Abstract
Purpose
The aim of the study was to assess the distribution of positive tilt testing (TT) throughout the menstrual cycle and to determine if the phase of menstrual cycle contributes to the duration of the loss of consciousness.
Methods
TT results of 183 premenopausal women, aged 29.5 ± 9.8 years, were studied. The menstrual cycle was divided into four phases based on the first day of the last menstrual bleeding: perimenstrual (M), preovulatory (F), periovulatory (O) and postovulatory (L).
Results
Positive TT results were equally distributed. In patients with TT in O phase, the highest percentage of NTG provocation was needed. Patients in L phase had significantly lower incidence of cardioinhibitory reaction. The longest duration of loss of consciousness was in the M phase. Multiple regression analysis revealed that the duration of loss of consciousness during positive TT was significantly associated with higher number of syncopal events, TT performed in M phase and lower heart rate at TT termination. Cardiodepressive type of neurocardiogenic reaction was more frequent during M and O phase than during L phase.
Conclusions
The distribution of positive TT results as well as syncope and presyncope does not differ throughout the menstrual cycle. Diagnostic TT in premenopausal women with unexplained syncope could be performed irrespective of the phase of menstrual cycle. TT has similar sensitivity throughout the menstrual cycle. During the postovulatory phase, cardioinhibitory reaction is less frequent than in M and O phases. The duration of loss of consciousness is longer during the M phase of the menstrual cycle independently of the higher syncope number and lower heart rate at TT termination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Hormonal changes during menstrual cycle may have impact on the occurrence of cardiovascular events: clustering myocardial infarction in the follicular phase as well as supraventricular tachycardias in the perimenstrual period in premenopausal women. Both estrogens and progesterone exert effects on the cardiovascular system by influencing the autonomic nervous system activity and the plasma volume regulation, which can also change the susceptibility to neurocardiogenic reflex provocation and its course. The other possibility of the relationship between the level of female sex hormones and susceptibility to neurocardiogenic reflex includes their action through the central serotonin neural system, which may be involved in the provocation of neurocardiogenic reflex [1, 2].
Despite the lack of differences both in orthostatic tolerance and cardiovascular control at the follicular and luteal phases of the menstrual cycle in healthy women, it could not be excluded that in vasovagal patients the susceptibility to neurocardiogenic reflex provocation and its course depends on the phase of the menstrual cycle [3, 4].
The aim of the study was to assess the distribution of the positive and negative tilt testing (TT) results defined as syncope and presyncope throughout the menstrual cycle and to determine whether the phase of the menstrual cycle influences the duration of the loss of consciousness during TT-induced syncope. The primary end point was to obtain a positive TT result depending on the phase of the menstrual cycle. The secondary end point involved assessing the positive TT on the basis of syncope duration. The division of TT results into a presyncope and syncope is concordant with the syncope of zero duration and a duration longer than zero, respectively. The VASIS classification constituted the tertiary end point owing to the fact that such a classification was aimed at providing an assessment of the changes to the heart rhythm only, and not the extent of global hemodynamic disorders.
Materials and methods
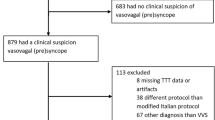
The study group consisted of 183 premenopausal women, cycling regularly every 21–36 days, aged 29.5 ± 9.8 years, referred to perform the TT by attending doctors because of recurrent unexplained presyncopal or syncopal episodes. Subjects were not taking any medications including estrogen/progesterone compound for contraception or hormonal and obstetric reasons. Patients with significant anemia were not included into the study.
The full medical history, including the number of syncopal spells, traumatic injuries related to syncope, blood phobia, the relationship between the syncopal episodes and menstrual cycle, and concomitant diseases and treatment, was taken in each case.
Each patient was asked about the first day of her last menstrual bleeding and about the regularity of the menstrual cycle. Only women with regular cycles between 21 and 36 days were included in further analyses. The phase of menstrual cycle when TT was performed was established for each patient.
