Abstract
Introduction
There is no doubt that lifestyle factors can be detrimental to fertility. The aim of the present pilot study was to identify initial prevalence rates for behaviour-related fertility disorders in a clinical sample of couples wanting a child.
Methods
Between February 2010 and August 2010, all patients coming for the first time to Heidelberg University’s Women’s Hospital for consultation on involuntary childlessness were asked to fill out a questionnaire designed by the authors of this article. The questionnaire was based on a review of the relevant literature, with special reference to the latest research findings on behaviour detrimental to fertility. Of the 156 couples addressed, 110 women and 100 men took part in the study.
Results
For behaviour-related infertility, 9 % of the women and 3 % of the men in our sample were classified on the basis of BMI <18.5, sexual disorders, or abuse of anabolic steroids. If we include smokers, these figures increase: 11 % female smokers and 18 % male smokers. A further 19 % of the women practised sport to an excessive degree; and 26 % of the women and 53 % of the men had a BMI ≥25.
Discussion
The prevalence of behaviour-related fertility disorders should not be underestimated. For the prevention of behaviour-related fertility disorders, it is important to inform the population about lifestyle-mediated fertility risks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The impact of psychological factors influencing infertility is a controversial issue. It is certain that the concept of (solely) “psychogenic infertility” is no more of relevance today [4]. Once it became apparent from scientific studies that there were no grounds for the initial pathologization (mostly of the women) via ascription of certain personality features, research moved away from the “psychogenic infertility model” towards a “psychological consequences model” that focused on the psychological factors resulting in infertility and reproductive medicine treatment [39].
The first publication in Germany propagating a new definition of behaviour-related infertility was the article Psychosomatik in der Reproduktionsmedizin—Leitlinien (Psychosomatics in Reproductive Medicine—Guidelines), which appeared in 2000 ([32]; see [39]). Since 2006, this definition is also part of the German medical guidelines on assisted reproduction [8]. The definition encompasses the following behaviours that have a negative or restrictive effect on fertility:
-
1.
if, despite the desire for a child and relevant counselling from a doctor, a couple continues to display behaviour detrimental to fertility (e.g. over-/underweight; alcohol, nicotine, tablet abuse; highly competitive sport; extremely debilitating job stress);
-
2.
if a couple does not have intercourse on fertile days, or if a solely psychogenic sexual disorder is present;
-
3.
if a couple explicitly says yes to a medically indicated course of therapy for involuntary childlessness but then decides not to embark on it, even after thinking it over a lengthy period.
The present study is the first to investigate the prevalence of behaviour-related fertility disorders as described by this definition. Previously, behaviour-related fertility disorders were estimated on the basis of clinical observation to be responsible for 5 % of all cases of infertility [39], an assessment largely geared to the presence or absence of a functional sexual disorder [40].
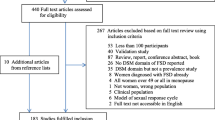
State of research
First, the authors of this article combed the relevant literature in a narrative review in search of the newest studies, reviews and meta-analyses providing information on up-to-date reference values and the present status of research on the topic of lifestyle factors and infertility. The numerous articles on the effects of lifestyle factors on IVF therapy or its outcome were left out, leaving only those publications discussing natural fertility. Among the psychosocial risk factors that are known to be detrimental to fertility and were discussed in the literature are age, smoking and extreme over- or underweight [10, 19, 20, 22]. Alcohol, caffeine, mental stress and excessive sporting activity are widely considered to be potentially detrimental factors, but research findings in the literature are anything but unanimous on this point.
