Abstract
Purpose
Undifferentiated uterine sarcomas (UUS) are rare and aggressive tumor with scarce data on the outcome and best treatment. We aimed to describe the behavior among patients with UUS at our institution.
Materials and methods
Thirteen patients with UUS treated in our centre from 1979 to 2010 were analyzed. Statistics: descriptive analysis for frequencies and Kaplan–Meier actuarial method for overall survival (OS).
Results
Patients mean age was 66 years. Three had FIGO 2009 stage IA, five IB, two IIB, and three IVB. Ten patients underwent surgery and eight received postoperative radiotherapy. Three patients received adjuvant chemotherapy. The median follow-up was 16 months (2–276 months). Stage I patients developed two local relapses and three distant metastases (DM). DM was also observed in stage II patients and in 61.5 % of the entire series. Fifty percent of patients receiving radiotherapy remain alive without relapse. The median OS was 16 months, being 17 months for stage I and 9 for the remainder.
Conclusions
Poor outcome of UUS was associated with a high incidence of DM. Stage I had the best outcome. Radiotherapy seems to have benefited patients, with 100 % of local control and 50 % of long-term survivors. The high incidence of metastasis suggests the need for more accurate initial assessment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Uterine sarcomas are rare tumors that affect 3–7/10,000 women in the United States and constitute 3–7 % of uterine neoplasms [1]. Characteristically, they are a heterogeneous pathologic group of neoplasms, with an aggressive behavior and worse prognosis than endometrial carcinoma [2]. Following the 2003 World Health Organization (WHO) classification there are four main types of uterine sarcomas: leimyosarcoma, endometrial stromal sarcoma (ESS), adenosarcoma, and undifferentiated sarcoma, each having a different outcome and management [3].
Undifferentiated uterine sarcomas (UUS) are rare and aggressive uterine neoplasms. Historically, many tumors currently referred to as UUS were classified as high-grade ESS. A few small case series have shown that UUS behave more aggressively than the more widely described lowgrade ESS [4]. The UUS have now been classified according to the last edition of the WHO, although it is still controversial whether high-grade ESS are actually UUS [3–6]. Based on the few reports published to date we know that low grade ESS have an indolent clinical course, whereas UUS have an aggressive behavior [7–10].
Considering their bad behavior UUS are one of the most aggressive mesenchymal uterine tumors, with 25 % of survivors at 5 years. Fortunately, despite the lack of consistent data related to the treatment, UUS are uncommon and are the least frequent of the four pathological types [11].
The diagnosis of UUS is established after surgery on the basis of its pathologic features. These sarcomas are characteristically composed of cells with severe nuclear pleomorphism, high mitotic activity (10 mitotic figures per 10 high-power fields), extensive myometrial invasion, necrosis and lack of specific differentiation [11]. UUS are diagnosed by exclusion after discarding other high-grade uterus tumors with a sarcomatous component.
Considering their low incidence there is little information in the literature related to the most effective treatment for UUS. Wide series are scarce and usually include cases over long periods of time (20–30 years or more). The largest series included only 21 patients and other series have reported only isolated cases [6]. The conventional treatment for these tumors is surgery and consists of total hysterectomy and bilateral salpingo-oophorectomy. Lymphadenectomy is or is not performed as part of surgical staging. Although radiotherapy and chemotherapy are considered as adjuvant treatments, little data has been reported on their effectiveness [5–8, 12]. What is well known is its poor survival, with 25 % of survivors at 5 years. Several prognostic factors with an impact on survival have been reported, including tumour size, vascular and lymphatic invasion, myometrial involvement and necrosis, among others [13–16].
The aim of the present study was to evaluate the characteristics and clinical outcomes of a series of 13 patients with UUS treated at our institution over a 31-year period and provide information to the literature about the behavior of UUS.
Patients and methods
From the files of the Department of Pathology we identified all the uterine tumors with a mesenchymal component diagnosed from 1979 to 2010. After a thorough pathological review of all the histological slides (6–23) by an experienced gynaecological pathologist, cases with a pure sarcomatous pattern were identified. Within this subset of tumors with pure sarcomatous growth, all cases fulfilling the definition of undifferentiated uterine sarcoma according to the last version of the WHO classification were selected for the study.
For the pathological analysis of the UUS all the slides available from surgical specimens were independently reviewed by two pathologists and the diagnosis was confirmed in all cases. When differences between the two independent evaluations were detected, a new consensus evaluation was conducted.
