Abstract
Purpose
To identify risk factors and perinatal outcomes associated with the duration of latency period in women who experience preterm premature rupture of membranes (PPROM).
Methods
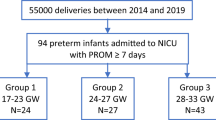
A retrospective study of women who experienced PPROM between 24 and 34 weeks of gestation was performed in a single tertiary center between 2009 and 2013. Patients were divided into two groups based on the duration of the latency period after PPROM: Group 1 ≤72 h and Group 2 >72 h. Risk factors and perinatal outcomes were compared according to latency period. Student’s t test and Chi-square test were used to compare continuous and categorical variables, respectively, between the two groups. Multivariate regression analysis was performed to control for potential confounding variables.
Results
In total, 3,257 patients presented with PPROM during the study period; of these, 204 (6.3 %) met the inclusion criteria. Higher gestational age upon admission (odds ratio [OR] = 0.83, 95 % confidence interval [CI] = 0.79–0.87; p < 0.001), oligohydramnios (OR = 0.47, 95 % CI = 0.25–0.91; p = 0.018), and twin gestation (OR = 0.67, 95 % CI = 0.45–0.89; p = 0.032) were independently associated with a shortened latency period. In addition, prolonged latency significantly increased the occurrence of chorioamnionitis (OR = 2.23, 95 % CI = 1.48–3.14; p = 0.002), placental abruption (OR = 1.9, 95 % CI = 0.95–3.53; p = 0.033), and decreased the length of stay of neonates in the intensive care unit (OR = 0.85, 95 % CI = 0.39–1.79; p = 0.021).
Conclusion
Gestational age at PPROM, twin gestation, and oligohydramnios significantly affected the latency period. Although a latency period >72 h was associated with chorioamnionitis and placental abruption, adverse neonatal outcomes were not affected.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preterm premature rupture of membranes (PPROM) occurs in approximately 1–3 % of all pregnancies and is responsible for one-third of all premature births [1]. It is generally accepted that PPROM occurring at a gestational age of 24–34 weeks should be conservatively managed, meaning that the pregnancy is prolonged to improve neonatal outcomes [2]. During antenatal surveillance, however, conservatively managed PPROM is associated with an increased risk of serious maternal, fetal, and neonatal morbidities. Gestational age and amniotic fluid volume at the time of PPROM are known factors affecting the incidence of maternal and neonatal complications. In recent years, the latency period (i.e., the time interval between rupture of membranes and delivery) has been suggested as another important factor related to neonatal survival [3, 4]. However, very few studies have comprehensively investigated the relationship between latency period and perinatal outcomes.
Previous reports explored some of the etiologies thought to be responsible for variation in latency period following PPROM. Intra-amniotic infection [5], gestational age [6, 7], placental abruption [5], and fetal distress are some of the key factors associated with a short latency period. Among these risk factors, intra-amniotic infection plays an important role in the initiation and progression of PPROM. However, no previous study has examined the relationship between latency period after PPROM and known inflammatory markers, such as C-reactive protein (CRP), platelet count, total leukocyte count (and its subtypes), neutrophil to lymphocyte ratio (NLR), or platelet to lymphocyte ratio (PLR).
In this study, we aimed to determine whether a variety of known risk factors, including inflammatory markers, could be used to estimate the duration of the latency period after PPROM and to investigate the effect of latency period on both maternal and neonatal outcomes.
Methods
Data were collected retrospectively from the database of a single tertiary center between January 2009 and October 2013. PPROM was defined as the spontaneous rupture of membranes prior to 37 weeks without active labor. Approval of our institutional review board was obtained for this study. The following data were obtained from original medical records: maternal age, parity, type of conception (spontaneous vs. in vitro fertilization [IVF]), maternal illness (preeclampsia or pre-gestational diabetes mellitus [DM]), history of PPROM, previous Cesarean section, antenatal bleeding, tobacco use, fetal gender, gestational age at time of PPROM and delivery, latency period, amniotic fluid index (AFI) upon admission, and maternal serum levels of inflammatory markers (CRP, platelet count, and total leukocyte, lymphocyte and neutrophil counts) upon admission before the administration of antibiotics or steroids. The NLR and PLR were also calculated. The NLR was defined as the absolute neutrophil count divided by the absolute lymphocyte count, and the PLR was defined as the absolute platelet count divided by the lymphocyte count.
