Abstract
Purpose
The literature includes a wealth of medical data on endometriosis, but the economic significance of the condition has so far been neglected. An analysis of hospital costs for endometriosis in Austria was, therefore, carried out for economic purposes.
Methods
Seventy-three patients with endometriosis were included in the study. A bottom-up approach was used to collect data on the average hospital costs of an endometriosis patient over a time period of 1 year. In addition, a prevalence approach was used that allows subsequent estimation of the total costs of endometriosis for the health-care system in Austria for that period. Retrospective questionnaire survey was conducted.
Results
The average annual costs of one case of endometriosis are €7,712, with €5,605.55 attributable to direct costs and €2,106.34 to indirect costs. This indicates an overall economic burden of €328 million. In-patient care (45 %) and loss of productivity (27 %) were identified as the major cost factors. The patients themselves pay for 13 % of the costs (through out-of-pocket payments).
Conclusions
This study impressively demonstrates the financial burden on the economy and on each individually affected patient caused by the disease of endometriosis. The massive consumption of resources represents a high level of usage of the medical services provided. The question arises as to whether more timely diagnosis, followed by better-targeted treatment, might have the potential to reduce these costs. The overall economic burden of endometriosis in Austria is currently comparable with that of Parkinson’s disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The fifth edition of the Euro Health Consumer Index [1] provides a user-focused, performance-related comparison of 33 national health-care systems. In this regularly published analysis of health-care systems in Europe, Austria came in fourth place among the 33 countries examined. One of the major diseases affecting populations in Europe is endometriosis, the second most frequent benign proliferative disease in women. It is estimated that approximately 7–15 % of women suffer from endometriosis [2]. According to the Austrian Statistical Office [3], the number of women of childbearing age (between 15 and 44 years) in 2009 was 1,703,442. If a prevalence of 5 % is assumed, this would mean that 85,172 women in Austria are affected by endometriosis. It is thought that 50 % of these women—i.e., 42,586 of the patients—require treatment due to their symptoms [4]. According to the European Institute for Women’s Health, 14 million women in Europe are affected by endometriosis [5]. Despite this, the cause of the condition has not yet been conclusively explained. The complex symptoms make the differential diagnosis difficult, and establishing the diagnosis takes an average of 10.4 years [6]. Studies on the costs arising as a result of the disease are nevertheless scarce, although it must be assumed that due to its chronic character, endometriosis is associated with a high level of resource consumption [4, 7, 8]. There is a lack of sufficient data regarding the indirect costs and productivity losses resulting from lost working hours. Furthermore, data on direct costs are also scarce due to interventions in cases of sterility [8]. As mentioned, the time between the appearance of the initial symptoms and a conclusive diagnosis averages 10.4 years—a period during which the affected patients endure a prolonged ordeal, associated with frequent visits to doctors, hospital stays, pain treatments (direct costs), and loss of the capacity to work (indirect costs).
For these reasons, the present study aimed to answer the following research questions: What are the direct and indirect costs of endometriosis in Austria and what diagnostic tools and treatments are most frequently used and what do they cost? What proportion of the costs is borne by social insurance bodies and what proportion by private payments?
Materials and methods
The method used was a retrospective questionnaire survey including 73 women suffering from endometriosis. One further inclusion criterion was that they must have compulsory health insurance coverage. This was a bottom-up approach to obtaining data on the average disease costs for one endometriosis patient over a period of 1 year. In addition, a prevalence approach was used that allows subsequent estimation of the overall costs of endometriosis for the health-care system in Austria for that period. Both tangible direct costs and tangible indirect costs were taken into account in calculating the disease costs. The response to the survey during the period from June 2011 to September 2011 consisted of 89 questionnaires, 73 of which (82 %) were almost fully completed and thus fully evaluable.
Data on the use of medical services were collected using the following parameters: Frequency of physician visits, of visits to a hospital outpatient department of in-patient hospital stays, including the length of stays in days; frequency of surgical procedures, including the type of surgery (laparotomy/laparoscopy) and the frequency of reimbursed medication use, including the proprietary name, dosage, period of administration and dosage scheme; and frequency of paid prescription fees, of self-paid treatment services and associated treatments because of infertility.
