Abstract
Purpose
Often breast cancer can be treated by breast-conserving surgery (BCS), after which 10 % locoregional recurrences (LRR) occur within 10 years. After BCS mastectomy is recommended at first LRR, although another BCS could be possible. Changes in clinical parameters and in tumor biology from primary breast cancer to first and multiple LRR are described and correlated with further LRR and overall survival (OS).
Methods
380 patients with ≥1 ≤3 LRR (1997–2007) were evaluated retrospectively and followed until 5/2009. Patients’ age, tumor size, nodal involvement, distant metastases, histological subtype, hormone receptor (HR) and Her-2/neu status were assessed. LRR therapy options were evaluated.
Results
247 patients had one LRR (94 two and 39 three). Mean OS was 10.1 years. Number of LRR was not correlated with OS. Positive HR status was significantly correlated with longer OS. Patients, who changed from primarily ER negative to positive at first LRR had a significantly longer OS compared to those, who remained or changed to ER negative (p < 0.01). Tumor size and grading correlated inversely with OS (both: p < 0.001). BCS at first LRR correlated with a significantly better OS than mastectomy (p < 0.001). LRR cases with chemotherapy had a shorter OS. Irradiation and/or endocrine therapy after LRR were not correlated with OS.
Conclusions
Patients with positive HR status had the best survival data. HR should always be determined. In positive cases, endocrine therapy is recommended. As clinical data are good, BCS at first LRR can be suggested for more patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common malignancy in women. One in eight to ten women is affected throughout her life. The median age of first diagnosis is 65 years [1]. Often breast-conserving therapy is standard of care in the western world. It combines breast-conserving surgery (BCS) followed by irradiation of the breast. Today, approximately 70 % of patients with primary breast cancer can be treated breast conserving [2].
After breast-conserving therapy approximately 10 % of patients suffer from locoregional recurrence (LRR) of breast cancer within 10 years, after mastectomy the number of recurrences is 4 %. If the tumor reappears in the ipsilateral breast or chest wall it is called a local recurrence, if it is localized in the axilla, supra-/infraclavicular lymph nodes or along the mammaria interna lymph nodes it is defined as regional recurrence [3, 4]. 5-year survival is 65 % for patients with a relapse after breast-conserving therapy and 50 % after mastectomy. In case of recurrence 20 % of patients have already developed distant metastases [4–6].
Several risk factors at the time of first diagnosis of the primary tumor are known for a later recurrence. These are especially young age, non-in sano resection of the tumor, negative hormone receptor status, poorly differentiated tumors, tumor size (>2 cm), and affected lymph nodes [7, 8]. Omission of endocrine therapy in case of positive hormone receptors or the lack of radiation after BCS is also contributing factors for relapse [7]. In case of a locoregional recurrence (LRR) tumor size, multifocality and tumor localization influence the risk of another relapse [9].
Treatment of LRR is similar to first-line therapy; corresponding guidelines have been developed by the German “Arbeitsgemeinschaft Gynäkologische Onkologie (AGO)”. After initial breast-conserving therapy the recommended surgical therapy at LRR is mastectomy, most likely achieving the goal of R0-resection. If tumor-free margins are likely to be gained by another breast-conserving approach, this option can be chosen, too. In this setting a sentinel lymph node biopsy can be performed again, if the patient appears clinically free of metastases. Alternatively, an axillary dissection should be conducted in case of clinically positive lymph nodes. If primary surgery was mastectomy, R0-resection is intended [9–11].
For further local treatment a radiation therapy of the whole breast is recommended after re-BCS, if no adjuvant irradiation has been done at first diagnosis. Otherwise, a different form of irradiation, a partial breast irradiation, can be performed. If mastectomy was performed at relapse, chest wall radiation can be discussed. In case of chest wall resection after mastectomy local radiation is reasonable, if no radiation has been done in the first place [12].
For systemic therapy in the situation of recurrence the preferential option is endocrine therapy for hormone receptor-positive tumors. Otherwise, especially in case of receptor-negative tumors, chemotherapy is recommended, combined with Her2-neu targeting agents if indicated [13].