We included patients with a confirmed diagnosis of PPROM, as indicated by one or more of the following: (1) a positive Nitrazine paper test; (2) the presence of insulin growth factor binding protein (IGFBP)-1 in the vaginal discharge; (3) gross pooling of amniotic fluid in the vagina. Due to termination of pregnancies with PPROM before 24 weeks and induction of pregnancies after 34 weeks, only patients with a diagnosis of PPROM between 24 weeks 0 days and 33 weeks 6 days were included in this study. Patients with clinical signs of chorioamnionitis, fetal distress, or active labor upon initial admission were excluded. Patients who had previously underwent cervical cerclage or amniocentesis, or those with fetuses with chromosomal or major structural anomalies and/or an estimated birth weight below the 10th percentile, were also excluded.
According to our protocol, patients were hospitalized for conservative management without tocolytic therapy after diagnosis. All patients received betamethasone (two intramuscular doses of 12 mg 24 h apart) for fetal lung maturation and antibiotic prophylaxis consisting of intravenous ampicillin (2 g every 6 h) and erythromycin (250 mg every 6 h) for 48 h, followed by oral amoxicillin (250 mg every 8 h) for 7 days after admission. Upon admission, all patients underwent an ultrasound to confirm gestational age and measure the cumulative four-quadrant AFI [8]. An AFI of <5 cm was considered oligohydramnios. The study protocol for the management of PPROM was based on our experience, as there is currently no consensus regarding the optimal management of PPROM or frequency of surveillance testing [9]. Accordingly, daily nonstress testing, twice-weekly ultrasonography, and as-needed biophysical profiling were performed for fetal surveillance. During ultrasound examinations, placental and amniotic fluid volume were assessed alongside fetal growth to detect placental abruption and pregnancies at high risk of cord compression. Indications for delivery included labor, non-reassuring fetal test results, or a diagnosis of chorioamnionitis or placental abruption.
Obstetric outcomes included gestational age at delivery, chorioamnionitis, placental abruption, cord prolapse, and delivery mode. Chorioamnionitis was clinically defined as the presence of maternal fever (≥38 °C) with two of the following signs in the absence of other potential sources of infection: uterine tenderness, maternal tachycardia (>100 beats/min), maternal leukocytosis (>15,000 cells/mm3), fetal tachycardia (>160 beats/min), and foul odor of amniotic fluid. Histopathological examination of the placenta was performed after all deliveries, but data on the histopathological diagnosis of chorioamnionitis were incomplete and therefore not included in the present study. In cases of clinical chorioamnionitis, patients were treated with ampicillin and gentamicin.
Fetal outcomes included birth weight, Apgar scores at 1 and 5 min, respiratory distress syndrome (RDS), early neonatal sepsis and death, duration of stay in the neonatal intensive care unit (NICU), emergency intubation (within 24 h after birth), and phototherapy. Early neonatal sepsis was defined as sepsis in a neonate with a positive blood or cerebrospinal culture in the first 48 h of life prior to antibiotic administration. Diagnosis of RDS was made based on the need for ventilation for 24 h and radiographic findings.
We categorized patients with PPROM into two groups based on time elapsed between the rupture of membranes and delivery (known as the latency period). Patients in Group 1 had a latency period of ≤72 h, whereas those in Group 2 had a latency period of >72 h. The two groups were compared in terms of demographic characteristics and perinatal outcomes.
Statistical analyses were performed using SPSS 20.0 for Windows. Continuous data were expressed as the mean ± standard deviation, while categorical data were presented as the number of patients. After assessing normality, continuous variables were compared between groups using Student’s t test. Categorical variables were compared between groups using the Chi-square test. Following univariate analysis, multivariate logistic regression modeling, with backward elimination, was performed to identify independent risk factors and perinatal outcomes significantly associated with prolonged latency (>72 h). Odds ratios (ORs) and their 95 % confidence intervals (CIs) were calculated. A p value of <0.05 was considered significant.
