Abstract
Purpose
To compare the effectiveness of expectant management versus methotrexate in selected cases of tubal ectopic pregnancy.
Methods
A double-blind randomized trial included 23 selected patients with a confirmed diagnosis of tubal pregnancy who met the inclusion criteria (hemodynamic stability, initial serum β-hCG concentration <2,000 mIU/mL, declining titers of β-hCG 48 h prior to treatment, visible tubal pregnancy on transvaginal ultrasound, a tubal mass <5.0 cm and fertility desire). The patients were divided into two groups: 10 patients in the methotrexate group (MTX 50 mg/m2 administered as a single intramuscular dose) and 13 patients in the placebo group (saline solution administered in a single intramuscular dose). Quantitative variables were expressed as means ± standard deviations and compared by Student’s t test or Mann–Whitney test. Dichotomous variables (success/treatment failure) were presented as proportions and compared by the Fisher exact test.
Results
Successful treatment with negative titers of β-hCG occurred in 9 cases (90.0 %) of the methotrexate group and in 12 (92.3 %) of the placebo group (p > 0.999). The β-hCG values became undetectable at 22 ± 15.4 days in the methotrexate group and 20.6 ± 8.4 days in the placebo group (p = 0.80).
Conclusion
This study showed no statistically significant difference between the treatment with methotrexate and placebo, with similar success rates and similar time interval for β-hCG to become undetectable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ectopic pregnancy is the leading cause of maternal death in the first trimester of pregnancy [1]. The association of transvaginal ultrasound and beta fraction of human chorionic gonadotropin (β-hCG) contributed for an earlier diagnosis of unruptured ectopic pregnancy. Thus, therapeutic approaches such as systemic methotrexate (MTX) or expectant management are now reasonable [2].
The very first report of expectant management dates from 1955 when Lund [3] conducted an observational prospective study in which 57 % of 119 patients with ectopic pregnancy not undergoing surgery healed spontaneously. Later studies adopting the same strategy demonstrated success rates ranging from 48 to 100 % [4–13]. The case selection should be meticulous and meet all the following criteria: hemodynamic stability, transvaginal ultrasound without embryonic cardiac activity, and declining titers of β-hCG in 24–48 h before treatment [4, 5].
Expectant management in ectopic pregnancy is not as well established as systemic treatment with MTX, which proved to be safe and cost-effective [2, 14]. A Cochrane review regarding the effectiveness of expectant management was inconclusive once most studies had not been conducted with a strict methodology [15]. Considering the controversial literature and the lack of randomized double-blind trials, this study aims to compare the effectiveness of expectant management versus methotrexate in selected cases of tubal ectopic pregnancy.
Methods
A double-blind randomized trial conducted from September 2011 to January 2013 in the Department of Obstetrics at the Federal University of São Paulo (UNIFESP) included selected patients with a confirmed diagnosis of tubal pregnancy who met the inclusion criteria. Non-tubal ectopic pregnancy (cervical, cesarean section scar, ovarian, interstitial and abdominal) or even pregnancies of unknown location were not included. The research ethics committee approved the study, and all volunteering patients signed an informed consent.
Inclusion criteria were: hemodynamic stability, initial serum β-hCG concentration <2,000 mIU/mL, declining titers of β-hCG 48 h prior to treatment, visible tubal pregnancy on transvaginal ultrasound characterized by an inhomogeneous adnexal mass or a tubal ring with or without a yolk sac [16], a tubal mass <5.0 cm and fertility desire.
Exclusion criteria were: embryonic cardiac activity on transvaginal ultrasound, signs of tubal rupture, and contraindication for MTX.
The diagnosis was based on the association of clinical history, gynecological examination, transvaginal ultrasound and quantitative dosage of serum β-hCG. Patients with a missed period, vaginal bleeding and/or pelvic pain combined with a positive β-hCG test underwent a transvaginal sonography. Ectopic pregnancy was confirmed in the presence of an empty uterine cavity and a visible tubal mass. Patients without intrauterine pregnancy and no visible image of tubal pregnancy were followed with a 48 h β-hCG curve and consecutive sonographic study, if necessary. Once the diagnosis was confirmed, these patients were also included.