In this study, we followed the course of disease of breast cancer patients with one or more LRR. Changes in clinical parameters and in tumor biology from primary breast cancer to first and multiple LRR are described. Predictive factors at first recurrence for further LRR, tumor burden at last follow-up and for breast cancer-related death were investigated and therapy options at first LRR were evaluated. As surgical strategies after first LRR had been diverse, we examine potential differences between mastectomy and a second breast conserving approach in regards to further course of disease and overall survival.
Methods
The present study is based on a retrospective analysis of medical records of a major Breast Unit at a University Hospital in Germany. All 380 patients with at least one event of recurrence of breast cancer between 01.01.1997 and 31.12.2007 were enrolled in the study. As in some cases multiple recurrences occurred, a total of 552 cases were analyzed. The patients were followed up until May 2009.
The data assessed for each patient are based on a patient’s enquiry as well as on saved medical records. Age at diagnosis, tumor size, nodal involvement, distant metastases, histological subtype, hormone- und Her2-neu receptor status, therapies conducted and time to recurrence were assessed. This information was determined for all primary tumors and each case of recurrence. Patients with up to three recurrences were considered for the trial.
This study was approved by the local Review Board (AZ# D450/10). All patients gave their written informed consent for this study participation.
Ordinally and nominally scaled values were displayed in absolute and percent frequencies. Two of each of these values were compared in contingency tables and tested for dependence or correlation using the Chi-square test. If the expected frequencies turned out to be too small, the exact test according to Fisher was used. Odds ratios were calculated to quantify the effect of influencing factors.
Overall survival was analysed by the method of Kaplan–Meier and log rank statistics. The tests were performed two sided with a significance level of 5 %. An alpha adjustment for multiple testing was not applied, and the results were interpreted accordingly in an exploratory way. Statistical calculations were done with SPSS Statistics 22 (SPSS Inc. an IBM Company, Chicago, IL).
Results
Patient characteristics
We investigated the course of disease of 380 patients aged 25–91 years with a median age of 54 years at first diagnosis. All of the patients had at least one recurrence of breast cancer. For 247 (65.0 %) patients this first relapse was the only one during the time of observation (35 years), 94 (24.7 %) suffered a second relapse and 39 (10.3 %) sustained a third. Patients and tumor characteristics at primary diagnosis and each case of recurrence are summarized in Table 1. Furthermore, we displayed the applied therapies at different stages of disease (Table 1).
Follow-up data were available for 359 patients. Out of these patients, 260 (72.4 %) patients were still alive at last contact and 99 (27.6 %) have died. The mean overall survival time was 10.1 years. From the patients, who died over the course of disease, 59 suffered from one recurrence, 28 patients had a second one and 12 patients relapsed for a third time. Time from first diagnosis to first LRR was 5.7 years, from first diagnosis to second LRR 9.2 years and to third relapse 10.4 years. A significant correlation between the number of relapses and overall survival could not be shown (p > 0.05).
Change of hormone receptor status over the course of disease
Exemplarily for the tumor features and their development over the course of disease, we took a distinct look at the change of hormone receptor status from first diagnosis to third relapse. A slight increase of estrogen receptor (ER)-positive tumors was observed. Initially 156 (67.5 %) patients had a positive ER expression, whereas 75 (32.5 %) were ER negative. At the time of first recurrence hormone receptor status was assessed in 292 women and the number and percentage of ER positive patients increased to 206 (70.5 %) with 86 (29.5 %) patients being ER negative. Further increase of positive expression could be observed at second recurrence with 70 (75.3 %) ER positive and 23 (24.7 %) ER negative patients. This proportion remained stable at third relapse (Table 1). Contrarily, the proportion of progesterone receptor (PR)-positive patients decreased over the course of events compared to negative PR expression. Only from second to third relapse the percentage of PR-positive tumors increased slightly (Table 1).
At the time of first relapse 40 (20.7 %) tumors changed their ER expression from either negative to positive (37.5 %) or positive to negative (62.5 %), 153 (79.3 %) tumors had a stable ER expression (positive 72.5 %, negative 27.5 %). For second relapse 7 (10.2 %) tumors changed from either ER negative to positive (71.4 %) or positive to negative (28.6 %), whereas 62 (89.8 %) tumors had a stable ER expression (positive 72.6 %, negative 27.4 %). At third recurrence 5 (23.8 %) tumors changed ER expression from negative to positive (20.0 %) or the other way around (80.0 %), 16 (76.2 %) tumors had a stable expression (positive 82.2 %, negative 18.8 %). Similar results were assessed for PR expression (Table 2).
