Abstract
Background
Identifying biomarkers that can predict the prognosis and treatment response is helpful for individualizing breast cancer (BC) therapy. A neoadjuvant treatment setting is ideal for testing biomarkers capable of predicting the treatment response. This study analyzed the value of immunohistochemical biomarkers for predicting pathological complete response (pCR) and prognosis in a group of BC patients receiving standardized treatment.
Patients and methods
A total of 100 BC patients were treated with neoadjuvant chemotherapy (four cycles of epirubicin and cyclophosphamide) between 2000 and 2005. Formalin-fixed and paraffin-embedded core biopsies were taken before chemotherapy for immunohistochemical staining of ER, PgR, HER2, Bcl-2, p53, cyclin D1, CK5/6, CK8, CK18, and TOP2A. Patient and tumor characteristics and biomarker scores were used to predict pCR and prognosis, using logistic regression and Cox proportional hazard models.
Results
pCR was achieved in 11 patients and was predicted by the established marker Ki-67. In addition, CK5/6 and CK18 improved the prediction model and were associated with lower pCR rates. For the prognosis, only the established markers nodal status, Ki-67, and PgR predicted overall survival and nodal status; Ki-67 and PgR predicted distant disease-free survival.
Conclusions
In this small retrospective study, CK5/6 and CK18 appeared to improve prediction of pCR in addition to the established markers. CK5/6 may indicate a tumor type resembling a basal phenotype that is more resistant to anthracycline-based therapy, and CK18 may indicate a luminal subtype that is more resistant to chemotherapy. However, these results need to be replicated in larger studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attempts have been made during the last 10 years to incorporate predictive factors for both the treatment response and the prognosis into the decision-making processes involved in the treatment of breast cancer (BC) patients [1]. Some biomarkers related to molecular subtypes of BC have already been included in clinical trials [2] and are likely to be incorporated into clinical practice soon [3]. Research studies on neoadjuvant therapy are an ideal setting not only for assessing the response to specific forms of treatment, but also for correlating the treatment response with the initially assessed prognosis.
Several recent studies have confirmed that the pathological complete response (pCR) after neoadjuvant chemotherapy is an outstanding predictive factor for the prognosis. However, these findings have mainly involved HER2-positive and triple-negative subgroups of patients [4–7]. In patients with hormone receptor–positive BC, pCRs appear to be too infrequent for this type of effect to be seen, due to the sample sizes in the published studies. Some biomarkers have already been quite consistently associated with a pCR after neoadjuvant chemotherapy; these include the estrogen receptor (ER), progesterone receptor (PgR), grading (G), and proliferation as assessed by Ki-67 [8].
Additional molecular markers for the prognosis have mainly been described in adjuvant therapy studies or in cohort studies without treatment. These studies have led to the development of what are known as multigene marker tests, in which hundreds or thousands of markers have been tested, some 20–80 of which have been validated as predictive for the prognosis [9–11].
The GeparTrio study recently reported on the benefits of a preplanned treatment change to an alternative chemotherapy regimen in patients who do not respond to neoadjuvant chemotherapy. The pCR rates did not differ between the groups of patients who received response-guided treatment and those who did not. However, particularly in the groups of patients with hormone receptor positive carcinomas, the treatment change in nonresponders improved the prognosis for these patients independently of pCR [12]. These results imply that tumors may behave differently in relation to the treatment response and prognosis.
The aim of the present study was therefore to investigate the value of six BC biomarkers previously described in the literature in relation to the treatment response and prognosis, in addition to established biomarkers and well-known predictive and prognostic factors, in a cohort of patients who were treated in standardized fashion with neoadjuvant anthracycline-based chemotherapy.