Those who agreed to participate underwent a double-blind randomization and were divided into two groups: the methotrexate group (MTX 50 mg/m2 administered as a single intramuscular dose) and the placebo group (saline solution administered in a single intramuscular dose).
Blood type and Rh factor were performed, as well as other exams prior to the medication and 7 days after, including a complete blood count, AST, ALT, urea, and creatinine. Whenever Rhesus factor was negative, we tested for indirect Coombs and if it was also negative, we administrated anti-D immunoglobulin.
Treatment results were conducted as follows: declining titers of β-hCG >15 % between the 4th and 7th days were repeated weekly until they became undetectable (<5 mIU/mL), whereas a decrease in smaller proportions was considered treatment failure due to persistent trophoblastic tissue.
Statistical analysis of all data collected was performed using the SPSS software (SPSS Inc., Chicago, IL, USA) version 15.0 for Windows. Quantitative variables are expressed as means ± standard deviations and compared by Student’s t test or Mann–Whitney test. Dichotomous variables (success/treatment failure) are presented as proportions and compared by the Fisher exact test. Only p values <0.05 were considered statistically significant.
Results
Study population
The sample consisted of 23 individuals, 10 allocated in the methotrexate group (43.5 %) and 13 in the placebo group (56.5 %). Comparisons of the population characteristics of both groups are summarized in Table 1.
The time of the last menstrual period in the methotrexate group was 8.4 ± 1.9 weeks and the placebo group was 8.1 ± 1.6 weeks. Only three patients (30 %) in the methotrexate group presented with the classic triad (missed period, vaginal bleeding and pelvic pain), while seven patients (46.2 %) in the placebo group reported these complaints as indicated in Table 2.
The mean initial value of β-hCG in the methotrexate group was 883 ± 729 and 704 ± 666 mIU/mL 48 h later, while the placebo group had an initial mean value of 794 ± 868 and 547 ± 641 mIU/mL in the following 48-h period. Regarding ultrasonographic aspects, the average size of the tubal mass was 28.3 ± 8.2 mm in the methotrexate group, and 25.8 ± 9.7 mm in the placebo group.
Treatment success
Successful treatment with negative titers of β-hCG occurred in 9 cases (90.0 %) of the methotrexate group and in 12 (92.3 %) of the placebo group (p > 0.999) as shown in Table 3.
Considering a threshold of 1,000 mIU/ml for the initial titer of β-hCG, 7 cases in the MTX group and 12 cases in the placebo group with levels below 1,000 mIU/mL had a successful treatment. One out of 3 cases with levels above 1,000 mIU/mL in the MTX group and the only case from the placebo group failed.
One failing treatment from each group required surgical intervention. The single case belonging to the methotrexate group did not meet the 15 % decline in β-hCG titers criteria and the woman in the placebo group evolved with persistent abdominal pain associated with free fluid detected by sonography. Neither patient had signs of tubal rupture or hemoperitoneum (Table 3).
Time for β-hCG titers to become undetectable
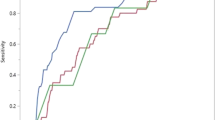
The β-hCG values became undetectable at 22 ± 15.4 days in the methotrexate group and 20.6 ± 8.4 days in the placebo group (p = 0.80) (Fig. 1).
Changes in laboratory tests
No patient in both groups had abnormal blood count and altered liver or renal function before or after treatment (Table 4).
Discussion
Ectopic pregnancy is the leading cause of maternal death in the first trimester of pregnancy [1]; yet, evidence regarding the efficacy of expectant management is scarce. Therefore, we conducted this double-blind randomized trial, comparing the outcomes of expectant versus MTX treatment where the groups presented a success rate of 92.3 and 90 %, respectively. The results suggest that there is no need to use MTX in selected cases since there was no statistically significant difference between the two homogeneous groups. Once this study was conducted in a single center during a 2-year period with rigorous inclusion criteria, the total number of participating patients was not sufficient to reach the desired statistic power.
