Abstract
Purpose
To evaluate the clinical significance of intrapartum fetal heart rate (FHR) monitoring in low-risk pregnancies according to guidelines and specific patterns.
Methods
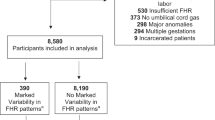
An obstetrician, blinded to neonatal outcome, retrospectively reviewed 198 low-risk cases that underwent continuous electronic fetal monitoring (EFM) during the last 2 h before delivery. The tracings were interpreted as normal, suspicious or pathological, according to specific guidelines of EFM and by grouping the different FHR patterns considering baseline, variability, presence of decelerations and bradycardia. The EFM groups and the different FHR-subgroups were associated with neonatal acid base status at birth, as well as the short-term neonatal composite outcome. Comparisons between groups were performed with Kruskal–Wallis test. Differences among categorical variables were evaluated using Fisher’s exact test. Significance was set at p < 0.05 level.
Results
Significant differences were found for mean pH values in the three EFM groups, with a significant trend from “normal” [pH 7.25, 95 % confidence interval (CI) 7.28–7.32] to “pathological” tracings (pH 7.20, 95 % CI 7.17–7.13). Also the rates of adverse composite neonatal outcome were statistically different between the two groups (p < 0.005). Among the different FHR patterns, tracings with atypical variable decelerations and severe bradycardia were more frequently associated with adverse neonatal composite outcome (11.1 and 26.7 %, respectively). However, statistically significant differences were only observed between the subgroups with normal tracings and bradycardia.
Conclusions
In low-risk pregnancies, there is a significant association between neonatal outcome and EFM classification. However, within abnormal tracings, neonatal outcome might differ according to specific FHR pattern.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neonatal metabolic acidosis occurs in 20–25 newborns per 1,000 deliveries. Most cases are inconsequential although 3–4 of the acidotic neonates will be diagnosed with multiorgan failure [1, 2].
Since the 1960s, continuous electronic fetal heart rate monitoring (EFM) has influenced the assessment and identification of fetal hypoxia in an attempt to prevent subsequent perinatal asphyxia and acidosis [3, 4].
Unfortunately, its widespread use in the ensuing decades did not attain these aims and, on the other hand, brought to a rise in the rate of unnecessary intervention.
Many clinicians focused their attention on the limitations of this technology concluding that the poor interobserver/intraobserver agreement in the classification and interpretation of EFM and the erroneous assessment of the fetal physiologic condition might account for the high false-positive rate of diagnosing fetal distress [5–8].
Despite these limitations, the EFM remains the gold standard method for fetal surveillance in labor and there is a common belief that a normal reactive, accelerative and not decelerative EFM pattern is suggestive of a reassuring fetal status. Similarly, the tracings characterized by absent variability with persistent late deceleration and/or prolonged decelerations represent an ominous sign, potentially associated with adverse perinatal outcome.
Between these two extremes, there is a variable spectrum of suspicious tracings that the clinicians have to deal with. These cases represent a great challenge, especially for those units where the intrapartum fetal blood sampling (FBS) or ST analysis are not routinely performed [7].
The aim of our study was to assess the clinical significance of intrapartum EFM interpretation system in low-risk pregnancies during the last 2 h of labor. To assess our objective, we first evaluated the association between short-term neonatal outcome measures and the classification of EFM tracings, as defined and adapted from the Documentation Centre on Perinatal and Reproductive Health (SaPeRiDoc) guidelines (EFM groups) [9]. Second, we focused our attention on specific fetal heart rate (FHR) patterns (FHR-subgroups) to determine whether different features of non-reassuring or abnormal tracings were associated with a different clinical neonatal outcome.
Methods
A 6-month retrospective review of labor ward database of Maternal and Child Institute Burlo Garofolo (third Italian referral center with roughly 2,000 deliveries/year) was carried out to assess all intrapartum EFM tracings in low-risk pregnancies. Institutional approval for this study was granted by Technical Scientific Committee.