Impact of body weight on fertility
Women
In their review, Homan et al. [19] confirm that the negative impact of over- and underweight is evidence based. According to WHO [37], the reference values are a body mass index (BMI) of ≥25 for overweight and <18.5 for underweight. In pathophysiological terms, the hormonal changes to the reproductive system as a result of an excessive or inadequate supply of energy cause anovulation or amenorrhoea and thus prevent pregnancy [14]. Underweight is one of the main diagnostic criteria for anorexia nervosa, a severe eating disorder with a high mortality rate. In their study of lifestyle factors with the participation of 2,112 pregnant women, Hassan and Killick [18] confirm that a BMI <19 or >25 involves a relative risk of 2.2 for needing more than 12 months before the onset of a pregnancy. As early as 1994, Rich-Edwards established that the risk of infertility increases with body weight. Investigating the Nurses′ Health Study (116,678 American hospital nurses), he found that the risk of infertility was highest in adipose women with a BMI of ≥ 32 [30].
Men
In men, by contrast, we have no firmly established findings on the effect of body weight on fertility [19, 22]. A study by Nguyen et al. [24] investigating 26,303 couples for connections between infertility and BMI indicated that BMI also had a significant impact on male fertility. In agreement with Rich-Edwards’ findings for women, Nguyen et al. established that in men the infertility rate also increased with body weight, peaking at a BMI of 32.4. By contrast, Paasch et al. [26] found a connection between BMI and fertility only in men between 20 and 30 years of age.
Impact of sport behaviour on fertility
Women
In the reviews, infertility due to sporting activity is evaluated differently. For instance, Derbyshire [11] finds that a low intake of energy combined with excessive sport favours infertility. Homan et al. [19], by contrast, point out that excessive sport has a beneficial effect when BMI is higher than it should be. None of these articles offer a precise definition of “excessive” sport. The only reference drawn upon is a study about the impact of sporting activity on the outcome of IVF therapy that describes >4 h of sport per week as detrimental to fertility [23]. Like the hormonal changes in the hypothalamic–pituitary axis caused by over-/underweight, extreme sport behaviour also has a negative effect on hormone balance and fertility [31, 35]. A major Norwegian study investigating the sport behaviour of 3,887 women from 1983 to 1986 and correlating this with the birth rate of those same women in 1995 to 1997 indicates that the conception rate declines with increasing frequency, duration and intensity of sporting activity [15]. These findings were independent of the confounding factors such as age, smoking or BMI, but were shown to be reversible during the follow-up period.
Men
Owing to the absence of comparable studies on the subject, none of the reviews or meta-analyses report on firmly established findings in connection with the impact of male sport behaviour on fertility. However, in line with the female pathomechanism, it is widely conjectured that intensive and prolonged physical training will also lead to hormone production alteration in men [25].
Impact of smoking on fertility
Women
Smoking is known to be a detrimental agent that affects fertility in a variety of ways [19, 20]. The meta-analysis by Waylen et al. [36] indicates that women smokers have significantly fewer pregnancies and significantly more miscarriages and ectopic pregnancies. None of the articles make any reference to a boundary value for the number of cigarettes per day. The analyses attribute to passive smoking the same detrimental impact as active smoking.
Men
The relevant articles are unanimous on the detrimental effect of smoking on all semen parameters [19, 20, 22]. Smoking impairs sperm production, sperm count, motility and fertilisation capacity, affects sperm morphology and involves a higher risk of damage to genetic information [13, 21, 28, 41].
Other factors detrimental to fertility
Alongside these well-investigated factors detrimental to fertility, there are others whose impact is yet to be adequately confirmed by scientific studies. They include frequently prescribed medicines like beta-blockers and anti-depressants, as well as anabolic steroids [2] used by men to build up muscle mass and known to have a highly adverse impact on sperm production [27]. In most studies, excessive alcohol consumption appears as a cofounder of smoking, so its effects on fertility are yet to be clarified [12, 22]. Caffeine consumption may adversely affect fertility, but the evidence is limited [19]. The meta-analysis by Klonoff-Cohen [20] shows that the findings on the fertility impact of mental stress are ambivalent (see also [39]). A most recent meta-analysis of 14 prospective studies with 3,583 infertile women came to the conclusion that emotional distress did not compromise the chance of becoming pregnant [7]. The impact of “extremely debilitating job stress” as given in the definition above has to be verified yet.