A change of hormone receptor status was significantly correlated with overall survival (OS). Patients, who changed from ER negative to ER positive or who kept positive ER from first diagnosis to first recurrence had a significantly longer OS than those, who either stayed negative or changed from positive to negative ER (p < 0.01). For the time from second to third recurrence, patients who stayed ER positive had the longest survival and those who changed from negative ER to positive ER died earliest (p < 0.01). With regard on PR expression, LRR patients with stable positive PR showed the longest, those with unchanged negative PR the shortest OS. PR change from negative to positive had a longer OS than from positive to negative (p < 0.01).
Correlation between markers at first LRR and number of LRR
We investigated the correlation between tumor biology at first LRR and the number of further recurrences. No significant results were obtained. Furthermore, none of the applied therapies correlated significantly with the number of LRR. We put special regard on differences in surgical therapy at first relapse. Neither BCS nor mastectomy showed significant correlation with further LRR (p > 0.05). Similarly, neither the application of chemotherapy nor radiation therapy of the breast or chest wall correlated significantly with further course of disease. In conclusion, neither tumor characteristics nor any therapy options at time of first relapse influenced the number of further LRR (data not shown).
Correlation between markers at first LRR and tumor burden at last follow-up
Several tumor characteristics at first recurrence were significantly associated with tumor load at last follow-up. The absence of any tumor tissue was predicted by lobular histological subtype (p < 0.001), small tumor size (p < 0.001), favorable grading (p = 0.012) and recurrence being localized within the breast after BCS at first diagnosis (p < 0.001). Additionally the chance of tumor-free status at last follow-up was significantly higher without nodal involvement (p < 0.001), lack of distant metastases (p < 0.001) and positive ER status (p = 0.016). No significant correlation was shown for PR- and Her2-neu status (Table 3).
Regarding the therapy administered, the application of chemotherapy at time of first LRR correlated significantly with higher tumor load at last follow-up compared to patients treated without chemotherapy (p < 0.001). A significant association was also shown for the type of surgery (p < 0.001); the chance to be tumor free at last follow-up was significantly higher after ablative surgery compared to chest wall revision and was highest after BCS. No significant correlation was shown for irradiation, endocrine therapy and trastuzumab (Table 3).
Correlation between markers at first LRR and overall survival
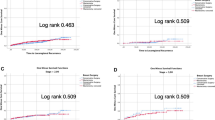
A number of tumor features at first LRR showed significant association with OS (Table 4). Tumor size and grading correlated inversely with OS (both: p < 0.001). Accordingly, patients without distant metastases lived significantly longer compared to those with spread disease (p < 0.001). Positive ER and PR status both showed significant correlation with longer OS [ER: p = 0.001 (Fig. 1); PR: p = 0.017 (Fig. 2)]. Nodal positive patients on the other hand showed longer OS as well (p = 0.012). Histological subtype, specific localization of LRR and Her2-neu status were not significantly correlated with OS (Table 4).
Taking a look at therapy options and OS, the choice of surgery showed significant correlation (p < 0.001). BCS at first LRR had an unimpaired survival of 100 % after 5 years, mastectomy showed a 5 year survival time of 91.2 %, chest wall revision even less. Cases, in which the application of chemotherapy was indicated, were correlated with a significantly shorter OS (p < 0.001). Patients receiving trastuzumab lived significantly shorter compared to those without this targeted therapy (p = 0.014). No correlation was detected concerning irradiation and endocrine therapy (Table 4).
Discussion
Patient cohort and therapy in context
Each patient in this study experienced at least one locoregional breast cancer recurrence. In the study population a maximum of three LRR occured. The number of cases with more than three relapses was too small for statistical analysis. Therefore, a cutoff was set at three recurrences.
Patients were treated according to current national recommendations (AGO/Breast) or the German national S3 guideline [9, 14]. In this study we included patients with recurrences between 1997 and 2007; the diagnosis of primary breast cancer in most cases was even earlier. Therefore, diagnostic tools and applied therapies are partially different from today’s standard. In the late 1990s, e.g., hormone receptor and Her2-neu status were not assessed in all patients. Consequently, endocrine therapies were not prescribed routinely in patients with primary diagnosis in the early and mid-1990s. For HER2-neu-positive tumors targeted agents such as trastuzumab were not offered routinely until 2005. Overall, most patients had a long follow-up time. Only 21 patients were lost to follow-up.
