Abstract
Purpose
The vast majority of the evidence on the prevalence of malignancy in endometrial polyps was obtained irrespectively of the time of diagnosis, i.e. including both women who were diagnosed at pre-surgical ultrasound and those who were diagnosed at the time of hysteroscopy. We hypothesize that this may represent an inaccuracy of potential clinical relevance since physicians have to take decisions regarding the need of surgery at the time of ultrasound diagnosis.
Materials and methods
Medical records of 2,245 patients who underwent hysteroscopy during a 4-year period were reviewed. Inclusion criterion was a pre-operative diagnosis of endometrial polyps.
Results
1,284 women (57 % of the cohort) were selected, of whom 36 were diagnosed with malignancies (2.8 %, 95 % CI 2.0–3.8). This prevalence markedly differ in pre- and post-menopause, being higher in the latter group (OR = 9.0, 95 % CI 2.6–30.3, p < 0.001). Six out of 803 resulted positive in the pre-menopausal group (0.7 %, 95 % CI 0.3–1.5) compared to 30 out of 481 in the post-menopausal group (6.2 %, 95 % CI 4.3–8.6). In the pre-menopausal group, a younger age resulted protective. The risk of malignancy in women younger than 50 years was 0.3 % (95 % CI 0.04–0.9). In the post-menopausal group, abnormal uterine bleeding (AUB) was associated with a diagnosis of malignancy (OR = 4.0, 95 % CI 1.9–8.5). The prevalence of malignancy in symptomatic and asymptomatic post-menopausal women was 11.8 % (95 % CI 7.6–17.1) and 3.0 % (95 % CI 1.4–5.3), respectively.
Conclusions
The prevalence of malignancy among endometrial polyps detected at ultrasound is low and in line with the evidence obtained for a diagnosis made at the time of surgery. Some simple anamnestic information such as menopausal status, age and AUB helps identify women at higher risk and should be used in the decision-making process guiding the choice of surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ruling out malignancy is claimed as a critical aspect in the management of women who are diagnosed with endometrial polyps. Hysteroscopic resection of these lesions has commonly slipped into clinical practice even in asymptomatic women to remove a lesion whose malignant potential is judged to be low but not rare [1]. However, evidence to support this cautious attitude is lacking. Of relevance here is that the prevalence of asymptomatic polyps is considerable. Pathological series reported a prevalence in post-menopause of up to 20 % [2]. This aspect is now assuming growing relevance because, in some western countries, there is a sort of natural endometrial screening in asymptomatic patients [2]. The wild use of transvaginal ultrasound combined with the enhanced accuracy of the available instruments is inevitably entailing a significant increase in the number of women diagnosed with endometrial polyps. The financial costs and the psychological burden of a policy of systematic screening and removal of endometrial polyps are huge and evidence to support its implementation is currently lacking.
In a recent meta-analysis including 17 studies, the prevalence of malignancy in endometrial polyps was 3.6 % (95 % CI 3.2–3.9) [1]. Abnormal uterine bleeding after menopause was associated with an enhanced risk and hysteroscopy is consistently deemed appropriate in these cases. In contrast, the prevalence among asymptomatic patients (2.2 %, 95 % CI 1.7–2.6) and pre-menopausal women (1.7 %, 95 % CI 1.3–2.1) is of debatable clinical relevance [1]. However, the available evidence may be questioned because most studies reporting on the prevalence of malignancy referred to a diagnosis of endometrial polyps made at the time of hysteroscopy and not to the diagnosis made at the time of ultrasound assessment. This point has to be considered as a potential relevant limitation since, in clinical practice, physicians have to face women with an ultrasound rather than an hysteroscopic diagnosis of polyps and the prevalence of malignancy in these two situations may differ. To our knowledge, only two small studies specifically reported data on women who were diagnosed with endometrial polyps at ultrasound or hysterosonography and data were conflicting (Table 1) [3, 4].
To further elucidate this aspect, we herein present data from a large series of women who underwent hysteroscopy based on a pre-surgical diagnosis of endometrial polyps. The primary aim was to assess the frequency of malignancy. The secondary aim was to identify risk factors for this condition.
Materials and methods
Medical records of patients who underwent hysteroscopy at the day surgery unit of the Obstetrics and Gynecological Department of the Fondazione IRCSS Ca’ Granda Ospedale Maggiore Policlinico from 1 January 2007 to 31 December 2010 were reviewed. Medical records of 2,245 patients were retrieved. Inclusion criterion was a pre-operative diagnosis of endometrial polyps. Patients with endometrial polyps detected during operative hysteroscopy, but not previously suspected at ultrasound were excluded. Women who were diagnosed with focal or diffuse endometrial thickening or with polypoid endometrium and those with a previous diagnosis of endometrial hyperplasia were also excluded.