Sexual dysfunctions and sexual disorders
Whereas sexual disorders are to be treated by professionals (if the person affected and/or his/her partner suffers from this disorder), sexual dysfunctions (like infrequent sexual intercourse) are common and of a temporary nature only; these dysfunctions are usually not treated. According to Wischmann [40], sexual disorders as a cause of involuntary childlessness are relatively unusual. Sexual dysfunctions resulting from diagnosis and medical therapy are common in couples with fertility problems, with women more frequently affected than men [33]. The prevalence of sexual disorders in infertile couples remains unclear [29].
Methods
For the present study, the authors approached all the couples coming for the first time to Heidelberg University’s Women’s Hospital for counselling on involuntary childlessness. From February 2010 up to and including August 2010, all couples were asked before the first medical consultation to complete a questionnaire on psychological risk factors for infertility (plus the Self-Esteem and Relationship (SEAR) questionnaire on sexual disorders [9]; its evaluation will be published in another article). The design of this study and the selection of these questionnaires were approved by the Ethics Committee of the Medical Faculty of Heidelberg University.
The questionnaire on risk factors was designed by the authors of this study and contained questions on psychosocial risk factors for involuntary childlessness, such as on body image, sporting activity, alcohol drinking, smoking and nutrition, mental stress, sexual behaviour and medical diagnostics. The criteria of the questionnaire were geared to the factors described as detrimental to fertility in the literature examined beforehand (in the section state of research) and to the definition of behaviour-related infertility set out earlier. Alongside open questions like “My age: … years”, “My lowest weight (after puberty): … kg”; “My present weight: … kg”, it also contained questions with pre-formulated answer options, e.g. “In comparison with other women (men) of my size and age, I eat: substantially less/somewhat less/the same amount/somewhat more/substantially more” or “At present, I smoke: no cigarettes/1-5 cigarettes/day/5-20 cigarettes/day/more than 20 cigarettes/day”, or “Looking back over the last six months, I (my partner) could (realistically) have become pregnant: never/once/two to three times/four to five times/six times”.
We classified the questions on the sporting activity of the couples into the categories “no”, “moderate” and “excessive” activity. Here, we took our bearings from a compendium of physical activity [1] in which specific sporting activities are categorised according to the energy consumption they involve (MET = metabolic activity). Less then 3 METs were rated as “no sporting activity”, 3–6 METs as moderate activity (e. g. golf or table tennis) and more than 6 METs as vigorous activity (e.g. boxing or squash). The compendium was developed to improve comparability between information on sporting activity volunteered in the framework of scientific studies. In addition, patients indicating that they spent more than 4 h per week on moderate sporting activity—compared to the usually recommended 2.5 h of moderate sporting activity per week [17]—were placed in the next higher category.
The evaluation of the responses was undertaken via frequency and percentage calculations, median values and range, the χ2 test and the t test for independent samples with the aid of the statistics programme SAS 9.2.
Responder/non-responder analysis
A total of 156 couples were approached, the response rate was 67.3 %. Anamnestic data from the patients’ files were used to investigate for differences between participants and non-participants. No significant difference between participants and non-participants was identified in any relevant variable, so selectivity in the study population is unlikely.
Results
Age
The average age of the women was 34 years (range 22–46) and that of the men 37.5 years (range 22–63). In this study population, the proportion of women >35 years was close to 40 % and that of the men >45 years, close to 6 %. At this age, female fertility is already 50 % lower than it is in women of 25 years [34]. On average, the unfulfilled desire for a child had lasted for 2.5 years.
Under- or overweight
The BMI distribution was such that 7.3 % of the women were underweight (BMI <18.5), while a quarter of the women and over half the men were overweight (BMI >25). Eating behaviour: 6.8 % of the women and 7.4 % of the men indicated that they ate less or much less than others (of the same sex, size and age), while one-fifth of the women and over one-third of the men felt that they ate more or substantially more.
Sport
As much as 65 % of the women and 41 % of the men engaged regularly in sporting activity, on average 2.6 h a week. Of these, over one-third of the men and women practised sport to a vigorous degree (according to the definition above) averaging 4.4 h per week.