Enquiries about all resources consumed were made exclusively in relation to endometriosis. Fee regulations for physicians under contract with the provincial statutory health insurance companies in Austria were used to calculate costs for consultations with family practitioners, specialists in gynecology and obstetrics, and other specialist physicians.
Costs for one hospital outpatient case in a department of gynecology and obstetrics in 2009 averaged €195.81 [9]. This sum includes remuneration for several outpatient contacts with the hospital and for initial treatments and follow-up treatment. Each patient was asked about the number of in-hospital stays, the length of each hospitalization, and about surgical procedures carried out. For each patient, or for each principal diagnosis, or for each single medical service, points were calculated taking the length of the hospitalization period into account [10].
In publicly financed hospitals, what is known as a “meals contribution charge” has to be paid by patients themselves for the period of the hospital stay. This charge amounts to approximately €10–17 per day. An average payment of €13.50 per day was used for the present study [11].
With regard to refundable drug costs, proprietary names, dosage, dosage scheme and period of administration had to be stated. For research on drug prices, the Internet-based “Information Tool on the Refunding Code” provided by Austrian Social Insurance was used. A prescription fee of €5 per prescription was used in the study [12].
An average price for one in vitro fertilization (IVF) and one IVF including intracytoplasmic sperm injection (ICSI) was used to calculate costs for medically assisted reproduction. Including the average costs for drugs, this amounts to a total of €2,430.27 and consists of €1,701.18 financed by the IVF Fund and a self-contribution by the patient of €729.09 [10]. The prices for one intrauterine insemination (IUI) differ widely and depend on the number of ultrasound examinations and on the drugs used. Refunded costs from health insurance companies also vary depending on the company. For this reason, and due to a lack of publicly available information, the price for one IUI, carried out in a public institution, was estimated at €200.
To allow calculation of the costs of private health-care services, the patients affected were asked about out-of-pocket services used and about complementary treatments. Data on indirect costs and productivity losses were also calculated on the basis of questions about days off work due to endometriosis and due to fertility treatments, unemployment, and illness-related retirement.
The human capital approach was used to calculate indirect costs due to sick leave. Formulas were used to assess the average productivity loss, as recommended by the Hanover Consensus [13, 14]. Productivity per day, expressed in Euros, thus amounted to €113.39 in 2009. To avoid overestimation, the friction-cost approach was conducted to calculate productivity loss in consequence of unemployment and illness-related retirement [13].
Statistics
The completed questionnaires were analyzed using Excel (2007 version) and IBM SPSS Statistics 19. To check the robustness of the analysis, a sensitivity analysis was also carried out in which the individual cost categories were adjusted in accordance with their (95 %) confidence intervals so that effects on total costs could then be analyzed.
Results
The characteristics of the participants are shown in Table 1. The 73 respondents consulted gynecology specialists in private practice 401 times during the 12 months, family physicians 245 times, and other specialists 138 times. On average, the respondents visited a physician 5.6 times per year, visiting family physicians 3.4 times and another specialist 1.9 times on average. The participants visited a hospital outpatient department a total of 151 times, an average of 2.1 times. The total costs of outpatient care for the 73 respondents amounted to €23,875 during the 1-year survey period. Annual costs for outpatient hospital consultation are €112.66. The total costs for outpatient care per case and year were calculated at €327.05.
The 73 respondents were admitted to hospital a total of 90 times during the 12 months. Nineteen of these hospital stays were due to diagnosis and conservative treatment of endometriosis, 55 for laparoscopy, and five were for laparotomy; 11 laparoscopies were carried out on a day-patient basis. The average hospitalization period was 6 days. For the 1-year survey period, including the privately paid meals contribution charge, in-patient care for the 73 respondents cost €246,594.90. In-patient care per case and year cost a total of €3,466.60 (Table 2).