The recorded variables were as follows: age, BMI, menopausal status, hormonal therapy (estroprogestins, tamoxifene), diagnosis of hypertension or diabetes mellitus, hormone replacement therapy (HRT) (in menopausal women), symptomatology, pre-operative ultrasound and hysterosonographic findings, hysteroscopic diagnosis, histological examination. Abnormal uterine bleeding (AUB) was defined as any kind of vaginal bleeding in post-menopause and as irregular vaginal bleedings in patients who menstruated or had hormone therapy. Menopausal status was mainly based on anamnestic data. For doubtful cases, serum FSH was tested twice and we applied the classical definition of menopause, i.e. absence of menstruation for a period of at least 12 months and value of serum FSH >40 UI/ml in at least two blood samples at a distance of over 1 month.
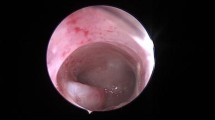
According to the policy of our unit, women with all sorts of AUB (hypermenorrhea, menorrhagia, intermenstrual vaginal bleedings, post-menopausal vaginal bleeding) are referred for transvaginal ultrasound examination and hysterosonography. Hysterosonography was also performed in asymptomatic women who were detected some endometrial abnormalities at basal ultrasound.
Operative hysteroscopic procedures were performed in day surgery under local or general anesthetic; polyp removal was performed through resectoscopic slicing with bipolar or monopolar handle or through operative office hysteroscope and polyp removal by small scissors. Endometrial biopsy was systematically performed. All removed specimen were sent for histological examination. Histological findings were considered positive for malignancy if revealing carcinoma or atypical hyperplasia [1, 5].
Statistical analyses were performed using the statistical package SPSS 18.0 (IL, USA). Data were compared using the Student’s t test or the Fisher Exact test, as appropriate. A p value below 0.05 was considered statistically significant. An a priori sample size calculation was not performed. A binomial distribution model was used to determine the 95 % confidence interval (95 % CI) of proportions.
Results
During the study period, 1,284 women were meant to undergo operative hysteroscopy with an ultrasound diagnosis of endometrial polyps. They constituted 57 % of all the hysteroscopic interventions performed. Among them, 481 (38 %) were post-menopausal (average duration of menopause 12 ± 8 years), whereas 803 were pre-menopausal (62 %). The mean ± SD age of all cohort was 50 ± 12 years (range 20–84 years). The mean ± SD BMI was 24.3 ± 5.0 kg/m2. Altogether, 615 patients (48 %) had AUB whereas 669 (52 %) were asymptomatic.
Post-surgical histological diagnoses are depicted in Table 2. The diagnosis of benign polyps (including those with hyperplasia without atypia) was confirmed in 985 cases (76 %). In 159 women (12 %) findings were unremarkable (normal or atrophic endometrium). Considering malignancy according to our definition (carcinoma or atypia), 36 women had a positive diagnosis. The prevalence of malignancy was thus 2.8 % (95 % CI 2.0–3.8). If excluding cases with atypia (n = 11), the prevalence dropped to 1.9 % (95 % CI 1.3–2.8). In nine out of these 25 women with carcinoma, hysteroscopy confirmed the presence of the described polyp. In seven of them, the carcinoma was confined to the polyp.
The prevalence of malignancies markedly differ in pre- and post-menopause (p < 0.001). Six out of 803 resulted positive in the pre-menopausal group (0.7 %, 95 % CI 0.3–1.5) compared to 30 out of 481 in the post-menopausal group (6.2 %, 95 % CI 4.3–8.6). The corresponding OR for malignancy was 9.0 (95 % CI 2.6–30.3). Given this marked discrepancy, it was deemed more appropriate to perform the analysis for risk factors separately for these two conditions. Results are illustrated in Table 3. Considering women in pre-menopause, affected women resulted significantly older than those carrying benign diagnoses. In fact, four out of the six cases occurred in women aged more than 50 years. The prevalence of malignancy in pre-menopausal women younger than 50 years was 0.3 % (95 % CI 0.04–0.9) (2 out of 709 women). In those younger than 40 years, it was 0.0 % (95 % CI 0.0–1.0) (0 out of 303 women). The other clinical variables did not significantly differ between the study groups. In post-menopause, age was not a significant factor. In contrast, AUB was markedly associated with a diagnosis of malignancy. The OR of malignancy in post-menopausal women with AUB was 4.0 (95 % CI 1.9–8.5). In fact, the prevalence of malignancy in symptomatic and asymptomatic post-menopausal women was 11.8 % (95 % CI 7.6–17.1) and 3.0 % (95 % CI 1.4–5.3), respectively.