Results
During the study period, a total of 3,257 patients delivered after PPROM. Among these, 204 women experienced PPROM between 24 and 34 weeks of gestation, which included 91 patients (44.6 %) in Group 1 (latency period ≤72 h) and 113 patients (55.4 %) in Group 2 (latency period >72 h). The demographic and obstetric data for Groups 1 and 2 are shown in Table 1. Groups 1 and 2 were similar with respect to maternal age, fetal gender, IVF conception rate, pre-gestational DM, history of PPROM, previous Cesarean section, antenatal bleeding, tobacco use, and inflammatory markers. Higher gestational age upon admission, nulliparity, twin gestation, and the occurrence of oligohydramnios or preeclampsia upon admission were associated with a shorter latency period (≤72 h). In the multiple logistic regression analysis to identify predictors of latency, gestational age at PPROM (p < 0.001), occurrence of oligohydramnios (p = 0.018), and twin gestation (p = 0.032) demonstrated a significant independent association with short latency period (Table 2). A plot of latency period vs. gestational age at PPROM is shown in Fig. 1 (Pearson correlation coefficient r = −0.563, p < 0.001). Nulliparity, preeclampsia, and antenatal bleeding were unrelated to the duration of the latency period.
We next examined differences in perinatal outcomes in patients with PPROM according to latency period (Table 3). Latency period ≥72 h was associated with an increased risk of chorioamnionitis, placental abruption, cord prolapse, and emergency Cesarean delivery. In addition, prolonged latency was negatively correlated with the occurrence of RDS, low Apgar scores at 1 min (<7), and length of stay in the NICU, but was positively correlated with the frequency of early neonatal sepsis. To further examine maternal and neonatal outcomes associated with prolonged latency, multiple logistic regression analysis was performed to control for potential confounders (Table 4). Regarding maternal outcomes, the incidence of chorioamnionitis (p < 0.002) and placental abruption (p = 0.033) was independently associated with prolonged latency, whereas length of stay in the NICU (p = 0.021) was the only neonatal outcome independently associated with latency period. Overall, the duration of latency was not associated with poor neonatal outcomes.
Discussion
Our study indicates that gestational age at the time of PPROM, twin gestation, and oligohydramnios are independent predictors of latency period after PPROM. In accordance with our observations, several studies have shown an inverse correlation between latency period and gestational age [9–12]. Savitz et al. [11] stated that when PPROM occurs at an early gestational age, it is less likely to proceed to labor within a specified time period. On the other hand, other studies have failed to observe any correlation between latency period and gestational age. Atarjavdan et al. [13] compared latency periods in patients who experienced PPROM at a gestational age of ≤30 weeks vs. those at a gestational age of >30 weeks and found no significant difference.
Patients with oligohydramnios (AFI<5 cm) were found to have shorter latency periods [14]. In addition to shortened latency period, several other adverse pregnancy outcomes have been associated with oligohydramnios [15]. The suspected pathophysiology of this relationship is that low amniotic fluid volume increases the frequency of microbial invasion and subsequent fetal inflammatory response syndrome [14].
Our data also indicated that twin gestation significantly reduced the latency period after PPROM. A similar correlation was found in the studies of Jacquemyn et al. [16] and Hsieh et al. [17], who examined women experiencing PPROM before and after 30 weeks of gestation, respectively. The finding that multiple gestations were associated with a shorter latency period was also confirmed at different gestational ages [18–20]. With the exception of Melamed et al. [10], who found no relationship between multifetal gestation and duration of the latency period, our results confirm the majority of previous studies.
It has been previously reported that the latency period is affected by additional factors such as nulliparity [21, 22]. Test et al. [21] demonstrated a significant association between nulliparity and shorter latency periods, although the reason for this relationship was unclear. Our study, in contrast, did not indicate that nulliparity is an independent factor in the prediction of latency after PPROM.