We considered only EFM tracings of singleton, at term (gestational age was confirmed in all cases by crown rump length measurement in the first trimester), who entered in labor spontaneously. Only spontaneous and operative vaginal deliveries were included. For all of them, external continuous FHR monitoring during the last 2 h of labor and full documentation of short-term neonatal outcomes were available. Low-risk pregnancies were defined as cases without potential risk factors for the development of acidosis, cerebral palsy, perinatal death, and neonatal encephalopathy [9].
To avoid the potential influence on acid base status at birth and neonatal outcome measures, only cases with normal—as stated in the reference guideline—admission test and/or reassuring EFM tracings in the first stage of labor were considered in the final analysis. All tracings were reviewed by a trained obstetrician (G.M.), who was blinded to umbilical cord gases results and neonatal outcome. Another obstetrician (M.P.) randomly reviewed 40 FHR tracings without knowledge of the neonatal outcome. The inter-observer agreement was compared between the two investigators and showed good correlation with a κ score of 0.74 [10].
All cases had immediate cord clamping after delivery and only those with an interval between the time of delivery and the last available FHR recording <10 min were included. The cord was double clamped at a minimum length of 10 cm when the placenta was still in situ and both the artery and vein were sampled in preheparinised syringes and analyzed within 15 min.
As a first step, the investigator evaluated the selected tracings classifying the 2-h FHR patterns before delivery according to the FHR variables, as defined in the reference guideline (Table 1). Specifically, the EFM groups were considered as normal, if all four FHR variables fell into the reassuring category; suspicious, if one of the variables presented non-reassuring characteristics and the remainder variables were reassuring; pathological, if more than two non-reassuring or more than one abnormal variable was, respectively, observed [9].
Similarly to the studies of Williams and Galerneau [11, 12], EFM tracings were then classified into ten patterns (FHR-subgroups) according to the EFM features (Table 2). In the interpretation of tracings, early, variable or late decelerations were considered significant only if associated with more than 50 % of the uterine contractions and in the presence of a minimum number of three. Variable decelerations were considered as typical or atypical. Atypical deceleration was defined in the presence of at least one of the following additional components: loss of primary or secondary rise in baseline rate; slow return to baseline FHR after the end of the contraction; prolonged secondary rise in baseline rate; biphasic deceleration; loss of variability during deceleration; continuation of baseline rate at lower level [9, 11, 12].
Bradycardia was considered as moderate or severe if a persistent fall of baseline between 100 and 109 beats/min and below 100 beats/min was, respectively, observed over a time period of 5 or 10 min [9]. The presence or absence of acceleration in each subgroup was also evaluated.
In order to assess the clinical significance of normal/suspicious/pathological EFM groups and of the different FHR-subgroups, we considered their association with both umbilical artery’s (UA) pH and base deficit (BD) values at birth, as well as with the short-term composite outcome. Adverse composite neonatal outcome was defined as the presence of at least one of UA pH <7 at birth, APGAR score <7 at 5 min, neonatal resuscitation in delivery room and admission to Neonatal Intensive Care Unit for distress at birth.
We chose the UA pH value of 7.20 as the cut off to define neonatal acidemia, to consider also the initial endangerment of the fetal acid base status. Cases with UA pH less than 7.10 and 7.00 were also reported [13]. A value greater than −12 mmol/L of BD was considered as a sign of metabolic acidemia [14, 15].
Categorical variables were presented as absolute frequencies, percentages and 95 % confidence intervals (95 % CI); continuous variables were presented as mean and 95 % CIs. Comparisons between groups were performed with Kruskal–Wallis test (non-parametric analysis of variance) and with non-parametric test for trend across ordered groups developed by Cuzick. Differences among categorical variables were evaluated using Fisher’s exact test (two tailed). Post hoc pairwise comparison was made using Bonferroni correction. Statistical analysis was carried out with the STATA statistical package (version 9.0) and p < 0.05 was considered as statistically significant.