With regard to medication, 63 of the 73 respondents took reimbursable drugs. To treat the endometriosis, 85 % of the affected women used analgesics, 30 % took progestins, 8 % took psychopharmaceuticals, and 7 % took gonadotropin-releasing hormone (GnRH) analogs. Table 3 shows the average costs of medications per case and year. The total costs for drugs amounted to €116.90, including prescription charges, per case and year. The 73 participants together used reimbursable drugs to the value of a total of €8,533.84 during the 1-year survey period.
Twenty-two of the women surveyed (30 %) experienced fertility problems due to their endometriosis during the survey period. Of these 22, 12 actually underwent medically assisted reproduction treatment during the survey period. Two respondents were treated with IUI and 10 with IVF, with one woman undergoing four IVF procedures, two receiving three IVFs, three receiving two IVFs, and four having one IVF during the observation period. The 12 women who underwent assisted reproduction treatment for infertility in connection with endometriosis used services with a total value of €49,005.40. Assisted reproduction due to infertility resulting from endometriosis thus cost €671.31 per case and year.
Sixty-nine respondents (95 %) used out-of-pocket services due to endometriosis-related symptoms during the 12-month period. Approximately half of those surveyed paid for analgesics and hormonal contraception themselves. Figure 1 shows the frequencies of the out-of-pocket services used. Table 4 shows the mean costs of out-of-pocket services per case and year and frequency of use. The total costs paid by the 73 respondents for out-of-pocket services during the 1-year survey period amounted to €65,231.46 excluding reimbursements totalling €9,498.00.
The annual out-of-pocket payments per patient were, therefore, calculated as €893.58. The average amounts reimbursed by social insurance amounted to €130.12. Figure 2 thus shows the direct costs arising for society as a whole per case and year. In all, treatment of one case of endometriosis currently costs €5,605.55 per year. Private expenditure covers 22 % of direct costs and public expenditure represents 78 % of them. Figure 3 shows the annual private and public expenditure per case of endometriosis.
Approximately 66 % (n = 48) of the women included in the study missed work for at least 1 day during the survey period. Altogether, the 73 respondents recorded a total of 1,148 working days lost per year, including 107 days off work due to treatments for medically assisted reproduction. On average, each patient was unable to work for approximately 16 days during the survey period. This implies an average productivity loss due to sick days per case and year of €1,702.47 (±2,610.97 SD).
In relation to unemployment, approximately 14 % of the affected women (n = 10) were unemployed for a total of 412 weeks due to endometriosis. Productivity losses due to unemployment amount to an average of €403.87 (±1,020.72 SD) per case and year. In total, sick days and unemployment for these 58 women resulted in a productivity loss of €153,762.59, with the average annual indirect costs per case amounting to €2,106.34 (±2,822.98 SD). This productivity loss is illustrated in Figure 4.
The average costs per case and year amount to €7,712 and consist of both direct and indirect costs. With a prevalence of 5 %, it can be inferred that 85,172 women in Austria are affected by endometriosis. Assuming that at least 50 % of these women—42,586 patients—require treatment for their symptoms, an overall economic burden of €328 million per year results (Table 5). In summary, it can be stated that the direct costs of endometriosis amount to €238.74 million (73 % of the total) and that productivity losses due to endometriosis (indirect costs) amount to €89.69 million (27 % of the total) per year.
Discussion
The medium size of the sample leads to sometimes relatively wide confidence intervals. Despite this, changes in outpatient costs and costs for reimbursable drugs have only a very slight effect on the total costs—i.e., these figures remain robust. Variations in costs for out-of-pocket services and for assisted reproduction influence the overall costs to the extent that they would increase or reduce them by approximately 3–5 %. This result can be regarded as acceptable. The largest cost categories—in-patient care and productivity losses—alter the overall costs to a relatively large extent (by around 11 % and 8 %, respectively). This means that the overall costs are sensitive to changes in these parameters and do not remain robust.
The direct economic costs of endometriosis in Austria were calculated in this study as approximately €239 million for 2009, or €5,606 per patient. For 2009, this figure represents approximately 0.8 % of all health-care expenditure in Austria and around 0.1 % of gross domestic product in Austria [3]. The indirect costs or productivity losses were evaluated at around €90 million or €2,106 per case. The total economic burden thus represents €328.42 million per year.