Clinical and epidemiologic data were obtained from the medical records. Tumor size, location and stage were obtained through the review of the surgical and pathological reports. Tumor stage was assigned according to criteria of the last reviewed International Federation of Gynaecology and Obstetrics (2009 FIGO) [17]. Primary treatment modality data (surgery, radiation therapy, chemotherapy, etc.) as well as treatment approach at recurrence were obtained from the review of the clinical files. All patients were followed in the Gynaecological Cancer Unit. Routine follow-up of each patient was conducted at 3-month intervals during the first 2 years and every 6 months afterwards. Additional diagnostic procedures (i.e. CT-scan, magnetic resonance imaging, thorax radiography, bone scintigraphy) were carried out when clinically indicated. The study was approved by the institutional Ethical Review Boards of our institution.
The Kaplan–Meier actuarial method was used to analyze the overall survival (OS). Statistical analysis was performed by SPSS 18.0 version (IBM, Armonk, NY, USA).
Results
Since 1979 a total of 170 cases fulfilling the definition for mesenchymal uterine tumors were diagnosed and treated at the Gynaecological Cancer Unit in the Hospital Clínic of Barcelona (HCB). Of these, 103 were carcinosarcomas and 67 were uterine sarcomas: 41 leiomyosarcomas, 9 adenosarcomas, 4 endometrial stromal sarcomas and only 13 UUS patients. The cases who revealed histology of UUS represent 7.6 % of the all the mesenchymal tumors and 19.4 % of uterine sarcomas.
The age of the patients ranged from 50 to 83 years old, with a mean age of 66 years. Metrorrhagia was the main symptom at diagnosis and prior to initiation of the therapeutic approach a CT and/or MRI was performed for clinical staging. Twelve out of the 13 patients underwent surgery, two with a palliative aim because of distant metastasis and one patient was not operated because of poor performance status and metastatic disease at diagnosis. Surgery consisted in hysterectomy plus salpingo-oophorectomy in 11/13, and lymphadenectomy was added in only one patient. The FIGO 2009 distribution by stage was: stage I in eight patients (IA 3, IB 5), stage IIB in two and stage IVB in three patients. The pathologic characteristics of the series are shown in Table 1.
Radiation therapy was administered in ten patients, in eight as adjuvant therapy and as palliative treatment after relapse in two cases. External beam radiotherapy (EBRT) was administered to seven patients using 6 or 18 MV photons from a Linac with a 2 or 4 pelvic field technique. The given dose ranged between 40 Gy and 66 Gy, with a median of 45 Gy. Seven patients received brachytherapy: six after EBRT and one as exclusive treatment after surgery; five patients were treated with HDR in three fractions of 5 Gy (192Ir and Micro-selectron nucletron® source projector), two patients were treated with LDR (137Cs and Selectron nucletron® source projector): one with a dose of 21 Gy after EBRT and 1 received 50 Gy as exclusive brachytherapy treatment. Only 3/13 patients received chemotherapy (ChT) as adjuvant treatment based in Doxorubicin/Ifosfamide; 4/13 received ChT with a palliative aim after local relapse and/or distant metastasis with different schedules. After treatment the patients were followed every 3 months during the first 2 years and every 4–6 months thereafter or until death.
Pathologic study of the present series showed aggressive features: a high rate of mitoses (>15 per HPF) was observed in all samples; most tumors were large (7/13 exceeded 8 cm. and 4/13 had >10 cm), necrosis was present in 10/13; myometrial invasion (MI) was detected in 11/13 of the cases and 8/13 had MI more than 50 %. In 9/13 vascular and lymphatic space invasion (VLSI) was observed. The pathologic characteristics of the series are shown in Table 1.
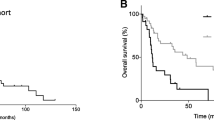
The median follow-up of the series was 16 months (2–276 months). Three patients had distant metastasis at diagnosis, with a median survival of 3 months. Of the 10 patients treated with a curative aim 1 had vaginal and parametrial relapse, 1 developed vaginal relapse and distant metastasis and 4 exclusively distant metastasis. Patients without relapse (4/10, 40 %) remained alive at the time of the analysis and all had stage I. Table 2 shows the distribution of the characteristics of the patients that were alive versus those who had died. The median OS was 16 months (mean 77.8): stage I was 17 months and 9 months for the remaining patients (mean 126 vs. 14.). In stage I 50 % of the patients (4/8) died because of distant metastases, but one had local progression also. Patients with stages II-IV all died because of metastatic disease. The most common sites of distant metastases were the lung, pleura, peritoneum and liver. Figure 1 shows the overall survival curves for the entire series (a) and for stage I (b).