Hormone receptor status over the course of disease
Percentage of hormone receptor-positive patients increased over the course of disease. At initial diagnosis 67.5 % were hormone receptor positive and 75.3 % at second relapse. An increase of negative receptor status might have been expected, as this is known as a risk factor and independent predictor for recurrence [15–17]. Patients with negative hormone receptor status probably died earlier in the course of events, whereas ER and PR-positive patients survived and lived longer to see further recurrence. 10–20 % of patients changed hormone receptor status at each case of relapse. Except of ER status at second recurrence, the tendency was clearly the change from positive to negative hormone receptor status. This again confirms that among other things a negative hormone receptor status is associated with LRR, possibly due to the missing employment of endocrine therapy [15–17].
The literature states, that negative ER and PR status are also associated with shorter OS [18]. Our data could confirm this. At the recurrent situation patients with either stable negative receptor status or change from positive to negative had a shorter OS time. Patients with positive hormone receptor status during the whole course of their disease, represent the group of patients with longest OS. Therefore, receptor status should be determined in each case of recurrence. In case of positive hormone receptor status an endocrine therapy should be initiated or altered, if an endocrine agent is still applied from the primary or previous disease [9].
Parameters at first LRR
In our analysis of tumor characteristics at first LRR, we found most of the known predictive markers in breast cancer patients being significantly correlated with tumor burden at last follow-up and with OS. Small tumor size, favorable grading, positive hormone receptor status and lack of distant metastases were associated with no tumor load at last follow-up and with longer OS. Patients with positive lymph node status showed more tumor burden at last follow-up, but also a longer OS. As a negative impact of nodal positivity on OS has been expected and has been previously reported [7], a positive correlation with a better OS appears somewhat contradictory. A possible explanation might be that OS is influenced by multiple factors. A small patient cohort of nodal positive patients at first LRR could result in invalid statistical results. Another explanation could be that nodal positive patients at first LRR received more aggressive local therapies, including a second surgery of the axilla and/or radiation of the locoregional lymph nodes. Also a selection bias for more and earlier aggressive forms of systemic therapies could have appeared in the group of nodal positive patients at first LRR. None of the parameters seemed to influence the course of disease in the sense of upcoming further recurrences.
Therapy at first LRR
The recommended surgical standard therapy of first LLR is mastectomy after breast-conserving therapy at initial treatment. A growing number of physicians offer the possibility of another breast-conserving approach. In our study neither BCS nor mastectomy at time of first LRR showed themselves predictive for further recurrences. This means, that ablative surgery was not superior to re-BCS on relation to OS. Furthermore, we could show that the chance to be free of tumor mass at last follow-up was greatest after re-BCS. Significantly more patients displayed tumor burden, when mastectomy or chest wall revision were performed. Additionally, the same applies for OS; patients after re-BCS at first LRR lived longest. This supports the approach of BCS at first recurrence being at least equal to mastectomy, if not superior. As this is a retrospective analysis and not a prospective, randomized trial, these results have to be handled with caution and should be validated in prospective clinical trials. The intention of each surgical procedure at LRR is the R0-resection. This can be assured at the highest level by mastectomy. BCS always bears the risk of positive tumor margins followed by either mastectomy or possibly reduced survival. BCS may also result in unsatisfying cosmetics and could limit local tumor control. Overall, patients demand for quality of life even with a malignant disease. This quality of life for women is often defined by feminine body awareness represented by two mammaries. Not every woman accepts the risk of multiple and extended surgeries of reconstruction by implants or homologue methods such as latissimus dorsi plastic or transverse rectus abdominis muscle plastic. Therefore, BCS followed by partial breast irradiation could be an option at first LRR [19]. Previous studies could not show an explicit benefit of chemotherapy at LRR. Only the CALOR study states an advantage of cytotoxic systemic therapy at LRR independent of hormone receptor status. 5-year survival was increased from 76 to 88 %. Therefore, chemotherapy was at least recommended at LRR for endocrine non-responsive tumors. Especially triple negative patients or patients with Her2-neu overexpression benefit from chemotherapy, combined with, e.g., trastuzumab if indicated [13]. Our study could not show any correlation between chemotherapy at first LRR and further recurrences. On the other hand the application of chemotherapy was correlated not only with higher tumor load at last follow-up, but also with shorter overall survival. This inverse correlation of chemotherapy with inferior survival data has to be interpreted as negative patient selection bias.
