urethra; the sling is anchored in the obturator membrane using anchoring device. The tightness of the sling is adjusted intraoperatively to obtain appropriate tension. The advantages of this approach include minimal injury, good tolerance, and shorter operative time. The other advantages are as follows: The surgery can be performed under local anesthesia, and the sling can be fixed firmly, with low incidence of postoperative pain, short hospital stay, and rapid recovery [7]. The present study was aimed to compare the subjective and objective cure rates, postoperative pain, postoperative complications, and postoperative quality of life after the surgical treatment of female SUI by Ajust® versus tension-free vaginal tape-obturator (TVT-O™).
Patients and methods
Study design
This prospective study included 368 patients undergoing simple surgery for SUI in the ward of pelvic disease of Gynaecology Department in Shengjing Hospital between January 2012 and October 2013. The patients were simply randomized using table of random numbers, and they received Ajust® (Bard) procedure or TVT-O™ (Johnson & Johnson) procedure; patients were followed up for 12 months. The study protocol was approved by the ethical committee of our hospital. All patients provided a written informed consent.
All surgeons were highly experienced and had performed more than 200 surgeries of TVT-O™ and more than 20 surgeries of Ajust® individually.
Patients
Study inclusion criteria were as follows: Patients with body mass index (BMI) < 35 kg/m2 and age > 18 years; patients with corresponding clinical symptoms (leakage of urine at cough and sneeze) and urodynamically diagnosed with SUI; and patients who received PFMT but failed to achieve efficacy or patients refused to receive PFMT (ineffective conservative therapy).
Study exclusion criteria were as follows: Patients with Pelvic Organ Prolapse Quantification score ≥ 2; patients with history of urinary incontinence surgery (such as Burch surgery and mid-urethral sling surgery) or history of pelvic irradiation; patients with mixed incontinence (SUI < urge urinary incontinence); patients who received prolapse therapy; and patients with disseminated sclerosis and other neurologic diseases.
Preoperative assessment
Preoperative assessment included patients’ medical history, pelvic examination, urodynamic assessment, 3-day urinary diary, and International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF).
Postoperative assessment
Visual analog scale (VAS) was used to measure the patients’ pain at 1 day, 1 week, 2 weeks, and 1 month after the surgery, where a VAS > 5/10 was considered severe pain. The bladder catheter was pulled out 24 h after surgery, and patients were asked to train for voluntary micturition; bladder scan (BladderScan® BVI9400; Verathon) was used to test the post-void residual volume (PVRV). In this study, a PVRV > 100 ml at 24 h after the surgery was considered urinary retention.
One year after the surgery, patients who had undergone standing cough stress test were guided to complete the Patient Global Impression of Improvement (PGI-I) and ICIQ-SF scales. In the PGI-I scale, patients with significant improvement or improvement in urinary incontinence were considered as “subjective cure.” Scale filling and VAS measurement were conducted by trained professionals, and they were blinded to the surgical approaches. The intraoperative blood loss was estimated by weighing the gauze pre- and post-operatively, together with the measurement of the amount of blood in the aspirator.
Surgical approaches
Ajust procedure
Normal saline was injected through anterior vaginal wall. Then the anterior vaginal wall was dissected longitudinally between inferior urethra and urethral lower ditch, and bilaterally dissected in urethral space till obturator. Along the tunnel on the right side created by previous dissection, the fixed anchor was passed behind the ischium pubic ramus before being pivoted through the obturator internus muscle and membrane by rotating the handle towards the obturator internus muscle to basically align the sling mid-line marker and middle urethra. The anchor was then released by pushing the release lever, the inducer was retracted, and gentle sling traction was applied to test for the quality of anchoring. The adjustable anchor was then introduced in the contralateral side in the same manner as described previously and the sling was adjusted. A flexible probe was inserted into the handle, and the sling lock was pushed to the adjustable anchor. Then the probe was removed, and the excessive mesh was cut off. The anterior vaginal incision was continuously sutured using 2–0 absorbable strands. After confirming no active bleeding, vagina was filled with two pieces of Anerdian gauzes, which were removed 24 h later.