Each group had only one case of treatment failure. None of them had tubal rupture or hemoperitoneum and the level of β-hCG was above 1,000 mIU/mL in both. Thus, further studies with a greater sample with a threshold of 1,000 mIU/mL for the initial β-hCG are encouraged, considering the absolute success rate even with only 20 patients.
Treatment failure was considered when titers of β-hCG decreased less than 15 %, which suggested a persistent trophoblastic tissue. Since the double-blind nature of the study permitted unawareness of the actual medication administered, these cases were conducted with surgery to prevent complications including tubal rupture. The failing case in the MTX group probably happened due to its local action on the trophoblastic tissue releasing β-hCG in the circulation, and surgical management was indicated for the patient in the placebo group due to persistent abdominal pain.
A randomized study by van Mello et al. [17] compared expectant management versus treatment with MTX and ended up indicating surgery for 1 out of 41 patients (2 %) in the MTX group and 4 out of 32 patients (13 %) in the expectant management group. The sole indication for surgical intervention was the complaint of pain and no tubal ruptures were observed.
To our knowledge, only two double-blind studies evaluating expectant management for tubal pregnancy are described in the literature. Egarter et al. [18] compared the use of prostaglandin and placebo in 23 cases of tubal ectopic pregnancy with β-hCG titers up to 2,500 mIU/mL. Since both prostaglandin and placebo were locally injected guided by laparoscopy, the disadvantage of this study is that expectant management was evaluated through an invasive procedure. On the remaining double-blind study, Korhonen et al. [6] evaluated 60 cases, divided into groups treated with placebo or oral MTX at a dose of 2.5 mg per day for 5 days. Such sub dose of oral MTX is now known to be ineffective for ectopic pregnancy, so this study practically compares two placebos. Our research is the only double-blind study in the literature using methotrexate in a single intramuscular dose of 50 mg/m2, a protocol that has already been acclaimed throughout medical literature.
The main predicting criteria for a successful expectant management are: low initial titers of β-hCG, declining titers of β-hCG in 48 h, no intrauterine gestational sac assessed by ultrasonography and longer interval since the last menstrual period [4, 5, 8].
Initial titers of β-hCG were as low as 883 ± 729 mIU/mL in the MTX group and 794 ± 868 mIU/mL in the placebo group (p = 0.445). Similarly, van Mello et al. [17] also obtained low titers of β-hCG, with an average of 535 ± 500 mIU/mL in the MTX group and 708 ± 376 mIU/mL in the expectant group. Elito Jr and Camano [4] employing the expectant management observed a mean β-hCG value of 648.8 ± 754.7 mIU/mL. Thus, both studies support the treatment’s safety in patients with titers of β-hCG under 2,000 mIU/mL.
One of the main selection criteria for expectant management is declining titers of β-hCG in 48 h, once it reflects involution of pregnancy. Mavrelos et al. [13] indicated expectant management in 144 tubal pregnancies with β-hCG titers under 1,500 mIU/mL. A total of 80 patients had declining titers within 48 h and 64 had them rising. The success obtained in patients with a declining β-hCG was 88.8 % against 51.6 % on the other group. In our study, the mean decrease in a 48-h period was 26.4 % in the methotrexate group and 29.3 % in the placebo group.
In our setting, early diagnosis of ectopic pregnancy was not always possible. The average time of patients’ last menstrual period was 8.3 weeks. As demonstrated by Elito Jr and Camano [4], the women with longer intervals since their last period could be in the declining phase of β-hCG levels when the risk of tubal rupture is diminished. So as the pregnancy is involuting and the trophoblastic tissue is being absorbed, specific treatments are no longer needed.
The mean time for β-hCG to become undetectable in the methotrexate group was 22 ± 15.4 and 20.6 ± 8.4 days in the placebo group (p = 0.80). This proves that there is no benefit in the use of MTX in selected patients with respect to an earlier decrease in the β-hCG titers. Additionally, laboratory tests in both groups showed no alteration, demonstrating that a single dose of MTX is relatively safe whenever its indication is appropriate.
In conclusion, this double-blind randomized trial did not demonstrate statistically significant difference between the treatment with methotrexate and placebo. It also facilitates the physicians’ decision-making process as well as provides evidence in favor of the expectant management for selected cases, contributing to lower hospital costs and reducing the unnecessary use of specific treatments for tubal ectopic pregnancy.