Endocrine therapy did not influence the course of disease significantly in this study. It has to be borne in mind that neither the assessment of hormone receptor status nor the application of endocrine agents was standard of care at times when follow-up of wide parts of this collective study started. Therefore, results have to be interpreted carefully and hormone receptor status should nevertheless be assessed at time of recurrence. If patients show hormone receptor-positive tumors at recurrence, endocrine agents should be prescribed [9].
Trastuzumab is indicated in LRR, if no Her2-neu targeting medication has been applied in the adjuvant setting. This study showed a shorter OS after application of trastuzumab at first LRR. In most cases no adjuvant therapy was applied despite aggressive tumor biology. It can be suspected that the employment of trastuzumab in an advanced course of disease is less effective. But we must also observe that only few patients received trastuzumab at all at first LRR and, therefore, numbers are too limited for further interpretation. The actual therapy recommendation should be followed [9].
One of the ways to estimate risk of tumor recurrence or progression in the adjuvant setting is the combination of clinical and tumor biological factors (e.g., grading, hormone receptor status and Her2-neu status). Sometimes also gene expression tests can be helpful for additional risk assessment. In selected cases they can help to make more individualized decisions on systemic therapies. So far, these gene signatures are only used in the adjuvant situation. We suggest to prospectively validate these gene signatures also for LRR, where they also could be helpful in selected cases.
In conclusion, our analysis shows that patients with continuous positive hormone receptor status over all their disease-affected lives represent the group of patients with longest OS. Therefore, receptor status should be determined at each time of LRR and endocrine therapy should be adjusted. We did not find any influential factors for further LRR, but could show several factors being predictive for tumor burden at last follow-up and for overall survival. In this context, therapy options at first LRR were evaluated and current standards could mainly be confirmed. Our data for surgical therapy at LRR encourage to treat more patients with BCS.
References
Robert-Koch-Institut, (Hrsg) (eds) (2013) Krebs in Deutschland 2009/2010, vol 9. Robert Koch-Institut und die Gesellschaft der epidemiologischen Krebsregister in Deutschland e.V, Berlin
Janni W (2005) Zertifizierte medizinische Fortbildung: Therapie des primären, invasiven Mammakarzinoms. Dtsch Ärztebl 102:S. A-2795/B-2360/C-2226
Smith TE, Lee D, Turner BC, Carter D, Haffty BG (2000) True recurrence vs. new primary ipsilateral breast tumor relapse: an analysis of clinical and pathologic differences and their implications in natural history, prognoses, and therapeutic management. Int J Radiat Oncol Biol Phys 48(5):1281–1289
Haffty BG, Fischer D, Beinfield M, McKhann C (1991) Prognosis following local recurrence in the conservatively treated breast cancer patient. Int J Radiat Oncol Biol Phys 21(2):293–298
Veronesi U, Marubini E, Del Vecchio M, Manzari A, Andreola S, Greco M, Luini A, Merson M, Saccozzi R, Rilke F et al (1995) Local recurrences and distant metastases after conservative breast cancer treatments: partly independent events. J Natl Cancer Inst 87(1):19–27
van der Hage JA, Mieog JS, van de Velde CJ, Putter H, Bartelink H, van de Vijver MJ (2011) Impact of established prognostic factors and molecular subtype in very young breast cancer patients: pooled analysis of four EORTC randomized controlled trials. Breast Cancer Res 13(3):R68. doi:10.1186/bcr2908bcr2908
