Abstract
Purpose
To evaluate the treatment of simple endometrial hyperplasia without atypia with different gestagens.
Methods
Sixty premenopausal women with histologically documented endometrial hyperplasia without atypia were included in this prospective controlled study. Patients were randomized into two groups: Group I included 30 patients who received lynestrenol (LYN) in a dose of 15 mg/d, while Group II included 30 patients who received micronized progesterone (MP) 200 mg/d for 12 days per cycle for 3 months. Patients were reevaluated with endometrial curettage after treatment. MP and LYN regimens were compared to regression, resolution or persistence rates and metabolic parameters.
Results
After 3 months of treatment in both groups, none of the cases progressed. In LYN group, the rate of resolution was observed to be higher compared to MP group (p = 0.045). LYN was found more effective inducing resolution in patients more than 45 years compared to MP (p = 0.036). When we compare both groups after 3 months of treatment, there was no statistically significant difference in BMI, total cholesterol, HDL, LDL and fibrinogen level between two groups. The rate of patients without any side effects was found to be similar in both groups (p = 0.5).
Conclusion
LYN which is a synthetic progestin ensures better endometrial control compared to MP in simple hyperplasia without atypia in the patients of premenopausal age especially in ages more than 45 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endometrial hyperplasia (EH) is characterized by an excessive proliferation of endometrial glands that may progress to or coexist with endometrial carcinoma of endometrioid histology [1]. It may present with abnormal uterine bleeding and always results from chronic estrogenic stimulation unopposed by the counterbalancing effects of progesterone. International Society of Gynecological Pathologists (ISGP) and World Health Organization (WHO) classification system for endometrial hyperplasia has been developed based on the complexity of endometrial glands and cytologic atypia. The endometrial hyperplasias are classified as simple or complex, with or without atypia [2]. The progression rate of simple and complex hyperplasia to endometrial carcinoma is 1 and 3 %, respectively, with a mean duration to progression of approximately 10 years [3]. However, simple atypical and complex atypical hyperplasia were reported to progress in 8 and 29 % of cases, respectively, with a mean duration to progression of 4.1 years [3]. Thus, the risk of progression of hyperplasia into endometrial carcinoma is closely related to the presence of cytologic atypia and to architectural crowding, and optimal treatment of endometrial hyperplastic lesions is essential to prevent endometrial cancer development.
Treatment options of simple EH include sole observation, treatment with progestins and surgery [4]. For simple EH cases, progestins have been used to prevent progression towards endometrial cancer and to control abnormal uterine bleeding. Progestins are effective on EH by activation of progesterone receptors, which results in stromal decidualization and subsequent thinning of the endometrium. Besides, progestin exposure decreases estrogen and progesterone receptors and activates hydroxylase enzymes to convert estradiol to its less active metabolite estrone. But, there is no consensus on dose, duration of treatment, administration route, and type of progestin that is most effective in the literature [5]. The most commonly used synthetic progestins have been associated with metabolic (e.g., induce significant disturbances in lipid levels, and glucose metabolism) and vascular side effects in controlled studies [6, 7]. The micronized progesterone (MP) administered orally has been shown to be as effective as the synthetic progestins for endometrial protection, but has significantly fewer metabolic side effects [8].
The objective of this prospective randomized follow-up study was to compare the effectiveness and tolerability of MP and lynestrenol (LYN) regimens for treatment of simple endometrial hyperplasia without atypia.
Methods
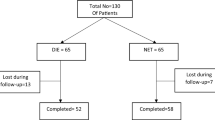
The study was approved by the local ethics committee of Etlik Zubeyde Hanim Women’s Health Research Hospital and informed consent was obtained from all the patients before the treatment. Out of the premenopausal patients applied to our hospital’s Gynecology Clinic in between the dates August 2009 and July 2011 with the complaint of abnormal uterine bleeding and performed to endometrial sampling and diagnosed with histologically documented simple EH without atypia were included in the study. Premenopausal status was defined by ongoing menstrual cycle for at least 6 months before inclusion. All participants underwent transvaginal ultrasound scanning to exclude the presence of other pathologies. Gynecologic pathologists assessed the histological samples and classified them using the WHO classification of EH [9]. Women with atypical hyperplasia or complex hyperplasia, treated with hormones in the previous 6 months and with associated pathologies of the endometrial cavity were excluded from the study. Participants were randomized into two groups based on computer-generated codes: Group I included 30 patients who received LYN in a dose of 15 mg three times daily for 12 days between the 14th and 25th day of the menstrual cycle for 3 months, while Group II included 30 patients who received MP 200 mg/d for 12 days between the 14th and 25th day of the menstrual cycle for 3 months. Three months from the start of treatment, follow-up endometrial curettage using Karman cannula was performed. Response to treatment based on histopathology of endometrial findings was classified as normal or hyperplastic. Normal endometrium was divided into functional (proliferative or secretory) or inactive/atrophic endometrium pattern. The ones diagnosed as secretory or inactive endometrium pattern were accepted as resolution while the ones diagnosed as proliferative endometrium pattern were accepted as regression. As per our clinical protocols, the cases considered as regression were planned to continue the treatment for another 3 months and then underwent endometrial curettage. Patients diagnosed with resolution by the same pathologists discontinued medical therapy and were followed every 3 months with transvaginal ultrasonography. Women diagnosed with persistence were offered same medication for another 3 months and were then reevaluated with endometrial curettage. Hysterectomy was performed if there was histological evidence of progression of EH to atypia or if there was no histological evidence of complete regression following a total of 6 months treatment. The primary outcome of the study was the proportion of patients requiring further treatment for 3 months.