Inflammation of the amniotic cavity, extraplacental membranes, and fetus has been implicated in the initiation and progression of PPROM [23]. CRP, total leukocyte count (and its subtypes), NLR, and PLR are predictors of inflammation. Therefore, high levels of these inflammatory markers may be a risk factor for intrauterine infection. For example, Perrone et al. [24] suggested that high maternal serum CRP levels in PPROM patients upon admission might be an early indicator of funisitis. To our knowledge, there are no previous reports investigating the effect of inflammatory markers on latency period after PPROM. In addition, we observed no correlation between latency period and laboratory markers of the systemic inflammatory response, including serum CRP levels. However, further research is needed to investigate the role of other inflammatory markers, particularly interleukin (IL)-6, which is a hallmark of fetal inflammatory response syndrome.
Our study demonstrates that gestational age at PPROM, chorioamnionitis, placental abruption, and length of stay in the NICU are independently associated with prolonged latency. A direct relationship between PPROM and chorioamnionitis has been demonstrated in multiple studies [10, 20, 21, 25–28]. It is expected that the presence of chorioamnionitis at the time of PPROM will decrease the time to delivery [20]. On the other hand, women showing prolonged latency are at greater risk of chorioamnionitis, as observed in our study [21, 27]. A recent Cochrane review also demonstrated that latency periods >24 h were associated with an increased risk of chorioamnionitis [28]. It is thought that this relationship between prolonged latency and chorioamnionitis is due to the fact bacterial pathogens have more time to ascend into the amniotic cavity after membrane rupture [29]. In addition, the bacteriostatic effect of amniotic fluid will also decrease over time due to fluid loss.
We also observed a significant association between prolonged latency (≥72 h) and placental abruption. In our study, the rate of placental abruption was 7.3 %, which falls within the reported range of 4–12 % [30]. This is consistent with the findings of Hnat et al. [22], who reported that placental abruption is more common in pregnancies complicated by PPROM prior to 28 weeks of gestation. In contrast to our study, Melamed et al. [10] found no relationship between placental abruption and latency period. They attributed this to a lack of statistical power to detect such an association. Our data indicate that patients with prolonged latency were more likely to undergo emergency Cesarean delivery because of chorioamnionitis and placental abruption, which is consistent with the findings of previous studies [6, 15].
Although adverse outcomes, such as chorioamnionitis and placental abruption, were significantly associated with a prolonged latency period, length of stay in the NICU was the only neonatal outcome that was significantly associated with prolonged latency. Unlike chorioamnionitis, development of sepsis in the neonate was not related to the duration of latency. This finding is consistent with the results of several recent observational studies [7, 10, 27, 31]. Manuck et al. [32] suggested that prolonged latency does not appear to worsen outcomes in pregnancies that are complicated by PPROM. Likewise, in a study by Nayot et al. [26], the perinatal death rate was not affected by a latency period >72 h, and the incidence of moderate to severe neonatal morbidity decreased for infants born at up to 34 weeks of gestation. Similarly, Aziz et al. [7] reported that a longer latency period is not associated with increased neonatal sepsis. The reason for more favorable neonatal outcomes in patients with latency periods over 72 h could be the use of antibiotic prophylaxis after PPROM, which reduces the incidence of adverse neonatal outcomes, including early neonatal sepsis, in pregnancies before 34 weeks [33]. Another explanation is that gestational age itself rather than the latency period may be the major determinant of neonatal outcomes [34].
In conclusion, this study identifies the pregnancy-related factors affecting the duration of the latency period in cases of PPROM. Our study showed that higher gestational age at PPROM, oligohydramnios, and twin gestation are associated with a shortened latency period. Accordingly, the data presented in this study can be used by physicians to predict the expected duration of latency. Furthermore, we observed that neonatal morbidity and mortality were not affected by the duration of latency period for infants delivered at up to 33 weeks 6 days gestation. Generally, a conservative approach directed toward extending pregnancy to improve neonatal outcomes is recommended following PPROM at gestational ages between 24 and 34 weeks [2]. Our results support this approach, provided that women with a latency period >72 h are monitored closely for chorioamnionitis and placental abruption.