TVT-O™ procedure
Normal saline was injected through anterior vaginal mucosa. Then the anterior vaginal wall was disserted longitudinally between inferior urethra to urethral lower ditch, and bilaterally dissected in urethral space till obturator. The left sling was inserted under the guidance of inducer, whose outlet was located about 3 cm parallel to and 1 cm below the urethra. The right sling was inserted in the same manner, and the sling was adjusted. Anterior vaginal wall was continuously sutured using absorbable strands. Then the puncture incision was also sutured, and two pieces of Anerdian gauzes were filled into vagina, which were removed 24 h later.
The primary endpoint was the subjective cure (defined as “very much improved” or “much improved” on the PGI-I scale) at 12 months after surgery.
The secondary endpoints were as follows: Objective cure (negative stress test: If there is no leakage of urine during the involuntary cough, the test is negative, indicating an objective cure.) at 12 months after surgery; PVRV at 24 h after surgery; VAS scores at 1 day, 1, 2, and 4 weeks after surgery; and surgery data and perioperative complications.
Sample size and statistical analysis
It was intended to enroll a total of 360 patients in this study. An estimated subjective cure rate of 80 % in the TVT-O group might obtain a difference of 10 % or above between the two groups with a certainty of 80 % (β = 0.2), α = 0.05.
Statistical analysis was performed using SPSS19.0 software. Measurement data analyses were performed using t test, and count data analyses were performed using Chi square test, where P < 0.05 was considered statistically significant.
Result
General characteristics of patients
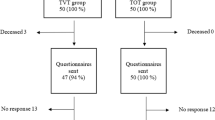
A total of 534 patients were recruited in this study, and 368 patients with SUI who met the inclusion criteria were randomized into two groups, namely, Ajust® (N = 184) and TVT-O™ (N = 184) procedures (Fig. 1). Patients in the two groups had no statistically significant differences in age, BMI, daily urinal pad, duration of SUI, preoperative PVRV, hormone replacement therapy, history of hysterectomy, smoking, and other baseline data, as shown in Table 1.
Primary endpoint
All patients received 12 months’ follow-up, and the patients from Ajust® and TVT-O™ groups had no statistically significant difference in the subjective cure rate (94.4 vs 90.7 %, P = 0.171), as shown in Table 2.
Secondary endpoint
In the 12 months’ follow-up, the patients from Ajust® and TVT-O™ groups had no statistically significant difference in the objective cure rate (97.2 vs 90.7 %, P = 0.195).
PVRV was measured at 24 h after the surgery, and the results showed that the Ajust® and TVT-O™ groups had no statistically significant difference in the objective cure rate (57.2 ± 23.2 vs 54.4 ± 30.7, P = 0.324).
Incidence of severe pain (VAS > 5/10) at 24 h after surgery in the Ajust® group was significantly lower than that in the TVT-O™ group (1.1 vs 4.9 %, P = 0.032).
Patients in the Ajust® group had shortening trend of postoperative hospital stay compared with the TVT-O™ group (P = 0.216), and had significantly shorter time to restore normal life (14.84 ± 1.17 vs 9.89 ± 1.26, P = 0.000).
In the 12 months’ follow-up, the average improvement in the Ajust® and TVT-O™ groups had no statistical significant difference (3.20 ± 5.43 vs 12.35 ± 4.87, P = 0.115), as shown in Table 2.
Postoperative pain was tested at 1 day, 1 week, 2 weeks, and 1 month after the surgery, and the results showed that the pain within 2 weeks after the surgery in the Ajust® group was significantly lower than the TVT-O™ group, and the pain in the two groups basically disappeared 1 month after surgery, with no statistically significant difference (Fig. 2; Table 3).