Statistical analyses were performed using SPSS 17 (SPSS Inc. Chicago, IL, USA) programme and p < 0.05 was defined as significant. Categorical variables are presented as percentages and continuous variables are presented as mean followed by standard deviation and median with maximum–minimum. The normality of the variables was tested with Kolmogorov–Smirnov test. For statistical analysis, independent samples t test and Mann–Whitney U test were used to compare two groups. Paired sample t test and Wilcoxin signed rank test were used to test drug effects. Comparison of variables was performed by Pearson Chi-square test for categorical variables.
Results
The mean age, body mass index (BMI), endometrial thickness (ET), hemoglobin level, lipid parameters and fibrinogen levels in both groups in the beginning of the study showed no significant differences, as shown in Table 1.
After 3 months of treatment in both groups, none of the cases progressed. In LYN group, the rate of resolution was observed to be higher compared to MP group (p = 0.045; OR 3.33, 95 % CI 1.10–11.13). The patients treatment outcomes according to the results of endometrial histopathology are shown in Table 2.
When we compare the effects of drugs in different age groups, although there was no statistically significant difference between two groups under the age of 45 years, LYN was found more effective inducing resolution in patients more than 45 years compared to MP (p = 0.036; OR 6.1, 95 % CI 1.02–36.89). The comparison of the effectiveness of treatment method in different age groups is shown in Table 3.
When we compare both groups after 3 months of treatment there was no statistically significant difference in BMI, total cholesterol, HDL, LDL and fibrinogen level between two groups (p = 0.32; p = 0.3; p = 0.7; p = 0.16; p = 0.9, respectively). Endometrial thickness after LYN treatment was found 8.1 ± 2.3 mm while ET after MP treatment was found 9.5 ± 4.6 mm (p < 0.001). As a result, both drugs were found effective on endometrium by reducing endometrial thickness.
The most common side effect was abdominal bloating in 63 % of the cases using LYN (n = 19), while in MP group, 66.7 % of the cases (n = 20) fatigue was observed. There were six patients having any side effects in LYN group (20 %); in MP group no side effects were found out in five patients (17 %). The rate of patients without any side effects was found to be similar in both groups (p = 0.5).
Discussion
The regression rate of simple hyperplasia in different studies was given as 74–80 % with as 1 % progression rate [1, 3, 10]. In our study, as a result of 3 months gestagen treatment, glandular atrophy and stromal decidualization defined as complete resolution was found in 72 % of a total 60 cases without any case of progression. It was stated in the study performed by Kurman and colleagues that is accepted as an important source regarding the natural history of EH, the spontaneous regression rate for 93 simple EH cases followed at least for 1 year without treatment was 80 % while the persistence rate was 18 % [3]. We observed higher level of resolution rate in LYN group compared to MP group (83.3 % for LYN vs. 60 % for MP, respectively) and LYN was especially effective in patients more than 45 years of age (83.3 % for LYN vs. 60 % for MP, respectively).
Investigations using animal models have evaluated the ability of progestins to transform the endometrium, as assessed by the McPhail Index. Accordingly, when comparative potency of progestogens was evaluated, it was seen that LYN which is a synthetic progestin from the estranes sub-group of 19-nortestosterone’s was more potent than natural progesterone [11]. Since micronized formulation of natural progesterone, ensures optimal progesterone bioavailability, has been shown to be as effective as the synthetic progestins for controlling endometrial growth with significantly fewer metabolic side effects in several studies [8, 12]. The effect of orally administered MP in different doses on endometrial cell cycle has been evaluated especially on postmenopausal women primed with estrogens [8, 13]. In these studies, progressive reduction in endometrial mitotic activity was reported using MP 200–300 mg/d for 10–12 days [8, 13]. The studies about the use of MP for EH have been carried out on postmenopausal women with higher metabolic and cardiovascular risks [14]. There are limited number of studies which investigate the effectiveness of MP in women diagnosed with EH in premenopausal period [15–17]. In an old study carried out on 80 premenopausal women applied with the complaint of dysfunctional bleeding, half of the cases with cystic glandular endometrial hyperplasia. In this study, the use of 300 mg/d MP orally for 10 consecutive days during the second half of the cycle was found effective in avoiding the endometrial hyperplasia recurrence [15].