References
Simhan HN, Canavan TP (2005) Preterm premature rupture of membranes: diagnosis, evaluation and management strategies. BJOG 112:32–37
ACOG Practice Bulletin (2013) No. 139: premature rupture of membranes. Obstet Gynecol 122:918–930
Park SH, Kim HJ, Yang JH, Choi JS, Lim JE, Oh MJ, Na JY (2006) Neonatal brain damage following prolonged latency after preterm premature rupture of membranes. J Korean Med Sci 21:485–489
Mercer BM (2003) Preterm premature rupture of membranes. Obstet Gynecol 101:178–193
Medina TM, Hill DA (2006) Preterm premature rupture of membranes: diagnosis and management. Am Fam Phys 73:659–664
Caughey AB, Robinson JN, Norwitz ER (2008) Contemporary diagnosis and management of preterm premature rupture of membranes. Rev Obstet Gynecol 1:11–22
Aziz N, Cheng YW, Caughey AB (2008) Factors and outcomes associated with longer latency in premature rupture of membranes. J Matern Fetal Neonatal Med 21:821–825
Phelan JP, Smith CV, Broussard P, Small M (1987) Amniotic fluid volume assessment with the four-quadrant technique at 36–42 weeks’ gestation. J Reprod Med 32:540–542
Davis JM, Krew MA, Gill P, Nelson KM, Hopkins MP (2008) The role of continuous fetal monitoring in the management of preterm premature rupture of membranes. J Matern Fetal Neonatal Med 21:301–304
Melamed N, Hadar E, Ben-Haroush A, Kaplan B, Yogev Y (2009) Factors affecting the duration of the latency period in preterm premature rupture of membranes. J Matern Fetal Neonatal Med 22:1051–1056
Savitz DA, Ananth CV, Luther ER, Thorp JM Jr (1997) Influence of gestational age on the time from spontaneous rupture of the chorioamniotic membranes to the onset of labor. Am J Perinatol 14:129–133
Dale PO, Tanbo T, Bendvold E, Moe N (1989) Duration of the latency period in preterm premature rupture of the membranes. Maternal and neonatal consequences of expectant management. Eur J Obstet Gynecol Reprod Biol 30:257–262
Atarjavdan L, Khazaeipour Z, Shahbazi F (2011) Correlation of myometrial thickness and the latency interval of women with preterm premature rupture of the membranes. Arch Gynecol Obstet 284:1339–1343
Park JS, Yoon BH, Romero R, Moon JB, Oh SY, Kim JC, Jun JK (2001) The relationship between oligohydramnios and the onset of preterm labor in preterm premature rupture of membranes. Am J Obstet Gynecol 184:459–462
Vermillion ST, Kooba AM, Soper DE (2000) Amniotic fluid index values after preterm premature rupture of the membranes and subsequent perinatal infection. Am J Obstet Gynecol 183:271–276
Jacquemyn Y, Noelmans L, Mahieu L, Buytaert P (2003) Twin versus singleton pregnancy and preterm prelabour rupture of the membranes. Clin Exp Obstet Gynecol 30:99–102
Hsieh YY, Chang CC, Tsai HD, Yang TC, Lee CC, Tsai CH (1999) Twin vs. singleton pregnancy. Clinical characteristics and latency periods in preterm premature rupture of membranes. J Reprod Med 44:616–620
Pasquier JC, Rabilloud M, Picaud JC, Claris O, Ecochard R, Moret S, Mellier G (2008) Modeling the duration of the latency period after preterm premature rupture of the membranes according to maternal and pregnancy characteristics: DOMINOS study. Eur J Obstet Gynecol Reprod Biol 139:157–163
Bianco AT, Stone J, Lapinski R, Lockwood C, Lynch L, Berkowitz RL (1996) The clinical outcome of preterm premature rupture of membranes in twin versus singleton pregnancies. Am J Perinatol 13:135–138
Dagklis T, Petousis S, Margioula-Siarkou C, Mavromatidis G, Kalogiannidis I, Prapas N, Mamopoulos A, Rousso D (2013) Parameters affecting latency period in PPROM cases: a 10-year experience of a single institution. J Matern Fetal Neonatal Med 26:1455–1458