The menstrual phase was calculated on the basis of the first day of the last menses and the cycle length, both of which were asked during history taking. The menstrual cycle phase was classified as follicular between 1st and −15th and luteal between −14th and the last day of the cycle, and the second division as perimenstrual between −3rd to +4th day (M), preovulatory between +5th day and −18th (F), ovulatory between −17th and −11th (O) and postovulatory between the −10th and −4th (L). Shorter or longer cycles are generally reflected more strongly in the follicular phase than in the luteal one [5].
TT was performed according to the Italian protocol (20 min of passive tilting at 60°, 0.4 mg NTG administrations if necessary, 15 min of tilting) [6].
ECG Holter monitoring using Optima Jet Oxford system and BP monitoring with the oscillometric method with cardiomonitor (Biazet Poland in cooperation with S&W Medico Teknik, Denmark) were performed.
We terminated TT after syncope or presyncope provocation or completion of the whole protocol. TT was terminated at presyncope when at least a 2-min period of immeasurable blood pressure or systolic blood pressure below 80 mmHg with very intense presyncope symptoms occurred [7, 8].
For each patient, the reason for the termination of TT was noted as a completion of TT–negative TT, presyncope or syncope provocation, as well as the heart rate at TT termination when the TT was positive. Each patient was inquired about the reproduction of spontaneous symptoms during TT. The type of provoked neurocardiogenic reaction was determined according to the VASIS criteria as cardioinhibitory, mixed or vasodepressive [9].
-
Mixed: heart rate falls at the time of syncope but the ventricular rate does not fall to <40 beats/min, or falls to <40 beats/min for <10 s with or without asystole of <3 s.
-
Cardioinhibition: heart rate falls to a ventricular rate <40 beats/min for more than 10 s and/or asystole of more than 3 s occurs.
-
Vasodepression: blood pressure falls. Heart rate does not fall by more than 10 % from its peak at the time of syncope.
The patients were divided into four groups taking into account the phase of the menstrual cycle when TT was performed.
Statistical analysis
The variables were presented as means and their standard deviations for the continuous variables with normal distribution, or medians and interquartile ranges in the case of lack of normal distribution. The discrete variables were presented as percentages or numbers of cases.
Statistical power analysis
According to the literature data, TT sensitivity amounts to 85 %. In our study, the sensitivity level was 83 % which constitutes a very similar value to those mentioned by other authors. The decrease in TT sensitivity by 25 % seems to be clinically significant. Statistical power analysis indicates the necessity of subjecting a group of 31 people to research for the purposes of detecting the significant (p < 0.05) decrease in the positive TT outcomes by 25 % at the 0.80 level of study power.
The average duration of loss of consciousness during TT is about 20 s. Making the syncope duration longer by 10 s seems to be considerable from the clinical point of view. The sample size required to detect the change in the loss of consciousness duration lasting 10 s is n = 17 (power of 80 %).
The significance of the differences between studied variables was assessed with t Student’s test, U Mann–Whitney test and Chi-square test with or without Yates correction, as appropriate.
For the statistical analysis, the syncope number was dichotomized into at least three or less than three events, according to the median number of syncopal spells in the medical history in the studied population.
The logistic regression analysis was performed to find the association between the neurocardiogenic reaction provocation and the age, syncope number in the medical history (also after dichotomization into less than three and at least three syncopal spells), as well the phase of the menstrual cycle while TT was performed. The second logistic regression was performed in the subgroup with positive TT to find the association between syncope provocation and the age, syncope number in medical history, necessity of NTG use during TT, reproduction of the symptoms and the phase of the menstrual cycle during TT.
The multiple regression analysis was performed to find the association between the duration of the loss of consciousness and age, phase of menstrual cycle, number of syncopal spells in the medical history, instrumentation–injection blood phobia and the use of NTG during TT. The other multiple regression analysis was performed to find the association between the pause duration and age, phase of menstrual cycle, number of syncopal spells in the medical history, instrumentation–injection blood phobia and the use of NTG during TT.
A p value below 0.05 was considered to be statistically significant.