Comment
The ultrasonographic demonstration of an endometrial polyp may harbor a malignancy. The present study confirms that this situation, albeit rare, is possible. In fact, the prevalence of malignancy for the whole cohort was 2.8 % (95 % CI 2.0–3.8). This rate was lower (1.9 %, 95 % CI 1.3–2.8) if excluding cases with only atypia. Our results did not differ from those reported by the recent large meta-analysis including all women with endometrial polyps irrespectively of the time of diagnosis (i.e. pre-surgical or surgical). In that analysis, the prevalence of malignancy (carcinoma and atypia) was indeed 3.6 % (95 % CI 3.2–3.9) [1].
Our results also emphasize that the rate of malignancy varied according to the clinical characteristics of the women. It is an exceedingly rare event before the advent of menopause (0.7 %, 95 % CI 0.3–1.5) and becomes even rarer in the subgroup of pre-menopausal women younger than 50 years (0.3 %, 95 % CI 0.04–0.9). Moreover, even if the risk is generally higher in the post-menopausal group (6.2 %, 95 % CI 4.3–8.6), the use of a simple anamnestic information on symptoms helps discriminate between those with AUB who are at enhanced risk (11.8 %, 95 % CI 7.6–17.1) and the asymptomatic women who are at lower risk (3.0 %, 95 % CI 1.4–5.3). Again, these results are in line with previous evidence on this topic obtained from the whole population of women with endometrial polyps, i.e. those who were diagnosed with the lesion at ultrasound and/or at hysteroscopy. In their meta-analysis, Lee et al. [1] also noted a higher risk in post-menopause (Relative Risk-RR = 3.9, 95 % CI 2.9–5.1) and in women with AUB (RR = 2.0, 95 % CI 1.2–3.1). Noteworthy, the magnitude of the impact of these two variables was more evident in our series. Of further interest here is the observation that, in our study, AUB was not associated with malignancy in pre-menopause.
From a clinical point of view, our results support the possibility of expectant management in young pre-menopausal women. Surgical removal is mandatory in women seeking pregnancy because of the well-known detrimental impact on embryo-implantation and the demonstrated benefits of surgery [6]. In contrast, in asymptomatic women not seeking pregnancy, expectant management is indicated. Of relevance here is that spontaneous resolution of polyps is not uncommon in this age group [7]. In contrast, after menopause, hysteroscopic removal is mandatory for symptomatic women. In this group, one out of ten women was found to carry a malignancy. In contrast, we claim expectant management for asymptomatic post-menopausal subjects for several reasons. First, the risk of malignancy is low (3.0 %, 95 % CI 1.4–5.3 %). Secondly, albeit it is generally deemed that diagnosis before the advent of symptoms may have a favorable impact on the prognosis, this dogma remains to be demonstrated. Noteworthy, the prognosis of women with endometrial cancer does not markedly differ between those who did and did not report AUB at the time of the diagnosis [8–10]. Finally, this age group may be exposed to a higher risk of surgical complications, in particular in elderly women.
Enlarging the proportion of women with endometrial polyps to be treated expectantly represents a challenging new task, but it is mandatory. The clinical and financial burden of a policy of systematic surgery is huge. In our experience, endometrial polyps constituted 57 % of all the hysteroscopic interventions performed, corresponding to more than 300 interventions per year. The financial impact of this indication is considerable, the waiting list is exceedingly long and the organization of the service is rather complex. This situation is mainly consequent to the widespread diffusion and systematic use of transvaginal ultrasound. The regular use of this diagnostic tool in a preventive perspective has entered into clinical practice despite the lack of scientific evidence. Even more, it has recently emerged that this habit may be even detrimental [11, 12]. Finally, one has to wonder about the cost-effectiveness profile of a policy of systematic hysteroscopy aimed at early identification of endometrial cancer. This kind of analysis is beyond the scope of the present study but warrants evaluation given the low prevalence of the condition.
Strengths of this study are the large sample size that allowed us for a precise estimate of the rate of malignancy also in subgroup analyses. On the other hand, the number of included women may be insufficient for the analyses on risk factors, in particular in the pre-menopausal group because of the rarity of the malignancies. Among the limitations of the study it must be also acknowledged that the study was retrospective and some potential important characteristics of the women are missing. In particular, detailed data on the sonographic aspect of the polyps are lacking. We did not include this variable in our analysis since ultrasounds were performed by a large number of physicians and a precise policy for endometrial polyps description was not part of our routine clinical practice. Interestingly, Ferrazzi et al. [2] reported that a larger diameter of the polyp may be of relevance, at least in asymptomatic post-menopausal women. The OR of malignancy for polyps with mean diameter >18 mm was 6.9 (95 % CI 2.2–21.4). In a small cohort study, the additional use of Doppler evaluations did not help identify women with malignant lesions [3]. Nevertheless, this area of research may be of great interest since it may consent to identify a subgroup of women at enhanced risk who would actually benefit from surgery. Future large prospective studies are warranted to identify sonographic variables able to predict malignancy.