Test G, Levy A, Wiznitzer A, Mazor M, Holcberg G, Zlotnik A, Sheiner E (2011) Factors affecting the latency period in patients with preterm premature rupture of membranes. Arch Gynecol Obstet 283:707–710
Hnat MD, Mercer BM, Thurnau G, Goldenberg R, Thom EA, Meis PJ, Moawad AH, Iams JD, Van Dorsten JP, National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units (2005) Perinatal outcomes in women with preterm rupture of membranes between 24 and 32 weeks of gestation and a history of vaginal bleeding. Am J Obstet Gynecol 193:164–168
Gomez R, Romero R, Edwin SS, David C (1997) Pathogenesis of preterm labor and preterm premature rupture of membranes associated with intraamniotic infection. Infect Dis Clin N Am 11(1):135–176
Perrone G, Anceschi MM, Capri O, Galoppi P, Pizzulo S, Buccheri M, Pascone R, Nofroni I, Brunelli R (2012) Maternal C-reactive protein at hospital admission is a simple predictor of funisitis in preterm premature rupture of membranes. Gynecol Obstet Invest 74:95–99
Soper DE, Mayhall CG, Dalton HP (1989) Risk factors for intraamniotic infection: a prospective epidemiologic study. Am J Obstet Gynecol 161:562–566
Nayot D, Penava D, Da Silva O, Richardson BS, de Vrijer B (2012) Neonatal outcomes are associated with latency after preterm premature rupture of membranes. J Perinatol 32:970–977
Frenette P, Dodds L, Armson BA, Jangaard K (2013) Preterm prelabour rupture of membranes: effect of latency on neonatal and maternal outcomes. J Obstet Gynaecol Can 35:710–717
Buchanan SL, Crowther CA, Levett KM, Middleton P, Morris J (2010) Planned early birth versus expectant management for women with preterm prelabour rupture of membranes prior to 37 weeks’ gestation for improving pregnancy outcome. Cochrane Database Syst Rev. doi:10.1002/14651858.CD004735
Yoon BH, Kim YA, Romero R, Kim JC, Park KH, Kim MH, Park JS (1999) Association of oligohydramnios in women with preterm premature rupture of membranes with an inflammatory response in fetal, amniotic, and maternal compartments. Am J Obstet Gynecol 181:784–788
Sheiner E, Shoham-Vardi I, Hadar A, Hallak M, Hackmon R, Mazor M (2002) Incidence, obstetric risk factors and pregnancy outcome of preterm placental abruption: a retrospective analysis. J Matern Fetal Neonatal Med 11:34–39
Blumenfeld YJ, Lee HC, Gould JB, Langen ES, Jafari A, El-Sayed YY (2010) The effect of preterm premature rupture of membranes on neonatal mortality rates. Obstet Gynecol 116:1381–1386
Manuck TA, Maclean CC, Silver RM, Varner MW (2009) Preterm premature rupture of membranes: does the duration of latency influence perinatal outcomes? Am J Obstet Gynecol 201(4):414.e1–414.e6
Hutzal CE, Boyle EM, Kenyon SL, Nash JV, Winsor S, Taylor DJ, Kirpalani H (2008) Use of antibiotics for the treatment of preterm parturition and prevention of neonatal morbidity: a metaanalysis. Am J Obstet Gynecol 199(6):620.e1–620.e8
Tanir HM, Sener T, Tekin N, Aksit A, Ardic N (2003) Preterm premature rupture of membranes and neonatal outcome prior to 34 weeks of gestation. Int J Gynaecol Obstet 82:167–172
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ekin, A., Gezer, C., Taner, C.E. et al. Risk factors and perinatal outcomes associated with latency in preterm premature rupture of membranes between 24 and 34 weeks of gestation. Arch Gynecol Obstet 290, 449–455 (2014). https://doi.org/10.1007/s00404-014-3227-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3227-3