Intraoperative state and perioperative complications
Compared with the TVT-O™ group, the patients in Ajust® group had significantly shorter operative time (14.4 ± 7.8 vs 25.2 ± 8.6, P < 0.001) and had significantly smaller amount of intraoperative blood loss (14.6 ± 2.6 vs 22.3 ± 1.7, P < 0.001). No significant intraoperative and postoperative complications were found in the two groups and no bladder, vessel, and nerve damages were found after surgery. Urinal catheter was removed 24 h after surgery in both groups, and four and ten patients had urinary retention, respectively, from Ajust® and TVT-O™ groups; they required indwelling bladder catheter. One month after the surgery, the patients’ PVRV restored to normal level and they did not require self-catheterization. Three patients in the TVT-O™ group had vaginal sling erosion and they underwent surgery for partial removal, as shown in Table 4.
Discussion
The present study results suggested that compared with the TVT-O™ group, patients receiving Ajust® surgical approach had significantly less pain, shorter operating time, smaller amount of blood loss, and shorter recovery time.
Postoperative subjective and objective cure rates
Retrospective study on RP-TVT and TO-TVT as well as meta-analysis did not confirm that there were significant differences in the subjective and objective cure rates between the two groups [8, 9]. However, RP-TVT was more likely to damage bladder, leading to postoperative voiding dysfunction. Meanwhile, the incidence of postoperative pain in the inguinal region and in thigh was significantly increased after TO-TVT surgery.
Numerous studies on short-term follow-up showed that the objective cure rate at 3 months after Ajust surgery was 89.7 % [10], and those at six and 12 postoperative months were 91.4 % [11] and 82–86 % [7, 12], respectively. In Nauman et al. [6] study, patients with SUI (N = 52) received Ajust® surgery and 29 months’ follow-up. The results showed that the postoperative objective cure rate was 86.3 %, patient’s quality of life was significantly improved, and good long-term efficacy was achieved. Tantanasis et al. [13] reviewed the surgical techniques, with long-term success rates ranging from 84 to 95 %.
Postoperative pain
The present study results indicated that compared with TVT-O, patients receiving Ajust procedure had less postoperative pain within 2 weeks, and they might require less recovery time to perform activity and restore normal life. These results were consistent with previous study results [7, 8, 11, 12, 14–17]. In TVT-O surgical approach, postoperative pain was severe, long-lasting, covering large area, and often accompanied by pain in lower limbs, which was further aggravated during activity of lower limbs. It was suspected that the pain could be associated with the adductor tendon injury. Interestingly, in Ajust procedure, the postoperative pain was mild, short-lasting, and the recovery time was shorter compared to TVT-O. It was speculated that the less pain might be due to limited puncture was made only in obturator membrane without any penetrations in obturator internus, leading to no tendon injury. In a multicentre prospective study [10], patients with SUI (N = 137) were randomized to receive Ajust (N = 69) or TVT-O (N = 68) procedures, and the follow-up results showed that the postoperative pain in Ajust group was significantly lower than the TVT-O group within 4 weeks after the surgery.
Postoperative quality of life
Patients receiving Ajust procedure had significantly shorter time to restore their normal life. Multicenter prospective large sample studies [6, 10, 11] indicated that Ajust surgery can significantly improve quality of life of patients. In the present study, the ICIQ-SF survey suggested that the quality of life of patients in the two groups were both significantly improved.