Smoking, alcohol consumption and medication
As much as 10.9 % of the women and 18.4 % of the men smoked more than five cigarettes a day, while 4.6 % of the women and 9.3 % of the men said that they drank alcohol more than 2×/week; 8.4 % of the women regularly took medicines detrimental to fertility and a further 2.8 % on rare occasions, while 2 % of the men indicated that they were taking anabolic steroids regularly.
Psychological stress
On a scale from 0 to 5, the patients’ subjective stress assessment ranged from 11.2 % at the lowest stress level and 16.9, 21.8, 33 and 10.7 % at the intermediate stress levels to 6.3 % at the highest stress level. The women tended to refer more frequently to involuntary childlessness as the cause of distress, while most of the men blamed it on their jobs.
Sexuality
In the assessment of realistic pregnancy likelihood over the last 6 months, 41.7 % of the women indicated that conception would have been possible on between zero and three occasions; 11.5 % of the patients mentioned that they had failed to take advantage of the woman’s fertile days on 4–6 occasions over the last 6 months. Apart from medical (e.g. no ovulation) or logistic reasons (e.g. absence of a partner for job reasons), half of the reasons given for this came under the headings “no inclination”, “psychological grounds” and “sexual disorders”.
Diagnostic investigations
Almost 10 % of the couples said that despite having adequate time, they had delayed a diagnostic investigation for involuntary childlessness (e.g. a semen analysis) for 3 months or more despite the advice given to them by their doctors.
Prevalence of behaviour-related fertility disorders in our sample
In the following, we distinguish between couples whose responses suggest that they may be affected by behaviour-related fertility disorders (at least in part) and couples most probably affected by that condition (in accordance with the definition referred to earlier). Assessment of the prevalence of behaviour-related fertility disorders took place stepwise with increasing stringency of the definition.
First, we singled out all patients fulfilling at least one the following criteria for possible behaviour-related risk factors:
-
BMI <18.5 in women
-
excessive sport (in women)
-
>5 cigarettes/day (both partners)
-
consumption of anabolic steroids (in men)
-
sexual disorders (dyspareunia, sexual abstention for 6 months, reference to sexual disorder/s in the questionnaire)
Outcome
In accordance with this definition, 42.7 % of the female patients (see Fig. 1) and a quarter of the men (25 %; see Fig. 2) were evaluated as probably behaviour-related infertile. Among the women, 5.5 % displayed two or more risk factors. This was the case in only 1 % of the men.
In the next stage, the group of smokers was excluded from the overall evaluation on account of the addiction potential (in our view, smoking is not a “lifestyle” factor that is easy to modify), although scientific studies have established beyond doubt that smoking is detrimental to fertility. Excessive sport on the part of women (which we cannot assume in every case to be known as detrimental to fertility) and sexual disorders that have not been precisely diagnosed (this includes “dyspareunia” in the patient files) were also excluded.
Finally, after the evaluation of each individual aspect investigated, the following prevalence of behaviour-related fertility disorders was established: 9.1 % of the women (with BMI <18.5 or a clearly identified sexual disorder; see Fig. 1) and 3 % of the men (with anabolic steroid abuse or a clearly identified sexual disorder; see Fig. 2) in our sample were very likely to be suffering from behaviour-related fertility disorders (in accordance with the definition given above).
Discussion
The potential limitations of the study are as follows. First, the definition of behaviour-related fertility disorders referred to earlier includes the case where “despite (…) relevant counselling from a doctor, a couple continues to display behaviour detrimental to fertility”. In the study population, it was not possible to establish whether the first consultation at Heidelberg University’s Hospital for Women had been preceded by counselling from a doctor pertaining to factors detrimental to fertility. Accordingly, this group may not correspond to the population required by the definition. Second, our sample consisted of couples undergoing medical investigation in a university hospital. Given that not all infertile couples seek medical treatment [6], the generalizability of our results to other samples of infertile couples might be restricted. Third, the evaluation of behaviour-related fertility disorders was based on the couples’ self-assessment in the questionnaire and not on a medical assessment, so the prevalence of behaviour-related fertility disorders might be underestimated in this pilot study. One could also expect that regarding sports, the reported time might be overestimated and regarding smoking the number of cigarettes might be underestimated.