Results
A total of 198 patients were included in the study. Significant differences were found for mean pH and BD values in the three EFM groups, with a remarkable trend from “normal” (mean pH 7.25, 95 % CI 7.28–7.32; mean BD −3.35, 95 % CI −4.19 to −2.50) to “pathological” tracings (mean pH 7.20, 95 % CI 7.17–7.13; mean BD −7.50, 95 % CI −8.50 to −6.50; p < 0.001). Statistically significant differences were found between the normal group and both the suspicious and pathological ones for pH below 7.20 (p < 0.05) (Table 3). Significant differences in the rate of adverse neonatal outcome occurred only between the pathological and the normal EFM group (16.9 vs. 0 %, respectively, p < 0.05, Table 3). Among the FHR subgroups, the most represented subgroups were the 1, 3, 4, 9 and 10. No cases showed the FHR features described for patterns 2 and 6. The subgroups 5, 7 and 8 were excluded from the analysis because of the small sample size; 18 further cases were not considered because of the association of more than one FHR pattern (i.e. typical or atypical decelerations associated with moderate or severe bradycardia).
A difference of mean pH and BD values were found in the analyzed subgroups (173 cases), with a significant decreasing trend of pH from subgroup 1 to subgroup 10 (p < 0.001, Table 4).
Severe bradycardia (subgroup 10) was associated with the highest rate of pH <7.20 (46.7 %), pH <7.10 (26.7 %) and adverse neonatal outcomes (26.7 %). As for the type of variable decelerations, the presence of an atypical pattern was more frequently associated with a pH <7.20 (48.2 %) as compared with FHR patterns with typical decelerations (28.6 %). Among the tracings with variable deceleration, only one case presented a pH value <7 at birth.
The presence of accelerations changed significantly among the FHR subgroups, showing a decreasing rate of appearance from normal tracings to tracings characterized by typical and, even more, by atypical decelerations. In particular, the presence of acceleration was statistically different between subgroup 4 (atypical decelerations) and all the other subgroups. Accelerations occurred more frequently in the subgroups with bradycardia than in tracings presenting decelerations. The observation that all cases with severe bradycardia (mean pH 7.19, 95 % CI 7.13–7.26) were preceded by an accelerative tracing (Table 4) was of interest.
As regards the duration of the different suspicious/pathological patterns, we found a significant decreasing trend of duration (minutes) among the FHR subgroups (values ranging from 34.6, 95 % CI 30.0–39.2, to 9.7, 95 % CI 7.7–11.6; p < 0.001). Significant differences of time-interval between the onset of FHR pattern and delivery were found between tracings with typical or atypical decelerations and moderate or severe bradycardia (Table 4).
Discussion
The results we obtained in our study revealed the existence of a significant relationship between the three EFM-groups and the pH/BD values: decreasing mean values of pH and increasing mean values of BD were, respectively, observed, ranging from “normal” to “pathological” tracings. However, mean cord blood parameters remained always within the range of “normality”, showing that in our experience, the EFM classification has a low positive predictive value to identify at least one of the defined measures of adverse neonatal outcome (PPV 12 %). This is an expected result, which can theoretically be related to epidemiological and clinical aspects. It might be related to the low positive predictive value of the test that is dictated by its high sensitivity and low specificity (100 and 27.8 %, respectively, in our experience), in association with the low prevalence of the target condition.
It might also be the result of the so-called “treatment paradox effect”. This phenomenon is described in studies of prediction, where an outcome (i.e. neonatal outcome variables) with a known association with the test predictor (i.e. EFM)—conditional probability—can be ameliorated or avoided by an intervention.
As stated by different national EFM guidelines, suspicious or pathological FHR patterns need actions to further investigate the cause and then correct the cause or expedite delivery: we arbitrarily decided to consider the EFM interpretation guidelines commonly used in the Italian obstetric departments, where invasive ancillary tests, such as FBS, are not commonly used. In our experience, the lack of information about the use of conservative resuscitative measures, such as maternal repositioning or administration of intravenous fluid bolus, might represent a limitation in our observation. However, these aspects were beyond the objective of our study, since our aim was to assess whether a defined interpretation of different abnormal FHR patterns might have a different impact on neonatal outcome [7, 9, 16–18].
From our analysis we basically identified four categories of abnormal FHR patterns.
