Abstract
Objective
To assess the detection of Human Papillomavirus (HPV) in cervical biopsies, and its association with clinical response and survival of patients with cervical cancer.
Method
The presence of HPV was determined by polymerase chain reaction (nested PCR) of material from 183 paraffin blocks containing biopsies of patients with cervical cancer. Directives of the International Federation of Gynecology and Obstetrics (FIGO) were used for the clinical staging of all cases. Survival analysis was conducted with the Kaplan–Meier method and differences between the curves were calculated by the log-rank test.
Results
Amplification was positive in 78 cases, negative in 96 cases and indeterminate in 9. The detection of HPV had no statistically significant effect on the survival of patients.
Conclusions
From amongst the variables analyzed, only HPV positivity and clinical staging influenced a complete response after completing treatment. However, clinical staging was the only factor associated with progression of the disease, with patients in the early stages presenting better overall survival rates (p < 0.001).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer is the second most frequent malignancy and the third cause of cancer-related death in women, representing 8 % of female cancer deaths worldwide [1]. In developed countries, its mortality has been on the decline over recent decades, due to secondary prevention obtained with screening tests such as Pap smears [2, 3]. The direct association of the appearance of this tumor with infection from Human Papillomavirus (HPV) is well known. So far, more than 100 subtypes of HPV have been described and in general, genital tract infection caused by the virus regresses spontaneously, without any type of treatment [4, 5]. The persistence of HPV for 6 months or more is encountered in older patients, those infected with multiple viral subtypes and with potentially high-risk oncogenic subtypes, especially viral subtypes 16 and 18 [6]. In patients with cervical cancer, failure to detect the virus in the tumor, the viral subtype and the presence of the HPV DNA in the lymph nodes free of cancer are considered factors for poor prognosis [7–9]. With regard to the treatment of this neoplasia, very few significant changes have occurred over the recent years and treatment consists of surgery in the early stages, with radiotherapy or chemotherapy combined with radiotherapy reserved for high-risk early tumors or advanced disease [10].
Materials and methods
Clinico-pathological data
The study population comprised 183 patients with invasive cervical cancer, treated at the Oncology Unit at the Universidade de Pernambuco. This group represents 53 % of all women with this disease, who were treated during the period from January 2000 to December 2009, and is made up of patients whose biopsies, performed before oncology treatment and embedded in paraffin blocks, were available. The directives of FIGO (The International Federation of Gynecology and Obstetrics) were used for clinical staging (CS), where CS III was found to be the most frequent (48 %). In addition to clinical staging and testing for HPV, the following variables were also assessed in relation to the development of the disease: age, histological type and histological grade. A total of 143 patients received oncology treatment, 41 of whom were submitted to surgery and 120 (65 %) received an external radiation dose of 49 Gy for 8 weeks, with an average of 4 fractions of brachytherapy using a fractional dose of 27 Gy. Twenty-two patients received chemotherapy combined with radiotherapy, with a weekly dose of either cisplatin 40 mg/m² or cisplatin 70 mg/m² D1 and fluorouracil 1,000 mg/m2 D1 to D4, each 21 days. On completion of treatment, a complete response (CR) was considered if, after reassessing patient clinical, histological and imaging status, there was no local or distant disease, and a non-complete response (NCR) when there was residual or metastatic disease.
The Chi-squared test was used to analyze the associations between the categorized variables. The survival curves were constructed using the Kaplan–Meier method. Comparison of the curves was performed with the log-rank test and the adopted level of significance was 0.05. The statistical analyses were conducted with Stata 12.1SE. The study was authorized by the institution’s Ethics Committee.
Viral study
Paraffin blocks with cervical tissue were sectioned into 3–5 μm. Xylene was added to the paraffinized tissue in order to remove the paraffin and then 100 % ethanol was used to remove any traces of xylene from the studied tissue. The ethanol was air-dried and the tissue was homogenized with 20 μL of 20 % SDS, 80 μL buffer (NaCl 0.375 M, EDTA 0.12 M, pH 8.0), and 40 μL of proteinase K (10 mg/mL). Sterile water was added to the final volume of 380 μL. The tube containing the reaction was incubated at 55 °C for 16 h. After this, 100 μL of NaCl 6 M was added to the sample to precipitate the proteins by centrifugation at 10,000×g for 5 min. The supernatant was transferred to a new tube to which was added 1 mL of 100 % ethanol. The sample was centrifuged at 10,000×g for 5 min and the precipitate was washed in 70 % ethanol and evaporated in air. Finally, the precipitate was suspended in 50 μL TE buffer (Tris–Cl 10 mM, pH 8.0; EDTA 1 mM) and stored at less than 20 °C until the molecular test was conducted [11].
Oligonucleotides for β-actin genes were used as quality control for the extracted DNA. Samples were assessed for the presence of HPV using nested PCR with oligonucleotides MY09/11 (external) and GP5+/6+ (internal) [12, 13].