Materials and methods
Patients
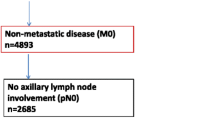
The study population consisted of 100 patients with histologically confirmed invasive BC who were treated with a neoadjuvant chemotherapy regimen consisting of four cycles of epirubicin (90 mg/m2 body surface area) and cyclophosphamide (600 mg/m2 BSA) between January 2000 and December 2005 at the University Breast Center of Franconia (Bavaria, Germany). No other adjuvant chemotherapy was allowed in patients included in the study. No patient received neoadjuvant or adjuvant trastuzumab. Patients were eligible for neoadjuvant chemotherapy if they had a tumor that was at least 1.5 cm in size as assessed on ultrasound or mammography prior to neoadjuvant chemotherapy. A total of 225 patients were treated with neoadjuvant chemotherapy between 2000 and 2005. Ninety-five patients were excluded because they did not receive the standardized neoadjuvant chemotherapy regimen described above. Two patients had to be excluded because they did not complete the chemotherapy regimen before surgery, and 13 patients were excluded because they had metastases at the time of the initial diagnosis. Adequate core biopsy material was not available for immunohistochemistry in 15 patients. The study was approved by the institutional ethics committee of the Medical Faculty of the University of Erlangen–Nuremberg. Informed consent was obtained from each patient before inclusion in the study.
Clinical data
The University Breast Center of Franconia has received certification from the German Cancer Society (Deutsche Krebsgesellschaft) and the German Society for the Study of Breast Diseases (Deutsche Gesellschaft für Senologie). To obtain certification, a breast center has to document each case of BC, including patient and tumor characteristics, treatment data, and some epidemiological data (details are available at http://www.onkozert.de). Follow-up information regarding local recurrences, distant metastases, and death has to be provided for up to 10 years. All histopathological data also have to be documented from the original pathological reports, including tumor size, axillary lymph-node status, grading, and estrogen receptor, progesterone receptor, and HER2/neu status. As part of the continuous certification process and quality assurance measures, breast centers and the quality of their data are audited annually. Data obtained through these processes were used in the analysis presented here.
Immunohistochemistry
Immunohistochemical analyses of whole-section slides of the core biopsies were carried out before the neoadjuvant chemotherapy, using the following primary antibodies in accordance with the manufacturers’ instructions: estrogen receptor (1:200, monoclonal mouse IgG, clone 1D5; Dako, Denmark), progesterone receptor (1:200 monoclonal mouse IgG, clone PgR 636; Dako, Denmark), HER2/neu (1:200, polyclonal rabbit IgG, clone cerB-2; Dako, Denmark), Ki-67 (1:100, monoclonal mouse IgG, clone MIB-1; Dako, Denmark), cytokeratin 5/6 (1:50, CK5/6, monoclonal mouse IgG, clone D5/16B4; Zytomed, Germany), cytokeratin 8 (1:200, CK8, monoclonal mouse IgG, clone C51; BioGenex, USA), cytokeratin 18 (1:500, CK18, monoclonal mouse IgG, clone CY-90; Sigma, USA), Bcl-2 (1:100, monoclonal mouse IgG, clone 124; Dako, Denmark), cyclin D1 (1:200, monoclonal rabbit IgG, clone SP4; DCS, Germany), P53 (1:50, monoclonal mouse IgG, clone DO-7; Dako, Denmark), and topoisomerase IIα (TOP2A, monoclonal mouse IgG, clone 3D4; Abcam, UK).
Secondary antibodies were selected relative to the primary antibodies; biotinylated rabbit antimouse IgG (Dako) and biotinylated goat antirabbit IgG (Dako) were used. Staining of Bcl-2, p53, CK5/6, CK8, and CK18 was visualized using strep-AB complex. The horseradish peroxidase (HRP) method was used for ER, PgR, HER2/neu, and MIB-1. A biotin–tyramine enhancement solution was used for staining of cyclin D1 and topoisomerase IIα.
All of the slides were evaluated independently by two observers. If there was disagreement regarding the interpretation of the immunohistochemical staining results, slides were examined with a two-headed microscope until consent was reached. The Remmele–Stegner immunoreactive score (IRS) was used [13]. HER2 status was scored in the pathology reports as 0, 1+, 2+, or 3+ in accordance with the guidelines published by Sauter et al. [14]. Tumors with a score of 0 or 1+ were regarded as HER2-negative, and those with a score of 3+ were regarded as HER2-positive. Tumors with a score of 2+ were tested for gene copy numbers of HER2 using chromogene in situ hybridization. Using a kit with two probes of different colors (ZytoDot, 2C SPEC HER2/CEN17; Zyto Vision Ltd., Bremerhaven, Germany), the gene copy numbers of HER2 and centromeres from the corresponding chromosome 17 were retrieved. A HER2/CEN17 ratio of ≥2.2 was regarded as amplification of HER2. Scoring was carried out in a standardized way by a group of dedicated pathologists in routine surgical pathology.