Subgroups 3 and 4: FHR patterns with variable decelerations associated with normal variability were the most frequent tracings observed in our study population (45.4 % of the cases). Gibb and Arulkumaran [19] described the FHR patterns of subacute hypoxia, characterized by the presence of repetitive variable decelerations. Schifrin [20] observed that every form of hypoxia is preceded by the presence of decelerations before any rising of baseline and reduction of variability. Our results support the hypothesis that subgroup 3 and 4 might represent two different forms of fetal “stress”, where the fetus starts to use its resources to cope with a suboptimal condition [21]. This hypothesis might be inferred by the following observations: (1) the frequency of accelerations is progressively reduced when typical and atypical variable decelerations occur (from 81.0 to 66.7 %, respectively); (2) the prevalence of cases with pH below 7.20 is different between the two groups (28.6 vs. 48.2 %) and significantly higher than in normal tracings; (3) there is a decreasing trend of pH from normal tracings to tracings with typical and atypical decelerations.
Subgroups 9 and 10: experimental studies on monkeys [22] showed that after total umbilical cord occlusion, to simulate marked bradycardia, brain blood flow ceased in 5–6 min, and cord’s pH dropped at a rate of 0.05 U/min. Other experimental studies supported this hypothesis: a significant decrease of pH at a rate of 0.03 per min has been observed in the case of a FHR baseline below 100 beats/min [19].
In line with these observations, the mean pH values observed in cases with severe bradycardia were significantly lower as compared with normal FHR patterns (mean 7.19, CI 95 % 7.13–7.26 vs. mean 7.31, CI 95 % 7.29–7.33, respectively) despite the short duration of this pattern and the presence of accelerations before the onset of severe bradycardia. These observations support the consensus of guidelines on managing these tracings: expedite delivery is mandatory [9, 16–18].
It is well known that besides the characteristics of FHR, the duration of the specific pattern can have a significant influence on pH at birth [21, 23]. In our experience, despite the limited sample size of the study group, the median time-intervals to delivery for moderate and marked bradycardia were significantly lower than the duration of FHR tracings with variable decelerations. It might reflect the different interpretation attributed to these patterns: bradycardia even if associated with normal variability was considered a sign of acute fetal “distress”, whilst tracings characterized by variable decelerations were considered a marker of subacute hypoxia only when persisting for a longer period.
The tracings with moderate bradycardia deserve particular considerations. It has been reported that this pattern might be the consequence of relative or absolute feto-pelvic disproportion [24]. No cases of adverse neonatal outcome were observed for this FHR subgroup and mean pH values were similar to those observed in tracings with decelerations. However, the time interval to delivery for moderate bradycardia was shorter and similar to that observed in cases of severe bradycardia. How to manage this condition was beyond the aim of our study, but evidence from our retrospective analysis supported the belief that obstetrician’s attitudes were to reduce the time interval to delivery, considering moderate bradycardia an ominous pattern, just like severe bradycardia. In this context, it is unclear whether these FHR tracings might represent a different form of fetal “stress”, leading, if long lasting, to “distress”.
In literature most efforts are directed to describe “extreme” FHR patterns of gradually developing hypoxia (i.e. tracings with tachycardia associated with late decelerations and/or decreased variability). In our experience we did not observe such cases: this can be partly due to their low incidence in low-risk labor and to the limited sample size. Another reason could be the lack of use of ancillary methods (i.e. FBS and ST analysis) in our clinical practice, which can possibly lead to earlier intervention, before the EFM tracings presented multiple or complex features of abnormal EFM patterns.
We decided to focus our attention on well-defined FHR patterns, excluding cases with composite clinical and FHR features to avoid potential bias on outcome assessment. In this context, our study provides a meaningful information to understand the clinical significance of the most frequent suspicious FHR patterns occurring during the late stages of labor: this might be particularly useful to caregivers in managing low-risk pregnancies, especially when FBS is not available or technically feasible. In this setting, a correct interpretation of FHR tracings might allow an appropriate action before performing unnecessary operative interventions [25].