Results
In the study, 103 tilt tests were carried out in the follicular phase of the cycle (defined as a time from the 1st day of the cycle until the 15th day before the due date of an expected menstruation), while 80 tests were carried out in the luteal phase of the cycle (defined as the last 14 days of the cycle). The frequency of the positive test outcome in the follicular phase amounted to 87.4 %, while in the luteal phase it was 76.3 %; p = NS.
Table 1 presents the demographics, clinical and TT data in the studied population divided into groups according to the follicular and luteal phases of the menstrual cycle.
The demographics, past medical history and TT data of the patients divided into four groups on the basis of four phases of the menstrual cycle when TT was performed are presented in Table 2. In patients with TT in the periovulatory phase, the highest percentage of NTG provocation was needed. The longest duration of the loss of consciousness was observed in the perimenstrual phase.
In the postovulatory group, the cardioinhibitory reaction was less frequent than in the perimenstrual and ovulatory phases.
The distribution of the duration of menstrual cycles was as follows: 21–22 days—10.9 %; 25–26 days—10.9 %, exactly 28 days—45.7 %, 28–32 days—23 % and 33–36 days—8.7 %. The timing of TT and the characteristics of the menstrual cycle for each patient did not confer any doubt regarding the phase of the menstrual cycle.
The comparison of frequencies of the positive and negative TT results across the menstrual cycle did not differ significantly (Fig. 1). Furthermore, the frequencies of syncope and presyncope as a result of TT did not differ significantly throughout the menstrual cycle. There was also no relationship between the syncopal episodes and phases of the menstrual cycle in women able to remember the appropriate timing of their last syncopal episode.
The distribution of the negative and positive TT results according to VASIS classification during the menstrual cycle is depicted in Fig. 2.
Logistic regression analysis did not reveal any relationship between the phase of menstrual cycle while TT was performed and the positive TT result. Logistic regression analysis revealed that the syncope as a result of TT in comparison with presyncope was related to the higher number of syncopal events in the medical history (OR, 2.25; 95 % CI 1.03–4.9; p < 0.01) and the history of instrumentation–injection blood phobia (OR, 2.7; 95 % CI 1.38–5.28; p < 0.01).
The multiple regression analysis revealed that the duration of loss of consciousness during positive TT was significantly associated with a higher number of syncopal events, the TT performed at the perimenstrual phase and the lower heart rate at TT termination as presented in Table 3.
In Fig. 3 the plot of the duration of the loss of consciousness against the day of the menstrual cycle when TT was performed is depicted in patients with higher and lower number of syncopal events in the medical history.
The relationship between spontaneous syncopal events and the menstrual cycle was established in 38 patients, who remembered the exact timing of the syncope, the cycle length and the date of menstruation in the preceding 2 months. In 10 women, syncope occurred in the perimenstrual phase, in 12 in the luteal phase, in 9 in the preovulatory phase and in 7 women in the periovulatory phase of the menstrual cycle. The frequency of syncopal events did not differ significantly among the cycle phases. Furthermore, five women reported that they fainted during menstruation in the past. Altogether, the relationship was established in 43 women who were only 23.5 % of the study group. A total of 65 women were pregnant in the past and 64 of them bore at least one child, and one woman had one miscarriage. Nine women (13.6 %) had at least one syncopal spell during pregnancy and two had profound presyncopal events. There was a syncopal event after delivery in three women. The patients were not asked about abortions.
Discussion
The main finding of the study was that throughout the menstrual cycle, the susceptibility to the provocation of neurocardiogenic reflex was stable. The sensitivity of the TT does not depend on the phase of the menstrual cycle. This suggests that there are no contraindications to perform the diagnostic TT at any time during the menstrual cycle without any risk of significant changes in the results obtained. However, the risk of developing a long-lasting loss of consciousness increases during the perimenstrual phase independently of the syncope number in the medical history and the heart rate at the termination of TT.
The lack of effect of the phase of the menstrual cycle on the TT result is concordant with the study of Meendering et al. [3], who showed that the adaptation to the vertical posture was not related to the phase of the menstrual cycle. Similarly, Claydon et al. [4] have reported that there is no difference in cardiovascular control at the follicular and luteal phases of the menstrual cycle in healthy women.