The pCR assessment was based on histopathological reports, all from one institution. Patients with a ypT0 ypN0 assessment were considered to have achieved a pCR. No invasive or noninvasive residual tumor tissue in the breast or nodes was allowed, as in the assessment by Sinn et al. [15].
Statistical considerations
Continuous data are presented as means with standard deviation, and categorical data as frequencies and percentages. As the biomarker values did not have a normal distribution, median values and interquartile ranges are shown. Spearman correlation coefficients between biomarkers were calculated.
The prediction of pCR was studied with logistic regression analyses. Simple logistic regression models were used for patient and tumor characteristics (age at diagnosis, tumor size before chemotherapy, histological type, and grading), for established biomarkers (Ki-67, ER, and PgR), and for investigational biomarkers (HER2 status, CK5/6, CK8, CK18, Bcl-2, p53). Odds ratios (OR) with 95 % confidence intervals are shown.
The predictive value of the investigational biomarkers, in addition to patient and tumor characteristics and the established biomarkers, was studied as follows. Initially, a multifactorial logistic regression model with the patient and tumor characteristics and established biomarkers was fitted. Backward stepwise variable selection was then carried out to obtain the best model in accordance with the Akaike information criterion (the final model without the investigational biomarkers). Next, another logistic regression model was fitted, containing the investigational biomarkers and the predictors from the final model without the investigational biomarkers. The variable selection procedure from above was carried out again, but on the condition that the selected predictors from the final model without the investigational biomarkers were retained. The resulting model (the final model with the investigational biomarkers) was compared with the final model without the investigational biomarkers using the likelihood ratio test. A significant test result means that the investigational biomarkers have predictive value independently of the established predictors. ORs with 95 % confidence intervals for the final model with the investigational biomarkers are shown. The predictive ability of the modeling procedure was estimated using the area under the curve (AUC) of the receiver operating characteristic, which was cross-validated twofold with 20 repetitions.
Overall survival and distant disease-free survival were studied using Cox proportional hazards (PH) models. Simple Cox PH models were used for the patient and tumor characteristics (age at diagnosis, tumor size before chemotherapy, histological type, grading, and nodal status), for the established biomarkers for prognosis (Ki-67, ER, PgR and HER2 status), and for the investigational biomarkers for prognosis (CK5/6, CK8, CK18, Bcl-2, and p53). Hazard ratios (HR) with 95 % confidence intervals are shown. The prognostic value of the investigational biomarkers, in addition to the patient and tumor characteristics and the established biomarkers, was studied in the same way as the logistic regression procedures described above. The proportional hazards assumptions in the final models were checked using tests correlating scaled Schoenfeld residuals with a suitable time transformation [16]. If the proportional hazards assumptions were not fulfilled, the analysis was to be repeated separately for survival times up to 5 years and from 5 years on.
All of the tests were two-sided, and P < 0.05 was regarded as statistically significant. Calculations were carried out using the R system for statistical computing (version 2.13.1; R Development Core Team, Vienna, Austria, 2011).
Results
A total of 100 patients were included in the analysis, 11 of whom had a pCR. The patients’ mean age was 53.6 years (±11.9 years). Patient characteristics and biomarker results are shown in Table 1.
Expression of each of the biomarkers was correlated with the others. Estrogen-receptor expression and progesterone-receptor expression clearly correlated with almost every biomarker except TOP2A and CK5/6. Cytokeratin 5/6 did not correlate with any of the other biomarkers, and CK8 and CK18 strongly correlated with each other. All correlations are presented in Table 2.
To assess the predictive value relative to pCR, simple logistic regression analyses were initially performed. Some of the investigational biomarkers were inversely associated with pCR, such as Bcl-2 expression (OR 0.72; 95 % CI, 0.52–0.99), CK8 (OR 0.70; 95 % CI, 0.56–0.87), and CK18 (OR 0.75; 95 % CI, 0.62–0.91). Ki-67, ER, PgR, and grading showed the expected associations (Table 3).
The preliminary multifactorial logistic regression analysis, which did not take the investigational biomarkers into account, identified grading and Ki-67 as relevant predictors. The other predictors were dropped during the variable selection process—i.e., their predictive value appeared to be irrelevant, or they were already explained by grading and Ki-67.