In our study, we compared the effectiveness of LYN and MP for the treatment simple EH in premenopausal women and LYN was found to be more effective on inducing resolution especially in patients more than 45 years of age which may be due to the presence of less intrinsic progesteron in this age group. Although the short follow-up time and small sample size are considered to be the limitations of the study, our study is the first study showing effects of drugs in different age group. In a current study, premenopausal women diagnosed with simple hyperplasia without atypia were treated orally either with 10 mg/d medroxyprogesterone acetate (MPA), 15 mg/d LYN or 15 mg/d norethisterone (NET) for 10 days between the 16th and 25th day of the menstrual cycle for a period of 3 months [16]. Although the resolution rates were determined to be lower than our findings, the highest resolution rate was reported in LYN group, similar to our study.
One of the concerns about the synthetic progestins is having higher frequency of side effects due to intrinsic antimineralocorticoid and androgenic effects. In our study, there is no patient discontinued the treatment due to side effects and the rate of patients having no side effects was found to be similar in both groups. We observed lower levels of both HDL and TG after 3 months of treatment in LYN group. Although less side effects and negative effects on carbohydrate/lipid metabolism were reported with MP in a study [18], we could not find any difference on lipids parameters after 3 months of treatment in MP group. We observed reduction of BMI in MP group which may be important.
As a result, LYN which is a synthetic progestin ensures better endometrial control compared to MP in simple hyperplasia without atypia in the patients of premenopausal age especially in ages more than 45 years.
References
Montgomery B, Daum G, Dunton C (2004) Endometrial hyperplasia: a review. Obstet Gynecol Surv 59:368–378
Silverberg SG, Kurman RJ (1992) Tumours of the uterine corpus and gestational trophoblastic disease. Armed Forces Institute of Pathology, Washington DC
Kurman RJ, Kaminski PF, Norris HJ (1985) The behavior of endometrial hyperplasia. a long-term study of “untreated” hyperplasia in 170 patients. Cancer 56:403
Haimovich S, Checa MA, Mancebo G, Fusté P, Carreras R (2008) Treatment of endometrial hyperplasia without atypia in perimenopausal and postmenopausal women with a levonorgestrel intrauterine device. Menopause 15:1002–1004
Ferenczy A, Gelfand M (1989) The biologic significance of cytologic atypia in progesteron-treated endometrial hyperplasia. Am J Obstet Gynecol 160(1):126–131
Sullivan JM, Shala BA, Miller LA, Lerner JL, McBrayer JD (1995) Progestin enhances vasoconstrictor responses in postmenopausal women receiving estrogen replacement therapy. J N Am Menopause Soc 2:193–199
Clarkson TB, Hughes CL, Klein KP (1995) The nonhuman primate model of the relationship between gonadal steroids and coronary heart disease. Prog Cardiovasc Dis 280:605–613
de Lignieres B (1999) Oral micronized progesterone. Clin Ther 21(1):41–58
Scully RE, Bonfiglio TA, Kurman RJ, Silverberg SG, Wilkinson EJ (1994) Uterine corpus. In: Scully RE, Poulsen HE, Sobin LH (eds) Histological typing of female genital tract tumours, 2nd edn. Springer, New York, p. 13
Tabata T, Yamawaki T, Yabana T, Ida M, Nishimura K, Nose Y (2001) Natural history of endometrial hyperplasia. Study of 77 patients. Arch Gynecol Obstet 265:85–88
Schindler AE, Campagnoli C, Druckmann R, Huber J, Pasqualini JR, Schweppe KW, Thijssen JH (2003) Classification and pharmacology. Maturitas 10(46 Suppl 1):S7–S16
Grady D, Ernster VL (1997) Hormone replacement therapy and endometrial cancer: are current regimens safe? J Natl Cancer Inst 98:1088–1089
Lane G, Siddle NC, Ryder TA, Pryse-Davies J, King RJ, Whitehead MI (1983) Dose dependent effects of oral progesterone on the oestrogenised postmenopausal endometrium. BMJ 287:1241–1245
Jondet M, Maroni M, Yaneva H, Brin S, Peltier-Pujol F, Pelissier C (2002) Comparative endometrial histology in postmenopausal women with sequential hormone replacement therapy of estradiol, and either chlormadinone acetate or micronized progesterone. Maturitas 41(2):115–121
Saarikoski DS, Yliskoski M, Penttila I (1990) Sequential use of norethisterone and natural progesterone in pre-menopausal bleeding disorders. Maturitas 12:89–97
Ozdegirmenci O, Kayikcioglu F, Bozkurt U, Akgul MA, Haberal A (2011) Comparison of efficacy of three progestins in the treatment of simple endometrial hyperplasia without atypia. Gynecol Obstet Invest 72:10–14
El-Shamy M, Gibreel A, Refai E, Sadek E, Ragab A (2012) Aromatase inhibitor “letrozole” versus progestin “norethisterone” in women with simple endometrial hyperplasia without atypia: a prospective cohort trial. Middle East Fertil Soc J 17:111–115
Simon JA, Cedars MI, Langer RD (2007) Uses of progesterone throughout a woman’s life. J Fam. Pract. 56(2 Suppl):S33–S56
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tasci, Y., Polat, O.G., Ozdogan, S. et al. Comparison of the efficacy of micronized progesterone and lynestrenol in treatment of simple endometrial hyperplasia without atypia. Arch Gynecol Obstet 290, 83–86 (2014). https://doi.org/10.1007/s00404-014-3161-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3161-4