References
Goodwin TM, Belai I, Hernandez P et al (1992) Asphyxial complications in the term newborn with severe umbilical acidemia. Am J Obstet Gynecol 167:1506–1512
American College of Obstetricians and Gynecologists and American Academy of Pediatrics (2003) Neonatal encephalopathy and cerebral palsy: defining the pathogenesis and pathophysiology. American College of Obstetricians and Gynecologists, Washington, DC
Dildy GA (2005) Intrapartum assessment of the fetus: historical and evidence-based practice. Obstet Gynecol Clin N Am 32:255–271
Alfirevic Z, Devane D, Gyte GML (2006) Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database of Systematic Reviews Issue 3. doi:10.1002/14651858.CD006066
Beaulieu MD, Fabia J, Leduc B et al (1982) The reproducibility of intrapartum cardiotocogram assessments. Can Med Assoc J 127:214–216
Chauhan SP, Klauser CK, Woodring TC et al (2008) Intrapartum nonreassuring fetal heart rate tracing and prediction of adverse outcomes: interobserver variability. Am J Obstet Gynecol 199(623):e1
ACOG Practice Bulletin (2009) Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstet Gynecol 114:192–202
Bohem F (1999) Intrapartum fetal heart rate monitoring. Obstet Gynecol Clin N Am 96:623–639
Regione Emilia-Romagna Progetto 3 (2004) La sorveglianza del benessere fetale in travaglio di parto. Linea guida fondata su prove di efficacia. http://www.saperidoc.it/flex/cm/pages/ServeBLOB.php/L/IT/IDPagina/50
Landis J, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Williams KP, Galerneau F (2003) Intrapartum fetal heart rate patterns in the prediction of neonatal academia. Am J Obstet Gynecol 188:820–823
Williams KP, Galerneau F (2002) Heart rate parameters predictive of neonatal outcome in the presence of a prolonged deceleration. Obstet Gynecol 100:951–954
Malin GL, Morris RK, Khan KS (2010) Strength of association between umbilical cord pH and perinatal and long term outcomes: systematic review and meta-analysis. BMJ 340:c1471. doi:10.1136/bmj.c1471
Fleischer A, Schulman H, Jorgani N, Mitchell J, Randolph G (1982) The development of fetal acidosis in the presence of an abnormal fetal heart rate testing: the average for gestational age fetus. Am J Obstet Gynecol 144:55–60
Victory R, Penava D, da Silva O, Natale R, Richardson B (2004) Umbilical cord pH and base excess values in relation to adverse outcome events for infants delivering at term. Am J Obstet Gynecol 191:2021–2028
National Collaborating Centre for Women’s and Children’s Health (2007) Intrapartum care: care of healthy women and their babies during childbirth. RCOG Press, London
ACOG Practice Bulletin (2010) Management of Intrapartum Fetal Heart Rate Tracings. Obstet Gynecol 116:1232–1240
Macones GA, Hankins GD, Spong CY et al (2008) The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines. Obstet Gynecol 112:661–666
Gibb D, Arulkumaran S (2008). Fetal monitoring in practice, III edn, chap 8. Elsevier Health Sciences, London
Schifrin BS (2004) The CTG and the timing and mechanism of fetal neurological injuries. Best Pract Res Clin Obstet Gynecol 18:437–456
Frasch MG, Grasch MG, Frasch MG et al (2009) Measures of acidosis with repetitive umbilical cord occlusions leading to fetal asphyxia in the near-term ovine fetus. Am J Obstet Gynecol 200(200):e1
Myers RE (1972) Two pattern of perinatal brain damage and their conditions of occurrence. Am J Obstet Gynecol 112:246–276
Piquard T, Hsiung R, Mettauer M, Schaefer A, Haberey P, Dellenbach P (1988) The validity of fetal heart rate monitoring in the second stage of labor. Obstet Gynecol 72:746–751
Young BK, Weinstein HM (1976) Moderate fetal bradycardia. Am J Obstet Gynecol 126:271–275
Pehrson C, Sorensen JL, Amer-Wåhlin I (2011) Evaluation and impact of cardiotocography training programmes: a systematic review. BJOG 118:926–935
Acknowledgments
According to Italian legislation, observational studies do not require the approval of Independent Bioethics Committee. The study project numbered 86/05 has been approved by Technical Scientific Committee of Maternal and Child Health Research-Trieste (Italy) on February 28, 2007, and every study case gave the consent to attend the research project.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maso, G., Businelli, C., Piccoli, M. et al. The clinical interpretation and significance of electronic fetal heart rate patterns 2 h before delivery: an institutional observational study. Arch Gynecol Obstet 286, 1153–1159 (2012). https://doi.org/10.1007/s00404-012-2446-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-012-2446-8