Patients with a tumor size less than 8 cm showed a better mean survival than those with larger sized tumors (156 vs. 20 months p = 0.056). VLSI and MI showed a trend to a poorer outcome, albeit not statistically significant. The size of 8 cm was chosen because was the median tumor size and there were only 4 patients with tumor size less than 4.5 cm.
In the group of ten patients treated with curative aim, none of the eight patients treated with radiation therapy (EBRT and/or BQT) developed local relapse, in contrast with the only two patients who did not receive irradiation, who presented local relapse, despite stage I. Patients receiving postoperative irradiation had 100 % of local control, nevertheless, four developed distant metastasis. The OS of the two stage II patients, who died due to distant metastases with local disease control, was greater than the two stage I non irradiated patients who fail locally.
Discussion
The UUS are an orphan topic in the literature. Only one series have reported more than 13 cases and the remaining isolated reports are usually described as case reports. Considering their low incidence and also because of the changes in the WHO classification, it is very difficult to reach conclusions as to the best treatment. In the present series UUS represented 7.6 % of all mesenchymal tumors and 19.4 % of the uterine sarcomas. Poor prognosis is of note in all the series and case reports described in the literature, with 25 % of survivors at 5 years [6–9]. In the present series the survival of the entire series was 30.7 %, being 40 % on exclusion of those with metastatic disease at diagnosis. In the present series survival was related to stage, with 50 % survivors at 5 years for stage I in comparison to 0 % for stages II-IVB.
As reported by other authors VLSI, MI and tumor size may be related to a worse outcome; nevertheless the number of patients analyzed in the present series does not allow any conclusion on prognostic factors to be established, despite comparing stage I vs. II–IV. On the other hand, it is well known that VLSI is responsible for distant metastasis, tumor size >5 cm is responsible for a more advanced stage, and that stage is the main prognostic factor in US. In the present series MI ≥ 50 % was observed in 61.5 %, VLSI in 69.3 % and a tumor size >5 cm in 69.3 %, being much greater than that expected for endometrial carcinoma and other types of uterine sarcoma [12–14]. All these factors contribute to the poor outcome of these patients which is demonstrated by the 3/13 patients with distant metastasis at diagnosis and 61.5 % in the entire series. Fifty percent of patients treated with aim to cure developed distant metastasis. This incidence of distant metastasis in USS is higher than in other uterine sarcomas. Thus, the need to perform imaging strategies such as PET/CT should be considered in order to detect possible occult distant disease in early stage of the disease.
All patients but one were underwent surgery. Despite only one patient having surgical lymph node analysis, nodal relapse was not found; nevertheless, 8/10 patients received pelvic radiotherapy after surgery. This would suggest a hematological spread instead lymphatic spread and/or a role of the radiotherapy treatment to control microscopic lymphatic metastases.
In contrast to other reports, in the present series 80 % of patients treated with a curative aim underwent adjuvant radiotherapy against only 30 % receiving adjuvant chemotherapy [6, 12]. A hundred percent of local control and a 50 % of survivors in stage I at 2 and 5 years was achieved in irradiated patients. Although chemotherapy treatment was not related with better outcome in our series (the four long—survivors did not receive it), we think should be considered in the future as a part of the therapeutic strategy because the high incidence of distant metastases.
In the only study in the literature with more patients than the present one, chemotherapy was used as complementary treatment after surgery. In that series composted by 19 patients: 6 stage I, 2 stage III and 11 stage IV disease, radiotherapy was not administered except in 4 stage I patients. The authors added adjuvant gemcitabine/docetaxel, doxorubicin, and ifosfamide/doxorubicin, concluding that chemotherapy achieved objective, but short-lived, responses in patients with measurable disease. One of the irradiated patients had local relapse and three had distant metastasis. The disease free-survival of the entire series was 7 months being 15 months for stage I. The median OS for the entire series was 11.8 months, being 26.5 months for stage I. In stage I, 33 % of the patients remained alive at 5 years [6]. In the present series we showed 50 % survivors in stage I and 100 % of local control in irradiated patients. Although the median survival was 17 months for stage I, these data are not comparable taking the number of patients into account.
The 100 % of local control without lymphadenectomy and the 50 % of survival rate observed in stage I patients suggest that radiotherapy would be administered as adjuvant treatment in UUS.