There have only been few studies conducted in Austria, from the field of neurology, that is directly comparable. Among these, one evaluation of the direct and indirect costs of Parkinson’s disease, based on a questionnaire (n = 81 patients), calculated that the disease represents an overall economic burden of €320 million per year [15]. When the different prevalences and resulting costs are taken into account, the two diseases are quite comparable with each other in economic terms.
At 9 %, assisted reproduction is not a major contributing factor to the high costs. Instead, in-patient care was identified as the major cost-driving factor, representing 45 % of total costs. Lost productivity is in second place as a cost factor at 27 %.
The smallest cost category is the use of reimbursable drugs, at 2 %. This appears to be compensated for by private consumption of over-the-counter products such as analgesics and hormonal contraceptives, since out-of-pocket payments represent a major cost item at 13 %. With regard to costs for outpatient care, representing a proportion of 4 %, it can be assumed that some underestimation of costs took place here, since according to the Austrian Endometriosis Association (Endometriose Vereinigung Austria, EVA) patients are increasingly consulting physicians who are not under contract with the statutory health insurance companies—although this was also reflected in the out-of-pocket cost category.
Despite this, as in any analysis of disease costs, there is a risk of systematic error, leading to overestimation or underestimation of the costs. The study population consisted of women affected by endometriosis, most of whom were members of the self-help organization EVA. It can, therefore, be assumed that the respondents had sought help from EVA due to severely burdensome disease courses. This may represent a selection bias and holds a risk of overestimation of costs, since it was mainly patients with a high level of suffering who took part in the survey. It may also explain the large number of hospital stays and laparoscopies. In the study by Brandes et al. [4], 41 % of the patients contacted had undergone surgery during the previous 12 months. The present study also included hospital stays due to a diagnosis of endometriosis, but without surgery (Table 2).
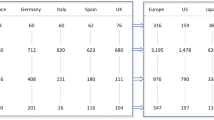
Comparison of the individual disease cost analyses is very difficult due to remarkable differences in health-care systems and charging structures. Table 6 shows a comparison with similar studies. The studies compared do not collect cost category data in a standard fashion. In general, most of the studies in the past have focused on direct costs, or specifically costs due to in-patient and surgical care [7]. As in the present study, in-patient costs in the comparative studies proved to be a major cost-driving factor. The costs of in-patient care were higher in comparison with the recent study published in 2012 by Simoens et al. [17], which may be due to the selection bias discussed above. By contrast, the productivity losses calculated by Simoens et al. are more than three times higher than in the present study. The reason for this may lie in the following methodological difference: as mentioned earlier, a friction-cost approach was used, on the one hand, while on the other figures for sick days were only included starting from 11 days, since shorter periods of only a few days can be compensated for by colleagues in the workplace or by extra work done on returning to the workplace [13, 14]. In addition, it is not clear from the study by Simoens et al. whether fertility treatments were included in the calculation. In addition, out-of-pocket payments were not taken into account. The degree of detail provided in the present study is certainly an advantage, even though the group studied was smaller.
Conclusions
This study impressively demonstrates the financial burden on the economy and on each individual patient caused by the disease of endometriosis. The massive consumption of resources represents a high level of usage of the medical services offered. The question arises of whether more timely diagnosis, followed by better and more targeted therapy, might have the potential to reduce these costs. However, there is probably a large potential for reducing indirect costs through timely diagnosis and appropriate treatment, since reducing the stress caused by the disease will also reduce productivity losses. However, further studies are needed to investigate this assumption.