Wapnir IL, Anderson SJ, Mamounas EP, Geyer CE Jr, Jeong JH, Tan-Chiu E, Fisher B, Wolmark N (2006) Prognosis after ipsilateral breast tumor recurrence and locoregional recurrences in five National Surgical Adjuvant Breast and Bowel Project node-positive adjuvant breast cancer trials. J Clin Oncol 24(13):2028–2037. doi:10.1200/JCO.2005.04.3273
Mirza NQ, Vlastos G, Meric F, Buchholz TA, Esnaola N, Singletary SE, Kuerer HM, Newman LA, Ames FC, Ross MI, Feig BW, Pollock RE, McNeese M, Strom E, Hunt KK (2002) Predictors of locoregional recurrence among patients with early-stage breast cancer treated with breast-conserving therapy. Ann Surg Oncol 9(3):256–265
Fehm T, Solomeyer E, Mundhenke C (2013) Diagnostik und Therapie primär und metastasierter Mammakarzinome—Loko-regionäres Rezidiv. Arbeitsgemeinschaft Gynäkologische Onkologie
Derkx F, Maaskant-Braat AJ, van der Sangen MJ, Nieuwenhuijzen GA, van de Poll-Franse LV, Roumen RM, Voogd AC (2010) Staging and management of axillary lymph nodes in patients with local recurrence in the breast or chest wall after a previous negative sentinel node procedure. Eur J Surg Oncol 36(7):646–651. doi:10.1016/j.ejso.2010.05.009
Taback B, Nguyen P, Hansen N, Edwards GK, Conway K, Giuliano AE (2006) Sentinel lymph node biopsy for local recurrence of breast cancer after breast-conserving therapy. Ann Surg Oncol 13(8):1099–1104. doi:10.1245/ASO.2006.08.026
Cardoso F, Harbeck N, Fallowfield L, Kyriakides S, Senkus E (2012) Locally recurrent or metastatic breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 23(Suppl 7):11–19. doi:10.1093/annonc/mds232
Aebi S GS, Lang I, Anderson SJ, Robidoux A, Martin M, Nortier JWR, Mamounas EP, Geyer, Jr. CE, Maibach R, Gelber RD, Wolmark N, Wapnir I (2012) Chemotherapy prolongs survival for isolated local or regional recurrence of breast cancer: The CALOR trial (Chemotherapy as adjuvant for locally recurrent breast cancer. NSABP Cancer Res 72(24):156–163
Kreienberg R, (Hrsg.) (2012) Interdisziplinäre S3-Leitlinie für die Diagnostik, Therapie und Nachsorge des Mammakarzinoms. Leitlinienprogramm Onkologie der AWMF, Deutschen Krebsgesellschaft eV und Deutschen Krebshilfe eV (AWMF-Register-Nummer: 032 – 045OL)
Voduc KD, Cheang MC, Tyldesley S, Gelmon K, Nielsen TO, Kennecke H (2010) Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol 28(10):1684–1691. doi:10.1200/JCO.2009.24.9284
Lowery AJ, Kell MR, Glynn RW, Kerin MJ, Sweeney KJ (2012) Locoregional recurrence after breast cancer surgery: a systematic review by receptor phenotype. Breast Cancer Res Treat 133(3):831–841. doi:10.1007/s10549-011-1891-6
Mersin H, Gulben K, Berberoglu U, Yazi M, Acun G, Kinas V, Erdogan S (2011) Prognostic factors affecting postmastectomy locoregional recurrence in patients with early breast cancer: are intrinsic subtypes effective? World J Surg 35(10):2196–2202. doi:10.1007/s00268-011-1240-2
Soerjomataram I, Louwman MW, Ribot JG, Roukema JA, Coebergh JW (2008) An overview of prognostic factors for long-term survivors of breast cancer. Breast Cancer Res Treat 107(3):309–330. doi:10.1007/s10549-007-9556-1
Hannoun-Levi JM, Resch A, Gal J, Kauer-Dorner D, Strnad V, Niehoff P, Loessl K, Kovacs G, Van Limbergen E, Polgar C (2013) Accelerated partial breast irradiation with interstitial brachytherapy as second conservative treatment for ipsilateral breast tumour recurrence: multicentric study of the GEC-ESTRO Breast Cancer Working Group. Radiother Oncol 108(2):226–231. doi:10.1016/j.radonc.2013.03.026S0167-8140(13)00156-4
Acknowledgments
Juergen Hedderich and Ulrike von Hehn advised and performed the statistical analyses.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wenners, A., Berlin, L., Alkatout, I. et al. Clinical implications of first and multiple locoregional breast cancer recurrences. Arch Gynecol Obstet 292, 165–173 (2015). https://doi.org/10.1007/s00404-014-3586-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3586-9