In conclusion, UUS are infrequent uterine sarcomas with a bad outcome mainly due to distant metastasis. This high incidence of metastasis suggests the need for more accurate initial assessment (i e. PET/TC at diagnosis) and more intensive treatments, with chemotherapy as the first treatment after surgery. The local control obtained in these patients receiving irradiation seems to indicate that radiotherapy would be administered in UUS. The lack of more information in the literature warrants multicentric analysis to establish the best treatment in these patients. Stage I showed the best outcome with four long-survivors.
References
Harlow BL, Weiss NS, Lofton S (1986) The epidemiology of sarcomas of the uterus. J Natl Cancer Inst 76:399–402
Gadducci A, Sartori E, Landoni F, Zola P, Maggino T, Cosio S et al (2002) The prognostic relevance of histological type in uterine sarcomas: a Cooperation Task Force (CTF) multivariate analysis of 249 cases. Eur J Gynaecol Oncol 23:295–299
Hendrickson MR, Tavassoli FA, Kempson RL (2003) Mesenchymal tumours and related lesions. In: Tavassoli FA, Deville P (eds) Pathology and genetics of tumours of the breast and female organs. IARC, Lyon, pp 233–244
Kurihara S, Oda Y, Ohishi Y, Iwasa A, Takahira T, Kaneki E et al (2008) Endometrial Stromal Sarcomas and Related High-grade Sarcomas: immunohistochemical and molecular genetic study of 31 Cases. Am J Surg Pathol 32:1228–1238
Xue W-C, Cheung ANY (2011) Endometrial stromal sarcoma of uterus. Best Pract Res Clin Obstet Gynaecol 25:719–732
Tanner EJ, Garg K, Leitao MM, Soslow RA, Hensley ML (2012) High grade undifferentiated uterine sarcoma: surgery, treatment, and survival outcomes. Gynecol Oncol 127:27–31
Ning L, Ling-Ying W, Hong-Tu Z, Ju-Sheng A, Xiao-Guang L, Shao-Kang M (2008) Treatment options in stage I endometrial stromal sarcoma: a retrospective analysis of 53 cases. Gynecol Oncol 108:306–311
Chang KL, Crabtree GS, Lim-Tan SK, Kempson RL, Hendrickson MR (1990) Primary uterine endometrial stromal neoplasms. a clinicopathologic study of 117 cases. Am J Surg Pathol 14:415–438
Klaus B, Barbara BA, Andreas O, Windbichler G, Petru E, Mayerhofer S et al (2001) Prognostic parameters in endometrial stromal sarcoma: a clinicopathologic study in 31 patients. Gynecol Oncol 81:160–165
Valduvieco I, Rovirosa A, Colomo L, De San Juan A, Pahisa J, Biete A (2010) Endometrial stromal sarcoma. is there a place for radiotherapy? Clin Transl Oncol 12(3):226–230
D’Angelo E, Prat J (2010) Uterine sarcomas: a review. Gynecol Oncol 116:131–139
Zagouri F, Domopoulos A-M, Fotiou S, Kouloulias V, Papadimitriou A (2009) Treatment of early uterine sarcomas: disentangling adjuvant modalities. World J Surg Oncol 7:38–48
Rovirosa A, Ascaso C, Ordi J, Abellana R, Arenas M, Lejarcegui JA et al (2002) Is vascular and lymphatic space invasion a main prognostic factor in uterine neoplasms with a sarcomatous component? a retrospective study of prognostic factors of 60 patients stratified by stages. Int J Radiat Oncol Biol Phys 52(5):1320–1329
Schick U, Bolukbasi Y, Thariat J (2012) Outcome and prognostic factors in endometrial stromaltumors: a rare cancer network study. Int J Radiation Oncol Biol Phys 82(5):757–763
Chew I, Oliva E (2010) Endometrial stromal sarcomas. a review of potential prognostic factors. Adv Anat Pathol 17(2):113–121
Rovirosa A, Ascaso C, Ordi J, Arenas M, Valduvieco I, Lejarcegui JA et al (2009) How to deal with prognostic factors and radiotherapy results in uterine neoplasms with a sarcomatous component? Clin Transl Oncol 11(10):681–687
FIGO staging for uterine sarcomas (2009) Int J Gynaecol Obstet 104:179
Conflict of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject or materials discussed in the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ríos, I., Rovirosa, Á., Morales, J. et al. Undifferentiated uterine sarcoma: a rare, not well known and aggressive disease: report of 13 cases. Arch Gynecol Obstet 290, 993–997 (2014). https://doi.org/10.1007/s00404-014-3311-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3311-8