Abbreviations
- EVA:
-
Endometriose Vereinigung Austria (Austrian Endometriosis Association)
- GnRH:
-
Gonadotropin-releasing hormone
- ICD:
-
International Classification of Diseases
- ICSI:
-
Intracytoplasmic sperm injection
- IUI:
-
Intrauterine insemination
- IVF:
-
In vitro fertilization
References
Björnberg A, Garrofé BC, Lindblad S. Euro Health Consumer Index 2009 (2009) Danderyd, Sweden: Health Consumer Powerhouse. Available online at: http://www.healthpowerhouse.com/files/Report%20EHCI%202009%20091005%20final%20with%20cover.pdf. Accessed 14 Dec 2012
Endometriose Schweppe K (2003) Eine Erkrankung ohne Lobby. Zentralbl Gynäkol. 125:233
Statistik Austria. Available online at: http://www.statistik.at. Accessed 12 Aug 2011)
Brandes I, Kleine-Budde K, Mittendorf T (2009) Krankheitskosten bei Endometriose. Geburtshilfe Frauenheilkd 69:925–930
European Institute of Women’s Health. Women’s health In Europe: facts and figures across the European Union. Available online at: http://www.eurohealth.ie/pdf/WomenshealthinEurope_FINALpdf. Accessed 8 Sept 2011)
Hudelist G, Fritzer N, Thomas A, Niehues C, Oppelt P, Haas D et al (2012) Diagnostic delay for endometriosis in Austria and Germany: causes and possible consequences. Hum Reprod 27:3412–3416
Gao X, Outley J, Botteman M, Spalding J, Simon J, Pashos C (2006) Economic burden of endometriosis. Fertil Steril 86:1561–1572
Simoens S, Hummelshoj L, D’Hooghe T (2007) Endometriosis: cost estimates and methodological perspective. Hum Reprod Update 14:395–404
Ruschitzka A, Scheuringer M. DIAG-Extranet database. Available online at: http://www.hauptverband.at. Accessed 3 Aug 2011
Bundesministerium für Gesundheit. Available online at: http://www.bmg.gv.at. Accessed 24 Jun 2011
Öffentliches Gesundheitsportal Österreich. Gesundheitsleistungen—Was kostet der Spitalsaufenthalt? Available online at: https://www.gesundheit.gv.at. Accessed 14 Jun 2011
Hauptverband der österreichischen Sozialversicherungsträger. Available online at: http://www.sozialversicherung.at. Accessed 3 August 2011
Greiner W (2008) Die Berechnung von Kosten und Nutzen. In: Schöffski O, Graf von der Schulenburg JM (eds). Gesundheitsökonomische Evaluationen. Springer, Berlin, pp 49–63
Graf von der Schulenburg JM, Greiner W, Jost R, Klusen N, Kubin M, Leidl R et al (2007) Deutsche Empfehlung zur gesundheitsökonomischen Evaluation: Dritte und aktualisierte Fassung des Hannoveraner Konsens. Gesundh Ökon Qual Manag. 12:285–290
Campenhausen S, Winter Y, Gasser J, Seppi K, Reese J, Pfeiffer K et al (2009) Krankheitskosten und Versorgungssituation bei Morbus Parkinson—eine Analyse in Österreich. Wien Klin Wochenschr 121:574–582 [Article in German]
Levy AR, Osenenko KM, Lozano-Ortega G, Sambrook R, Jeddi M, Bélisle S et al (2011) Economic burden of surgically confirmed endometriosis in Canada. J Obstet Gynaecol Can 33:830–837
Simoens S, Dunselman G, Dirksen C, Hummelshoj L, Bokor A, Brandes I et al (2012) The burden of endometriosis: costs and quality of life of women with endometriosis and treated in referral centres. Hum Reprod 27:1292–1299
Acknowledgments
The authors are grateful to Ms Steinberger, MA, and Ms Hofmeister of the managing committee of the Austrian Endometriosis Association (Endometriose Vereinigung Austria, EVA) for their assistance. Furthermore, the authors would like to thank the following institutions for providing support: General Hospital Linz, Endometriosis competence center; University of Innsbruck, Department for Endocrinology and Reproductive Medizin; LKH Villach, Endometriosis competence center; Wilheminenspital Vienna, Department for Gynecology and Obstetrics and University of Salzburg, Department for Gynecology and Obstetrics. No financial support was provided to this article
Conflict of interest
The authors hereby state that there were no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Prast, J., Oppelt, P., Shamiyeh, A. et al. Costs of endometriosis in Austria: a survey of direct and indirect costs. Arch Gynecol Obstet 288, 569–576 (2013). https://doi.org/10.1007/s00404-013-2793-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-013-2793-0