Postoperative urination and sling exposure
The present study showed that the incidence of urinary retention in the Ajust group was lower than the TVT-O group; however, the difference was not statistically significant (P > 0.05). A total of 14 patients in the two groups had PVRV > 100 ml at postoperative day 1, and they used indwelling catheter for a duration of 1–14 days; the patients’ PVRV reached the normal level at 4 weeks after the surgery. In Mostafa et al. [10] study, it was reported that the incidence of catheterization requirement in postoperative period in the Ajust group was 4.3 %, which was comparable with the present study results. In Meschin et al. [11] study, one patient had urinary retention at 9 days after the Ajust surgery, and then the sling was removed; 151 patients were followed up for 6 months in another study [18]. Ten patients (6.1 %) had de novo urge incontinence in their post-operative follow-ups which was resolved using anti-cholinergic drugs and two patients (1.2 %) required sling sections due to prolonged bladder outlet obstruction. In previous studies, more attention has been paid to tightness of sling, which is no objective indicator and is mostly associated with the experience of surgeons and training of surgical approach. In the present study, it was found that although the sling tightness was different, postoperative subjective and objective cure rates were not significantly different between the two treatment groups. Based on our operation experience and postoperative outcomes we found that a sling position in SUI surgical approach could affect the outcome, likely, sling position too close to the external urethral orifice might result in postoperative urinary retention and urinary thinning, while a sling position too far from the external urethral orifice might lead to failure of continence surgery and leakage of urine. Hence, it is believed that the core success of surgery is dependent on sling position rather than its tightness, and the use of too tight a sling should be avoided. The incidence of postoperative vaginal sling erosion had no statistically significant difference between the two groups, but was significantly lower than the results previously reported in early type SIMS [19, 20].
Limitation of the study
The major limitations in this study were intraoperative use of epidural anesthesia and use of normal saline for hydrodissection. Moreover, the follow-up duration was short (1 year).
Conclusion
Ajust® procedure is simple, safe, and effective for the treatment of SUI. Compared with TVT-O™, patients receiving Ajust® had less intraoperative blood loss, less postoperative pain, and shorter recovery time. However, the efficacy of Ajust® surgical approach needs to be further verified using multicenter, large sample, and long-term follow-up studies.
References
Abrams P, Artibani W, Cardozo L, Khoury S, Wein A (2005) Clinical manual of incontinence in women, 21st edn. Health Publisher Ltd., Paris
Labrie J, Berghmans BL, Fischer K, Milani AL, van der Wijk I, Smalbraak DJ, Vollebregt A, Schellart RP, Graziosi GC, van der Ploeg JM, Brouns JF, Tiersma ES, Groenendijk AG, Scholten P, Mol BW, Blokhuis EE, Adriaanse AH, Schram A, Roovers JP, Lagro-Janssen AL, van der Vaart CH (2013) Surgery versus physiotherapy for stress urinary incontinence. New Engl J Med 369(12):1124–1133. doi:10.1056/NEJMoa1210627
Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 7(2):81–85 discussion 85–86
Delorme E (2001) Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Progres en urologie : journal de l’Association francaise d’urologie et de la Societe francaise d’urologie 11(6):1306–1313
de Leval J (2003) Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol 44(6):724–730
Naumann G, Hagemeier T, Zachmann S, Al-Ani A, Albrich S, Skala C, Laterza R, Linaberry M, Koelbl H (2013) Long-term outcomes of the ajust adjustable single-incision sling for the treatment of stress urinary incontinence. Int Urogynecol J 24(2):231–239. doi:10.1007/s00192-012-1843-7