The ultimate logistic regression analyses, taking into account the relevant predictors from the preliminary analysis and in addition the investigational biomarkers, showed that the prediction can be improved overall by including CK5/6 and CK18 (P = 0.01, likelihood ratio test). ORs for the final model are shown in Table 4. Higher levels of CK5/6 or CK18 were associated with a decreased pCR rate. The cross-validated AUC was 0.67.
With regard to overall survival (OS), simple Cox regression analyses showed that negative nodal status and PgR expression were significantly associated with an improved OS. In addition, a high level of p53 expression (HR 1.16; 95 % CI, 1.02–1.32) and lower TOP2A expression (HR 0.76; 95 % CI, 0.58–0.99) were also associated with OS (Table 5).
The preliminary multifactorial Cox regression analysis, which did not take the investigational biomarkers into account, identified age, pN, Ki-67, and PgR as relevant prognostic factors. The ultimate Cox regression analyses, taking into account the relevant prognostic factors from the preliminary analysis and in addition the investigational biomarkers, did not yield any additional relevant prognostic factors—i.e., all investigational biomarkers were dropped during the variable selection process (data not shown). The HRs of the final Cox model are shown in Table 6.
With regard to distant disease-free survival (DDFS), only nodal status was found to be a significant prognostic factor in the simple Cox regression analyses (Table 6). In the multivariate model with established prognostic factors, nodal status, Ki-67 expression, and PgR expression were selected as relevant prognostic factors. None of the investigational immunohistochemical markers helped to improve the prognosis significantly (data not shown).
Discussion
In this retrospective study of 100 BC patients who were treated in a standardized fashion with four cycles of epirubicin and cyclophosphamide, grading and Ki-67 expression were found to be the strongest among the established predictors of a pCR. The investigational biomarkers CK5/6 and CK18 appeared to have an additional predictive value for pCR. Other markers such as Bcl-2 and hormone receptor expression did not remain significant predictors in the multivariate model.
Although the study has a small sample size and only a limited number of events relative to the outcome parameter pCR, with 11 patients, most of the correlations with biomarkers and pCR identified are in accordance with the published literature findings. Patients with higher proliferation, assessed either by grading or Ki-67, were associated with a higher pCR rate. This is consistent with several published studies [8]. The proliferation marker topoisomerase IIα, discussed as a target of epirubicin [17], was associated with a higher response rate (OR 1.39; 95 % CI, 0.86–2.25), although not with statistical significance. Hormone receptor expression also correlated with a decreased pCR.
Luminal cytokeratin markers 8 and 18 were inversely correlated with pCR in the univariate analysis, probably reflecting their positive correlation with expression of hormone receptors and negative correlation with proliferation markers. In addition, CK18 and CK5/6 helped improve pCR prediction in the multivariate model. Interestingly, this correlation was inverse. The greater the expression of the basal marker CK5/6 was, the less likely it was for a pCR to occur. This is consistent with the findings of other studies such as the one by Li et al., in which CK5/6-positive patients had a pCR rate of 22.2 % and CK5/6-negative patients had a pCR rate of 47.8 % [18]. Since triple-negative BCs generally have a higher pCR rate, CK5/6 positivity might reflect a more basal-like subtype that is resistant to chemotherapy. In the present small study, CK5/6 did not have any relevance for predicting the prognosis either for OS or DDFS.
The progesterone receptor (PgR) is one example of the way in which the response and prognosis may be interpreted in relation to one biomarker in this type of study. A high level of PgR expression indicates a reduced pCR and a better prognosis. The effects of the PgR on the prognosis may therefore be less likely to be mediated by a response to the chemotherapy. CK18 does not appear to have a very strong effect on the prognosis; it was not helpful in predicting OS or DDFS. However, it did appear to be associated with pCR. If its absence of effect relative to predicting the prognosis is a genuinely negative finding, then it could be hypothesized that there must be additional prognostic effects of CK18 on the prognosis that are independent of the chemotherapy response.
The predictiveness of biomarkers relative to pCR and relative to the survival prognosis was analyzed separately. Ideally, in order to investigate the relationship between biomarkers, the treatment response as assessed by pCR, and the prognosis, a Cox regression analysis including all the biomarkers of interest and pCR, as well as the interactions between the biomarkers and pCR as prognostic factors, would combine the separate analyses in the present study. Using a Cox model of this type, it would be possible to evaluate in a differentiated fashion the way in which biomarkers influence survival independently of pCR. For each of the four combinations of PgR high/low with pCR yes/no, for example, survival rates could be calculated and HRs based on these combinations could be estimated and compared. The greatest problem in carrying out this type of analysis is the sample size; as pCR occurs only relatively rarely, large numbers of patients who reach the survival event are needed.