In connection with the passage “if (…) a couple continues to display behaviour detrimental to fertility” in the definition, the question arose as to which of the lifestyle factors can safely be classified as detrimental to fertility. Overweight in particular has become so common that it can almost be regarded as “normal”. According to the WHO [38], about two-thirds of the women and about three-quarters of the men in Germany (30 years and older) are overweight (for obesity 30.9 % of the women and 31.3 % of the men). Overweight causes a number of illnesses and is also one of the most difficult eating disorders to deal with therapeutically. Underweight also has a pathogenic aspect. Of the eight women in our study population who were underweight, three also suffered (according to anamnestic enquiries) from an eating disorder. We can thus assume underweight to be an illness in these cases. A similar problem is posed by cigarettes, which are one of the most frequently consumed drug-containing substances and of course display major addiction potential.
In the calculation of the proportion of body fat, we did not use the waist measurement approach recently introduced but the BMI, so as to be able to compare our findings with those of existing studies. As the BMI does not allow for any distinction between weight from body fat and weight from muscle mass, it does not necessarily reflect the actual body fat content in every patient. It should be noted that patients indicating a BMI >25 and engaging in excessive sporting activity were not evaluated as behaviour-related infertile, as weight reduction enhances fertility in overweight patients. Also, the questionnaire did not ask how many years the relevant responders had been practising excessive sport, and so an evaluation in terms of “lifestyle factor” could only be approximate.
The indications on the prevalence of sexual disorders can also only be taken as an approximation, as not all the ICD-10 criteria of the respective sexual disorder were systematically addressed. Of the patients probably suffering from a sexual disorder, only those who fully satisfied the criteria for sexual disorders were included in the final outcome. How high the proportion of sexual disorders really is will need to be investigated in future studies on the basis of more precise criteria.
Despite these limitations, the study clearly indicates that given this prevalence of factors detrimental to fertility, knowledge about the impact of lifestyle in the population as a whole and particularly in couples who approach a reproductive medicine centre for advice/treatment is either inadequate or has not been properly taken into account. Precisely those risk factors established in meta-analyses as detrimental to fertility (smoking, excessive alcohol consumption, BMI) are in fact susceptible to modification. In addition, these factors not only impede natural pregnancy, but also interfere with the course of infertility therapy and its outcome [19, 20].
Accordingly, careful anamnesis is indispensable, as in any medical interview. At the first consultation attended by couples affected by involuntary childlessness, it is important to enquire into modifiable lifestyle factors. This should be followed by a thorough anamnestic enquiry into sexuality. Studies indicate, however, that even specialist centres frequently fail to address the sexuality aspect [40]. An enquiry into the diagnostics routines of local German gynaecologists in their surgeries revealed that in most cases, there was no routine anamnesis on the subject of sexuality. Instead, 70 % of the patients bring up their sexual problems of their own accord [5]. In most cases, questions on subjective experience of sexuality, cohabitation frequency or non-contraceptive intercourse remain unaddressed.
It is certainly true that the general population needs to be enlightened on these points. Alongside couples affected by involuntary childlessness, an enlightenment drive for preventive purposes should naturally be angled primarily at the younger members of society. Ample proposals for the prevention of involuntary childlessness and the improvement of anamnesis have been advanced. Anderson et al. [3] and Berner [5] suggest devising health programmes to help the relevant couples to alter behaviours detrimental to fertility and thus prevent involuntary childlessness. A further task for medical science would be to draw up guidelines on behaviour-related infertility for both physicians and couples so as to facilitate the initial stages of counselling.