Abdel-Fattah M, Agur W, Abdel-All M, Guerrero K, Allam M, Mackintosh A, Mostafa A, Yousef M (2012) Prospective multi-centre study of adjustable single-incision mini-sling (Ajust((R))) in the management of stress urinary incontinence in women: 1-year follow-up study. BJU Int 109(6):880–886. doi:10.1111/j.1464-410X.2011.10471.x
Novara G, Artibani W, Barber MD, Chapple CR, Costantini E, Ficarra V, Hilton P, Nilsson CG, Waltregny D (2010) Updated systematic review and meta-analysis of the comparative data on colposuspensions, pubovaginal slings, and midurethral tapes in the surgical treatment of female stress urinary incontinence. Eur Urol 58(2):218–238. doi:10.1016/j.eururo.2010.04.022
Ogah J, Cody DJ, Rogerson L (2011) Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women: a short version Cochrane review. Neurourol Urodyn 30(3):284–291. doi:10.1002/nau.20980
Mostafa A, Agur W, Abdel-All M, Guerrero K, Allam M, Lim C, Yousef M, Abdel-Fattah M (2012) A multicentre prospective randomised study of single-incision mini-sling (Ajust(®)) versus tension-free vaginal tape-obturator (TVT-O™) in the management of female stress urinary incontinence: pain profile and short-term outcomes. Eur J Obstet Gynecol Reprod Biol 165(1):115–121
Meschia M, Barbacini P, Baccichet R, Buonaguidi A, Maffiolini M, Ricci L, Braghin C, Brusati V, Dell’Utri C, Spreafico L (2011) Short-term outcomes with the Ajust system: a new single incision sling for the treatment of stress urinary incontinence. Int Urogynecol J 22(2):177–182. doi:10.1007/s00192-010-1254-6
Cornu J, Ciofu C, Sebe P, Peyrat L, Haab F (2011) Cure of women stress urinary incontinence with the Ajust single-incision sling: one year results. Neurourol Urodyn 30(6):787–1195
Tantanasis T, Daniilidis A, Pantelis A, Chatzis P, Vrachnis N (2013) Minimally invasive techniques for female stress urinary incontinence, how, why, when. Arch Gynecol Obstet 288(5):995–1001. doi:10.1007/s00404-013-3024-4
Wang YJ, Li FP, Wang Q, Yang S, Cai XG, Chen YH (2011) Comparison of three mid-urethral tension-free tapes (TVT, TVT-O, and TVT-Secur) in the treatment of female stress urinary incontinence: 1-year follow-up. Int Urogynecol J 22(11):1369–1374. doi:10.1007/s00192-011-1445-9
Abdel-Fattah M, Ramsay I, Pringle S, Hardwick C, Ali H, Young D, Mostafa A (2010) Randomised prospective single-blinded study comparing ‘inside-out’ versus ‘outside-in’ transobturator tapes in the management of urodynamic stress incontinence: 1-year outcomes from the E-TOT study. BJOG: Int J Obstet Gynaecol 117(7):870–878. doi:10.1111/j.1471-0528.2010.02544.x
Liapis A, Georgantopoulou C, Bakas P (2010) Short term results of the Ajust adjustable single incision sling procedure for the treatment of urodynamic stress urinary incontinence. Int Urogynecol J 21:S1–428
Naumann G, Hagemeier T, Zachmann S (2010) AjustTM fully adjustable single incision sling for the treatment of stress urinary incontinence: 1 year follow-up on a new minimal-invasive treatment for female SUI. Int Urogynecol J 21:S1–428
Taner CE, Okay G, Goklu Y, Basogul O, Basogul N (2015) Perioperative and postoperative complications after Ophira mini sling operations. Arch Gynecol Obstet 291(2):341–346. doi:10.1007/s00404-014-3402-6
Hinoul P, Vervest HA, den Boon J, Venema PL, Lakeman MM, Milani AL, Roovers JP (2011) A randomized, controlled trial comparing an innovative single incision sling with an established transobturator sling to treat female stress urinary incontinence. J Urol 185(4):1356–1362. doi:10.1016/j.juro.2010.11.083
Basu M, Duckett J (2010) A randomised trial of a retropubic tension-free vaginal tape versus a mini-sling for stress incontinence. BJOG: Int J Obstet Gynaecol 117(6):730–735. doi:10.1111/j.1471-0528.2010.02513.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Xin, X., Song, Y. & Xia, Z. A comparison between adjustable single-incision sling and tension-free vaginal tape-obturator in treating stress urinary incontinence. Arch Gynecol Obstet 293, 457–463 (2016). https://doi.org/10.1007/s00404-015-3949-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3949-x