It should be pointed out that the conclusions drawn here need to be regarded with caution, as one obvious weakness of the present study is the small sample size, with only 100 patients and 11 patients with a pCR. Therfore for example analyses in subsets of patients such as luminal A like, luminal B like HER2 positive or triple negatives were not feasible. However, the small sample size was the result of rigorously excluding patients who received any form of treatment other than the one specified, in order to restrict interpretation of the results to the chemotherapy regimen with anthracycline and cyclophosphamide. This as well restricts the conclusions to patients that did not receive trastuzumab, and it has to be kept in mind, that HER2 positive patients did not receive trastuzumab, neither in the neoadjuvant nor in the adjuvant setting, as the drug was not approved yet at the time, when the patients were treated. Some markers appeared to be significant signals for predicting both pCR and prognosis, so that a causal connection may be hypothesized. In recent years, the use of taxanes as a standard treatment has been included in most neoadjuvant study protocols [7, 19–22]. Furthermore targeted therapies such as lapatinib, trastuzumab, bevacizumab, pertuzumab, everolimus and others are tested especially when a resistance against a standard chemothereapy is observed or anticipated [6, 23–25]. Therefore, this might be another limitation for interpreting the results with regard to the clinics.
In conclusion, this study provides evidence that the basal marker CK5/6 and the luminal marker CK18 may be potentially helpful in predicting the response to chemotherapy regimens containing anthracycline and cyclophosphamide. In this small retrospective study, it is not possible to assess whether these effects may translate into prognostic factors. Further studies are needed in order to differentiate biomarkers with regard to their ability to predict the treatment response and prognosis.
References
Liedtke C, Wolf MK, Kiesel L (2010) New concepts for targeted systemic therapy in breast cancer. Geburtsh Frauenheilk 70(8):625–633. doi:10.1055/s-0030-1250182
Harbeck N, Salem M, Nitz U, Gluz O, Liedtke C (2010) Personalized treatment of early-stage breast cancer: present concepts and future directions. Cancer Treat Rev 36(8):584–594. doi:10.1016/j.ctrv.2010.04.007
Fasching PA, Fehm T, Janni W, Kummel S, Luftner D, Lux MP, Maass N (2010) Breast cancer therapy—a state of the art review. Geburtsh Frauenheilk 70(11):875–886. doi:10.1055/s-0030-1250437
Andre F, Mazouni C, Liedtke C, Kau SW, Frye D, Green M, Gonzalez-Angulo AM, Symmans WF, Hortobagyi GN, Pusztai L (2008) HER2 expression and efficacy of preoperative paclitaxel/FAC chemotherapy in breast cancer. Breast Cancer Res Treat 108(2):183–190. doi:10.1007/s10549-007-9594-8
Liedtke C, Mazouni C, Hess KR, Andre F, Tordai A, Mejia JA, Symmans WF, Gonzalez-Angulo AM, Hennessy B, Green M, Cristofanilli M, Hortobagyi GN, Pusztai L (2008) Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol 26(8):1275–1281. doi:10.1200/JCO.2007.14.4147
Untch M, Fasching PA, Konecny GE, Hasmuller S, Lebeau A, Kreienberg R, Camara O, Muller V, du Bois A, Kuhn T, Stickeler E, Harbeck N, Hoss C, Kahlert S, Beck T, Fett W, Mehta KM, von Minckwitz G, Loibl S (2011) Pathologic complete response after neoadjuvant chemotherapy plus trastuzumab predicts favorable survival in human epidermal growth factor receptor 2-overexpressing breast cancer: results from the TECHNO trial of the AGO and GBG study groups. J Clin Oncol 29(25):3351–3357. doi:10.1200/JCO.2010.31.4930