Conclusion and outlook
According to the definition referred to at the outset, 9 % of the women and 3 % of the men who attend their first interview in connection with involuntary childlessness are very likely affected by behaviour-related fertility disorders. If we include the widespread risk factors of overweight and smoking, the prevalence figures soar. An additional 10 % of the women and 2 % of the men may be suffering from sexual disorders. These figures indicate that the time has come to sensitise the population on these points and enlighten them on the causes and consequences of behaviour-related fertility disorders.
The findings suggest that the women are more often affected by this diagnosis than men. In contrast to women, we still know very little about the impact of male age on problems connected with the desire for a child. Meta-analyses have so far failed to clarify the impact of too high a BMI in men, and at present the findings on male sport behaviour are even more contradictory. This means that, on the one hand, more research is required on these points and, on the other, preventive measures counteracting behaviours detrimental to fertility in the general population (e. g. [16]) need to be established or stepped up.
References
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ et al (2000) Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 32(9 Suppl):S498–S504
Anderson K, Nisenblat V, Norman R (2010) Lifestyle factors in people seeking infertility treatment—a review. Aust NZ J Obstet Gynaecol 50(1):8–20
Anderson K, Norman R, Middleton P (2010) Preconception lifestyle advice for people with subfertility. Cochrane Rev 11
Apfel RJ, Keylor RG (2002) Psychoanalysis and infertility—myths and realities. Int J Psychoanal 83:85–103
Berner M, Schmidt E, Weinhäupl C, Günzler C, Kriston L, Zahradnik HP (2010) Prävalenz, Diagnostik und Therapie weiblicher sexueller Funktionsstörungen in der gynäkologischen Praxis—Eine deutschlandweite Repräsentativbefragung. Geburtsh Frauenheilk 70(04):281–287
Boivin J, Bunting L, Collins JA, Nygren KG (2007) International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod 22(6):1506–1512
Boivin J, Griffiths E, Venetis CA (2011) Emotional distress in infertile women and failure of assisted reproductive technologies: meta-analysis of prospective psychosocial studies. Br Med J 342:d223
Bundesärztekammer (2006) (Muster-)Richtlinie zur Durchführung der assistierten Reproduktion—Novelle 2006. Dtsch Ärztebl 20:A1392–A1403
Cappelleri JC, Althof SE, Siegel RL, Shpilsky A, Bell SS, Duttagupta S (2004) Development and validation of the self-esteem and relationship (SEAR) questionnaire in erectile dysfunction. Int J Impot Res 16(1):30–38
Centers for Disease Control and Prevention (CDC) (2011) Reproductive Health. Infertility FAQs. http://www.cdc.gov/reproductivehealth/Infertility/index.htm
Derbyshire E (2007) Taking it a step too far? Physical activity and infertility. Nutr Food Sci 37(5):313–318
Eggert J, Theobald H, Engfeldt P (2004) Effects of alcohol consumption on female fertility during an 18-year period. Fertil Steril 81(2):379–383
Frey KA, Navarro SM, Kotelchuck M, Lu MC (2008) The clinical content of preconception care: preconception care for men. Am J Obstet Gynecol 199(6, Suppl 2):S389–S395
Grodstein F, Goldman MB, Cramer DW (1994) Body mass index and ovulatory infertility. Epidemiology 5(2):247–250
Gudmundsdottir SL, Flanders WD, Augestad LB (2009) Physical activity and fertility in women: the North-Trondelag Health Study. Hum Reprod 24(12):3196–3204
Hammiche F, Laven JSE, van Mil N, de Cock M, de Vries JH, Lindemans J, et al (2011) Tailored preconceptional dietary and lifestyle counselling in a tertiary outpatient clinic in the Netherlands. Hum Reprod 24(9):2432–2441
Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al (2007) Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 116(9):1081–1093