In the first phase, 1 μL of DNA was used, extracted from each patient, 1 μL MY09/11 (10 pmol each) and 12 μL of GoTaq Master Mix (Promega, USA). Ultrapure water was used in sufficient quantities to complete a final volume of 25 μL of the PCR reaction. The amplification program followed the following specifications: 95 °C for 2 min, 40 cycles of 95 °C for 1 min, 55 °C for 1 min and 72 °C for 1 min, followed by a final extension of 10 min at 72 °C and maintained at 4 °C. The nested PCR used 5 μL of the first phase to prepare the second phase, to which was added 1 μL GP5+/6+ (10 pmol of each). All other items were added to the same specification mentioned above.
Amplification was performed with the following specifications: 95 °C for 2 min and 40 cycles of 95 °C for 45 s, 48 °C for 45 s and 72 °C for 45 s. The final extension was 10 min at 72 °C, and the sample was maintained at 4 °C. The amplicons were visualized in 1 % agarose gel electrophoresis containing ethidium bromide as a fluorescent double-stranded DNA intercalator under an ultraviolet light. Ultrapure water was used as a negative control and plasmid pBR322-HPV16 was used as a positive control of the reaction. Results were classified as positive or negative, according to the presence or absence of HPV amplification in the sample. The term used in cases of viral amplification was indeterminate, but the control of β-actin was not positive.
Results
The mean age was 53 years, and the predominant histological type was squamous cell carcinoma (87 %). In 36 % of the biopsies, the tumor was moderately differentiated and 37 % did not receive this classification. There was a similarity regarding the origins of the patients (90 patients from the metropolitan region and 93 from the interior of the state). Human Papillomavirus tests resulted in 78 positive biopsies, 96 negative and 9 indeterminate. There was no association between the variables and the results of the HPV study (Table 1).
The median follow-up period of the studied group was 1.6 years, where 15 % of patients were monitored for more than 5 years. A total of 143 patients (78 %) received oncology treatment and of these, 131 (92 %) were assessed for response to treatment. In this aspect, the positive result of HPV and the clinical staging were the only factors associated to the response encountered after completing treatment (Table 2).
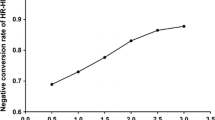
The survival graph demonstrates that, after a 5-year monitoring period, around 60 % of all patients were still alive (CI 95 % 51.8–73.1) and at the end of the study, half the patients were alive (CI 95 % 39.5–65.1) (Fig. 1).
The positive result obtained in the polymerase chain on the presence of Human Papillomavirus (HPV) in the cervical paraffin biopsies had no influence on overall patient survival (Fig. 2).
In the survival curves according to clinical staging, stages III and IV demonstrated a poor performance. There was a statistically significant association between clinical staging and survival (p < 0.001) (Fig. 3).
Discussion
When assessing the prognosis of cervical cancer, a number of clinico-pathological and epidemiological factors are commonly included in studies, such as age, smoking, histological type, histological grade, tumor size, lymphatic invasion, presence and subtype of detected HPV and even the type and form of treatment undertaken [14, 15]. The present study initially assessed data regarding age, histological type and grade and patient origins in relation to the amplification of HPV and afterwards to the clinical response. According to the results obtained, none of these variables were associated with detecting the virus, nor with progression of the disease.
Because it is a sexually transmitted disease, associated with HPV, it was expected that the virus would be more frequent in biopsies of patients from large urban centers, i.e., from the state capital and the metropolitan region. However, there was no significant association with the patients’ place of origin and the PCR result when testing for HPV.
In patients with cervical cancer, testing for HPV in biopsies of fresh cervical tissue resulted in detection and viral subtyping in around 90 % of all cases [16–19]. Despite reports of higher viral detection in some studies that have investigated the presence of the virus in paraffin-embedded biopsies, the viral amplification detected in the present study was only possible in 78 cases (43 %) with the use of nested PCR [20]. In this case, one reason for this difficulty could have been the time lapse between collecting material and performing the test, or technical factors, such as the condition of the biopsies and the quality of the inclusion material (paraffin). However, this difficulty was partly compensated for by conducting nested PCR, a more sensitive method than traditional PCR.
Similar to reports regarding carcinomas in the head and neck, the absence of Human Papillomavirus in cervical biopsies is also associated with poor prognosis [8, 9, 21]. In the present study, HPV positivity (p = 0.51) was associated with a complete response only in relation to the completion of treatment. When an assessment was undertaken in relation to the survival curves, viral detection had no influence on the course of the disease. The clinical staging established in the initial assessment was the only one to demonstrate an association with survival of the patient.
In conclusion, from amongst all the assessed prognostic factors, only the presence of HPV and advanced clinical staging influenced the clinico-pathological response after completing treatment, while in the survival analysis, staging was the only factor implicated in the progression of the disease.