In conclusion, our results do not support our initial concern. The frequency of malignancy among endometrial polyps detected at transvaginal ultrasound did not differ from previous data obtained irrespectively to the time of diagnosis. Moreover, our data confirmed that this risk is associated to menopausal status and to the presence of symptoms. It peaks in post-menopausal women with AUB. On these bases, we consider that surgery should be indicated in post-menopausal women with AUB while expectant management should be envisaged in pre-menopause and in asymptomatic post-menopausal women. Finally, given the rarity of malignancies and the lack of supporting evidence, a policy of systematic screening for endometrial polyp is currently unjustifiable.
References
Lee SC, Kaunitz AM, Sanchez-Ramos L, Rhatigan RM (2010) The oncogenic potential of endometrial polyps: a systematic review and meta-analysis. Obstet Gynecol 116:1197–1205
Ferrazzi E, Zupi E, Leone FP, Savelli L, Omodei U, Moscarini M, Barbieri M, Cammareri G, Capobianco G, Cicinelli E, Coccia ME, Donarini G, Fiore S, Litta P, Sideri M, Solima E, Spazzini D, Testa AC, Vignali M (2009) How often are endometrial polyps malignant in asymptomatic postmenopausal women? A multicenter study. Am J Obstet Gynecol 200:235.e1–235 e6
Goldstein SR, Monteagudo A, Popiolek D, Mayberry P, Timor-Tritsch I (2002) Evaluation of endometrial polyps. Am J Obstet Gynecol 186:669–674
Dreisler E, Stampe Sorensen S, Ibsen PH, Lose G (2009) Prevalence of endometrial polyps and abnormal uterine bleeding in a Danish population aged 20–74 years. Ultrasound Obstet Gynecol 33:102–108
Bergeron C, Nogales FF, Masseroli M, Abeler V, Duvillard P, Müller-Holzner E, Pickartz H, Wells M (1999) A multicentric European study testing the reproducibility of the WHO classification of endometrial hyperplasia with a proposal of a simplified working classification for biopsy and curettage specimens. Am J Surg Pathol 23:1102–1108
Bosteels J, Weyers S, Puttemans P, Panayotidis C, Van Herendael B, Gomel V, Mol BW, Mathieu C, D’Hooghe T (2010) The effectiveness of hysteroscopy in improving pregnancy rates in subfertile women without other gynaecological symptoms: a systematic review. Hum Reprod Update 16:1–11
DeWaay DJ, Syrop CH, Nygaard IE, Davis WA, Van Voorhis BJ (2002) Natural history of uterine polyps and leiomyomata. Obstet Gynecol 100:3–7
Gerber B, Krause A, Müller H, Reimer T, Külz T, Kundt G, Friese K (2001) Ultrasonographic detection of asymptomatic endometrial cancer in postmenopausal patients offers no prognostic advantage over symptomatic disease discovered by uterine bleeding. Eur J Cancer 37:64–71
Kimura T, Kamiura S, Yamamoto T, Seino-Noda H, Ohira H, Saji F (2004) Abnormal uterine bleeding and prognosis of endometrial cancer. Int J Gynaecol Obstet 85:145–150
Seebacher V, Schmid M, Polterauer S, Hefler-Frischmuth K, Leipold H, Concin N, Reinthaller A, Hefler L (2009) The presence of postmenopausal bleeding as prognostic parameter in patients with endometrial cancer: a retrospective multi-center study. BMC Cancer 9:460
Moyer VA (2012) What we don’t know can hurt our patients: physician innumeracy and overuse of screening tests. Ann Intern Med 156:392–393
Jacobs I, Gentry-Maharaj A, Burnell M, Manchanda R, Singh N, Sharma A, Ryan A, Seif MW, Amso NN, Turner G, Brunell C, Fletcher G, Rangar R, Ford K, Godfrey K, Lopes A, Oram D, Herod J, Williamson K, Scott I, Jenkins H, Mould T, Woolas R, Murdoch J, Dobbs S, Leeson S, Cruickshank D, Skates SJ, Fallowfield L, Parmar M, Campbell S, Menon U (2011) Sensitivity of transvaginal ultrasound screening for endometrial cancer in postmenopausal women: a case-control study within the UKCTOCS cohort. Lancet Oncol 12:38–48
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uglietti, A., Mazzei, C., Deminico, N. et al. Endometrial polyps detected at ultrasound and rate of malignancy. Arch Gynecol Obstet 289, 839–843 (2014). https://doi.org/10.1007/s00404-013-3037-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-013-3037-z