Hassan MAM, Killick SR (2004) Negative lifestyle is associated with a significant reduction in fecundity. Fertil Steril 81(2):384–392
Homan GF, Davies M, Norman R (2007) The impact of lifestyle factors on reproductive performance in the general population and those undergoing infertility treatment: a review. Hum Reprod Update 13(3):209–223
Klonoff-Cohen H (2005) Female and male lifestyle habits and IVF: what is known and unknown. Hum Reprod Update 11(2):180–204
Künzle R, Mueller MD, Hänggi W, Birkhäuser MH, Drescher H, Bersinger NA (2003) Semen quality of male smokers and nonsmokers in infertile couples. Fertil Steril 79(2):287–291
Li Y, Lin H, Li Y, Cao J (2011) Association between socio-psycho-behavioral factors and male semen quality: systematic review and meta-analyses. Fertil Steril 95(1):116–123
Morris SNMD, Missmer SAS, Cramer DWMD, Powers RDMD, McShane PMMD, Hornstein MDMD (2006) Effects of lifetime exercise on the outcome of in vitro fertilization. Obstet Gynecol 108(4):938–945
Nguyen RHN, Wilcox AJ, Skjaerven R, Baird DD (2007) Men’s body mass index and infertility. Hum Reprod 22(9):2488–2493
Olive DL (2010) Exercise and fertility: an update. Curr Obst Gynaecol 22:259–263
Paasch U, Grunewald S, Kratzsch J, Glander H-J (2010) Obesity and age affect male fertility potential. Fertil Steril 94:2898–2901
Pasqualotto FF, Lucon AM, Sobreiro BP, Pasqualotto EB, Arap S (2004) Effects of medical therapy, alcohol, smoking, and endocrine disruptors on male infertility. Rev Hosp Clin Fac Med S Paulo 59:375–382
Ragheb AM, Sabanegh ES (2009) Smoking and male fertility: a contemporary review. Arch Med Sci 5(1A):S13–S19
Read J (2011) Sexual problems and infertility. BICA Publications
Rich-Edwards WJ, Goldman BM, Willett CW, et al (1994) Adolescent body mass index and infertility caused by ovulatory disorder, vol 171. Elsevier, New York
Rich-Edwards JW, Spiegelman D, Garland M, Hertzmark E, Hunter DJ, Colditz GA et al (2002) Physical activity, body mass index, and ovulatory disorder infertility. Epidemiology 13(2):184–190
Strauß B, Bettge S, Bindt C, Brähler E, Felder H, Gagel D et al (2000) Psychosomatik in der Reproduktionsmedizin. Leitlinien. Reproduktionsmed 16(5):326–331
Tao P, Coates R, Maycock B (2011) The impact of infertility on sexuality: a literature review. Australas Med J 4(11):620–627
van Noord-Zaadstra BM, Looman CW, Alsbach H, Habbema JD, te Velde ER, Karbaat J (1991) Delaying childbearing: effect of age on fecundity and outcome of pregnancy. Br Med J 302(6789):1361–1365
Warren M, Perlroth N (2001) The effects of intense exercise on the female reproductive system. J Endocrinol 170(1):3–11
Waylen AL, Metwally M, Jones GL, Wilkinson AJ, Ledger WL (2009) Effects of cigarette smoking upon clinical outcomes of assisted reproduction: a meta-analysis. Hum Reprod Update 15:31–44
WHO (1997) BMI classification. http://www.who.int
WHO (2011) Prevalence of overweight & obesity map. http://www.who.int/topics/obesity/en/. Retrieved 16 June 2011 from http://www.who.int/topics/obesity/en/
Wischmann T (2003) Psychogenic infertility—myths and facts. J Assist Reprod Genet 20(12):485–494
Wischmann TH (2010) Sexual disorders in infertile couples. J Sex Med 7(5):1868–1876
Zenzes MT, Bielecki R, Reed TE (1999) Detection of benzo(a)pyrene diol epoxide-DNA adducts in sperm of men exposed to cigarette smoke. Fertil Steril 72(2):330–335
Acknowledgments
We are grateful to the women and men for their willingness to participate in this study.
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schilling, K., Toth, B., Rösner, S. et al. Prevalence of behaviour-related fertility disorders in a clinical sample: results of a pilot study. Arch Gynecol Obstet 286, 1307–1314 (2012). https://doi.org/10.1007/s00404-012-2436-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-012-2436-x