References
Agência Internacional para Pesquisa do Câncer (2008) Estatística global do câncer, Organização Mundial da Saúde. http://globocan.iarc.fr/factsheet.asp. Accessed 10 Jan 2012
Instituto Nacional de Câncer José de Alencar Gomes da Silva (2011) Estimativa 2012: Incidência de Câncer no Brasil. Ministério da Saúde. http://inca.gov.br/estimativa/2012/estimativa20122011.pdf. Accessed 10 Jan 2012
Forouzanfar MH, Foreman KJ, Delossantos AM, Lozano R, Lopez AD, Murray CJL, Naghavi M (2011) Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis. Lancet 378:1461–1484
Federação Brasileira das Sociedades de Ginecologia e Obstetrícia (2002) Papilomavírus Humano (HPV): Diagnóstico e Tratamento. http://www.febrasgo.org.br/arquivos/diretrizes/079.pdf. Accessed 16 June 2010
Hellner K, Munger K (2011) Human Papillomaviruses as therapeutic targets in human cancer. J Clin Oncol 29:1785–1794
Ho GYF, Bierman R, Beardsley NP, Chang CJ, Burk RD (1998) Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med 338(7):423–428
Higgins GD, Uzelin DM, Philips GE, Davy M, Roder D, Burrell CJ (1991) Increased age and mortality associated with cervical carcinomas negative for human papillomavirus. Lancet 338(8772):910–913
Riou G, Bourhis J, Favre M, Orth G, Jeannel D, Le Doussal V (1990) Association between poor prognosis in early-stage invasive cervical carcinomas and non-detection of HPV DNA. Lancet 335(8699):1171–1174
Eifel PJ, Berek JS, Markman M (2011) Cancer of the cervix, vagina, and vulva. In: Devita VT Jr, Lawrence TS, Rosenberg SA (eds) Cancer principles and practice of oncology. Lippincott Williams and Wilkins, Philadelphia, pp 1311–1344
Ota T, Takeshima N, Tabata T, Hasumi K, Takizawa K (2007) Treatment of squamous cell carcinoma of the uterine cervix with radiation therapy alone: long-term survival, late complications, and incidence of second cancers. Brit J Cancer 97(8):1058–1062
Husman AMR, Walboomers JMM, van den Brule AJC, Meijer CJLM, Snijders PJF (1995) The use of general primers GP5 and GP elongated at their 3′ends with adjacent highly conserved sequences improves human papillomavirus detection by PCR. J Gen Virol 76:1057–1062
Haws ALF, He Q, Rady PL, Zhang L, Grady J, Hughes TK et al (2004) Nested PCR with the PGMY09/11 and GP5+/6+ prime sets improves detection of HPV DNA in cervical samples. J Virol Methods 122:87–93
Khan S, Jaffer NN, Khan MN, Rai MA, Shafiq M, Ali A et al (2007) Human papillomavirus subtype 16 is common in Pakistani women with cervical carcinoma. IJID 11:313–317
Haie-Meder C, Morice P, Castiglione M (2010) Cervical cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 21(5s):37–40
Cooke SL, Temple J, MacArthur S, Zahra MA, Tan LT, Crawford RAF et al (2011) Intra-tumor genetic heterogeneity and poor chemoradiotherapy response in cervical cancer. B J Cancer 104:361–368
Howell-Jones R, Bailey A, Beddows S, Sargent A, Silva N, Wilson G et al (2010) Multi-site study of HPV type-specific prevalence in women with cervical cancer, intraepithelial neoplasia and normal cytology, in England. BJC 103:209–216
Mayrand MH, Duarte-Franco E, Rodrigues I, Walter SD, Hanley J, Ferency A et al (2007) Human Papillomavirus DNA versus Papanicolaou screening tests for cervical cancer. N Engl J Med 357(16):1579–1588
Huang HJ, Huang SL, Lin CY, Lin RW, Chao FY, Chen MY et al (2004) Human papillomavirus genotyping by polymerase chain reaction-based genechip method in cervical carcinoma treated with neoadjuvant chemotherapy plus radical surgery. Int J Gynecol Cancer 14:639–649
Prétet JL, Jacquard AC, Carcopino X, Charlot JF, Bouhour D, Kantelip B et al (2007) Human Papillomavirus (HPV) genotype distribution in invasive cervical cancers in France: EDITH study. Int J Cancer 122:428–432
Huang LW, Chao SL, Hwang JL (2004) Human Papillomavirus-31-related types predict better survival in cervical carcinoma. Cancer 100(2):327–334
Fakhry C, Westra WH, Li S, Cmelak A, Ridge JA, Pinto H, Forastiere A, Gillison ML (2008) Improved survival for patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst 100:261–269
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barreto, C.L., Martins, D.B.G., de Lima Filho, J.L. et al. Detection of Human Papillomavirus in biopsies of patients with cervical cancer, and its association with prognosis. Arch Gynecol Obstet 288, 643–648 (2013). https://doi.org/10.1007/s00404-013-2803-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-013-2803-2