Untch M, von Minckwitz G, Konecny GE, Conrad U, Fett W, Kurzeder C, Luck HJ, Stickeler E, Urbaczyk H, Liedtke B, Beckmann MW, Salat C, Harbeck N, Muller V, Schmidt M, Hasmuller S, Lenhard M, Nekljudova V, Lebeau A, Loibl S, Fasching PA (2011) PREPARE trial: a randomized phase III trial comparing preoperative, dose-dense, dose-intensified chemotherapy with epirubicin, paclitaxel, and CMF versus a standard-dosed epirubicin–cyclophosphamide followed by paclitaxel with or without darbepoetin alfa in primary breast cancer–outcome on prognosis. Ann Oncol 22(9):1999–2006. doi:10.1093/annonc/mdq713
Fasching PA, Heusinger K, Haeberle L, Niklos M, Hein A, Bayer CM, Rauh C, Schulz-Wendtland R, Bani MR, Schrauder M, Kahmann L, Lux MP, Strehl JD, Hartmann A, Dimmler A, Beckmann MW, Wachter DL (2011) Ki67, chemotherapy response, and prognosis in breast cancer patients receiving neoadjuvant treatment. BMC Cancer 11:486. doi:10.1186/1471-2407-11-486
Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M, Baehner FL, Walker MG, Watson D, Park T, Hiller W, Fisher ER, Wickerham DL, Bryant J, Wolmark N (2004) A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med 351(27):2817–2826. doi:10.1056/NEJMoa041588
Parker JS, Mullins M, Cheang MC, Leung S, Voduc D, Vickery T, Davies S, Fauron C, He X, Hu Z, Quackenbush JF, Stijleman IJ, Palazzo J, Marron JS, Nobel AB, Mardis E, Nielsen TO, Ellis MJ, Perou CM, Bernard PS (2009) Supervised risk predictor of breast cancer based on intrinsic subtypes. J Clin Oncol 27(8):1160–1167. doi:10.1200/JCO.2008.18.1370
van’t Veer LJ, Bernards R (2008) Enabling personalized cancer medicine through analysis of gene-expression patterns. Nature 452(7187):564–570. doi:10.1038/nature06915
von Minckwitz G, Blohmer JU, Costa S, Denkert C, Eidtmann H, Eiermann W, Gerber B, Hanusch C, Hilfrich J, Huober J, Jackisch C, Kaufmann M, Kümmel S, Paepke S, Schneeweiss A, Untch M, Zahm DM, Mehta K, Loibl S (2011) Neoadjuvant chemotherapy adapted by interim response improves overall survival of primary breast cancer patients—results of the GeparTrio trial. Cancer Res 71(24 Suppl):103s
Remmele W, Stegner HE (1987) A proposal for the standardization of the immunoreactive score (Irs) for the immunohistochemical demonstration of estrogen-receptors (Er-Ica) in breast-cancer. Pathologe 8(3):138–140
Sauter G, Lee J, Bartlett JM, Slamon DJ, Press MF (2009) Guidelines for human epidermal growth factor receptor 2 testing: biologic and methodologic considerations. J Clin Oncol 27(8):1323–1333. doi:10.1200/JCO.2007.14.8197
Sinn HP, Schmid H, Junkermann H, Huober J, Leppien G, Kaufmann M, Bastert G, Otto HF (1994) Histological regression of breast cancer after primary (neoadjuvant) chemotherapy. Geburtsh Frauenheilk 54(10):552–558. doi:10.1055/s-2007-1022338
Grambsch PM, Therneau TM (1994) Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 81(3):515–526
Slamon D, Eiermann W, Robert N, Pienkowski T, Martin M, Press M, Mackey J, Glaspy J, Chan A, Pawlicki M, Pinter T, Valero V, Liu MC, Sauter G, von Minckwitz G, Visco F, Bee V, Buyse M, Bendahmane B, Tabah-Fisch I, Lindsay MA, Riva A, Crown J (2011) Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med 365(14):1273–1283. doi:10.1056/NEJMoa0910383
Li XR, Liu M, Zhang YJ, Wang JD, Zheng YQ, Li J, Ma B, Song X (2011) CK5/6, EGFR, Ki-67, cyclin D1, and nm23-H1 protein expressions as predictors of pathological complete response to neoadjuvant chemotherapy in triple-negative breast cancer patients. Med Oncol 28(Suppl 1):S129–S134. doi:10.1007/s12032-010-9742-6