References
Barnhart K, Coutifaris C, Esposito M (2001) The pharmacology of methotrexate. Expert Opin Pharmacother 2:409–417
Barnhart KT (2009) Clinical practice. Ectopic pregnancy. N Engl J Med 361:379–387
Lund JJ (1955) Early ectopic pregnancy treated nonsurgically. J Obstet Br Empire 62:70–76
Elito J Jr, Camano L (2000) Unruptured tubal pregnancy: different treatments for early and late diagnosis. São Paulo Med J 124:321–324
Ylostalo P, Cacciatore B, Sjoberg J, Kaariainen M, Tenhunen A, Stenman UH (1992) Expectant management of ectopic pregnancy. Obstet Gynecol 80:345–348
Korhonen J, Stenman UH, Ylostalo P (1996) Low-dose oral methotrexate with expectant management of ectopic pregnancy. Obstet Gynecol 88:775–778
Cacciatore B, Korhonen J, Stenman UH, Ylostalo P (1995) Transvaginal sonography and serum hCG in monitoring of presumed ectopic pregnancies selected for expectant management. Ultrasound Obstet Gynecol 5:297–300
Trio D, Strobelt N, Picciolo C, Lapinski RH, Ghidini A (1995) Prognostic factors for successful expectant management of ectopic pregnancy. Fertil Steril 63:469–472
Shalev E, Peleg D, Tsabari A, Romano S, Bustan M (1995) Spontaneous resolution of ectopic tubal pregnancy: natural history. Fertil Steril 63:15–19
Lui A, D’Ottavio G, Rustico MA, Conoscenti G, Fischer Tamaro F, Meir YJ et al (1997) Conservative management of ectopic pregnancy. Minerva Ginecol 49:67–72
Olofsson JI, Poromaa IS, Ottander U, Kjellberg L, Damber MG (2001) Clinical and pregnancy outcome following ectopic pregnancy; a prospective study comparing expectancy, surgery and systemic methotrexate treatment. Acta Obstet Gynecol Scand 80:744–759
Elson J, Tailor A, Banerjee S, Salim R, Hillaby K, Jurkovic D (2004) Expectant management of tubal ectopic pregnancy: prediction of successful outcome using decision tree analysis. Ultrasound Obstet Gynecol 23:552–556
Mavrelos D, Nicks H, Jamil A, Hoo W, Jauniaux E, Jurkovic D (2013) Efficacy and safety of a clinical protocol for expectant management of selected women diagnosed with a tubal ectopic pregnancy. Ultrasound Obstet Gynecol 42:102–107
Elito J Jr, Reichmann A, Uchiyama M, Camano L (1999) Predictive score for the systemic treatment of unruptured ectopic pregnancy with a single dose of methotrexate. Int J Gynecol Obstet 67:75–79
Hajenius PJ, Mol F, Mol BW, Bossuyt PM, Ankum WM, van der Veen F (2007) Interventions for tubal ectopic pregnancy. Cochrane Database Syst Rev (1):CD000324
Kirk E, Bottomley C, Bourne T (2014) Diagnosing ectopic pregnancy and current concepts in the management of pregnancy of unknown location. Hum Reprod Update 20:250–261
van Mello NM, Mol F, Verhoeve HR, van Wely M, Adriaanse AH, Boss EA et al (2013) Methotrexate or expectant management in women with ectopic pregnancy of unknown location and low serum hCG concentrations? A randomised comparison. Hum Reprod 28:60–67
Egarter C, Kiss H, Husslein P (1991) Prostaglandin versus expectant management in early tubal pregnancy. Prostaglandins Leukot Essent Fatty Acids 42:177–179
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Silva, P.M., Araujo Júnior, E., Cecchino, G.N. et al. Effectiveness of expectant management versus methotrexate in tubal ectopic pregnancy: a double-blind randomized trial. Arch Gynecol Obstet 291, 939–943 (2015). https://doi.org/10.1007/s00404-014-3513-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3513-0