von Minckwitz G, Rezai M, Loibl S, Fasching PA, Huober J, Tesch H, Bauerfeind I, Hilfrich J, Eidtmann H, Gerber B, Hanusch C, Kuhn T, du Bois A, Blohmer JU, Thomssen C, Dan Costa S, Jackisch C, Kaufmann M, Mehta K, Untch M (2010) Capecitabine in addition to anthracycline- and taxane-based neoadjuvant treatment in patients with primary breast cancer: phase III GeparQuattro study. J Clin Oncol 28(12):2015–2023. doi:10.1200/JCO.2009.23.8303
von Minckwitz G, Untch M, Blohmer JU, Costa SD, Eidtmann H, Fasching PA, Gerber B, Eiermann W, Hilfrich J, Huober J, Jackisch C, Kaufmann M, Konecny GE, Denkert C, Nekljudova V, Mehta K, Loibl S (2012) Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. doi:10.1200/JCO.2011.38.8595
von Minckwitz G, Untch M, Nuesch E, Loibl S, Kaufmann M, Kummel S, Fasching PA, Eiermann W, Blohmer JU, Costa SD, Mehta K, Hilfrich J, Jackisch C, Gerber B, du Bois A, Huober J, Hanusch C, Konecny G, Fett W, Stickeler E, Harbeck N, Muller V, Juni P (2011) Impact of treatment characteristics on response of different breast cancer phenotypes: pooled analysis of the German neo-adjuvant chemotherapy trials. Breast Cancer Res Treat 125(1):145–156. doi:10.1007/s10549-010-1228-x
Untch M, Fasching PA, Konecny GE, von Koch F, Conrad U, Fett W, Kurzeder C, Luck HJ, Stickeler E, Urbaczyk H, Liedtke B, Salat C, Harbeck N, Muller V, Schmidt M, Hasmuller S, Lenhard M, Schuster T, Nekljudova V, Lebeau A, Loibl S, von Minckwitz G (2011) PREPARE trial: a randomized phase III trial comparing preoperative, dose-dense, dose-intensified chemotherapy with epirubicin, paclitaxel and CMF versus a standard-dosed epirubicin/cyclophosphamide followed by paclitaxel ± darbepoetin alfa in primary breast cancer—results at the time of surgery. Ann Oncol 22(9):1988–1998. doi:10.1093/annonc/mdq709
von Minckwitz G, Eidtmann H, Rezai M, Fasching PA, Tesch H, Eggemann H, Schrader I, Kittel K, Hanusch C, Kreienberg R, Solbach C, Gerber B, Jackisch C, Kunz G, Blohmer JU, Huober J, Hauschild M, Fehm T, Muller BM, Denkert C, Loibl S, Nekljudova V, Untch M (2012) Neoadjuvant chemotherapy and bevacizumab for HER2-negative breast cancer. N Engl J Med 366(4):299–309. doi:10.1056/NEJMoa1111065
Untch M, Loibl S, Bischoff J, Eidtmann H, Kaufmann M, Blohmer JU, Hilfrich J, Strumberg D, Fasching PA, Kreienberg R, Tesch H, Hanusch C, Gerber B, Rezai M, Jackisch C, Huober J, Kuhn T, Nekljudova V, von Minckwitz G (2012) Lapatinib versus trastuzumab in combination with neoadjuvant anthracycline-taxane-based chemotherapy (GeparQuinto, GBG 44): a randomised phase 3 trial. Lancet Oncol 13(2):135–144. doi:10.1016/S1470-2045(11)70397-7
Untch M, Rezai M, Loibl S, Fasching PA, Huober J, Tesch H, Bauerfeind I, Hilfrich J, Eidtmann H, Gerber B, Hanusch C, Kuhn T, du Bois A, Blohmer JU, Thomssen C, Dan Costa S, Jackisch C, Kaufmann M, Mehta K, von Minckwitz G (2010) Neoadjuvant treatment with trastuzumab in HER2-positive breast cancer: results from the GeparQuattro study. J Clin Oncol 28(12):2024–2031. doi:10.1200/JCO.2009.23.8451
Conflict of interest
The authors hereby declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wachter, D.L., Fasching, P.A., Haeberle, L. et al. Prognostic molecular markers and neoadjuvant therapy response in anthracycline-treated breast cancer patients. Arch Gynecol Obstet 287, 337–344 (2013). https://doi.org/10.1007/s00404-012-2534-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-012-2534-9