The second finding is that during the postovulatory phase, cardioinhibitory reaction is less frequent than in the perimenstrual and ovulatory phases. It may be related to the hormonal changes during the menstrual cycle. The hormonal changes during the menstrual cycle have been shown to impact on such factors as sympathetic baroreflex sensitivity, circulating catecholamine concentrations, sensitivity of sympathetic adrenergic receptors and plasma volume [3]. Estrogens seem to enhance parasympathetic activity [10, 11], and progesterone alone or in combination with estrogen may lead to the activation of sympathetic activity. Resting levels of circulating plasma norepinephrine have been reported to be higher during the luteal phase of the menstrual cycle when both estrogen and progesterone concentrations are elevated [12–16]. Both estrogen and progesterone have profound effects on plasma volume which is highest in the menstrual cycle during the postovulatory phase. Furthermore, estradiol receptors are abundant in the central nervous system. Central mechanisms may be more important than peripheral ones in the pathogenesis of the vasovagal syncope [17]. Estradiol enhances the brain serotoninergic and noradrenergic activity. Selective serotonin reuptake inhibitors are successful agents for the treatment of vasovagal syncope via a reduction in the central serotoninergic activity during its long-term administration. On the other hand, acute intravenous administration of clomipramine, a selective serotonin reuptake inhibitor, may be even more effective in neurocardiogenic reflex provocation than nitroglycerin [2, 17]. Serotonin surges may occur in humans before syncope, and chronic treatment with serotonin reuptake inhibitors decreases the sensitivity of serotonin receptors, with the subsequent prevention of vasovagal syncope. A low serotoninergic activity during premenopausal activity could in turn increase the sensitivity of serotoninergic receptors. Different subtypes of serotonin-receptor antagonists reduce the sympathetic and adrenomedullary response to hypotension [18]. An increased central serotoninergic activity was suggested to play a role in the sudden inhibition of sympathetic activity responsible for the genesis of vasovagal syncope.
We have presumed that similarly as during postpartum period, which is a risk factor for syncope, [19] the perimenstrual phase with a relatively low level of female sex hormones would be associated with a higher susceptibility to neurocardiogenic reflex provocation by tilt testing.
However, we have not revealed any differences in the ratio of positive TT results between different phases of the menstrual cycle. On the other hand, the duration of the loss of consciousness was longer when neurocardiogenic reflex was provoked during the period of low levels of female sex hormones. During neurocardiogenic reflex, sympathetic withdrawal is present and a high level of female sex hormones may facilitate the restoration of the blood pressure to the level required for regaining consciousness.
The activity of the sympathetic nervous system may modulate the course of neurocardiogenic reflex. While neurocardiogenic reflex is provoked, increased sympathetic activity diminishes hemodynamic disturbances. Yohimbine-induced enhancement of sympathetic tone, assessed as norepinephrine plasma concentration and muscle sympathetic nerve activity in patients with vasovagal syncope, improves orthostatic tolerance. An increase of the sympathetic activity achieved by counterpressure maneuvers during the presyncopal phase of TT may change the course of the neurocardiogenic reflex and prevent the loss of consciousness [20]. Although beta-blockers may change the course of neurocardiogenic reflex and predispose to the cardiodepressive type of neurocardiogenic reaction, they do not change the susceptibility to the provocation of the neurocardiogenic reflex. During the luteal phase, the sympathetic tone is higher than during the follicular phase, which may contribute to the shortening of the QT interval [13].
Minson et al. [21] have demonstrated that the hormonal fluctuations occurring during the normal menstrual cycle alter the baroreflex regulation of the sympathetic outflow, but do not do so with the baroreflex regulation of the heart rate or the transduction of a sympathetic nerve activity into vascular resistance. Our results in the light of their findings indicate the significance of the baroreflex regulation of sympathetic outflow on the duration of the loss of consciousness during a neurocardiogenic reflex.
Limitations
The main limitation of our study was the lack of verification of the phase of the menstrual cycle by the measurements of circulating concentrations of estradiol and progesterone. However, our patients had a regular menstrual cycle and we presumed that the calendar method has enough precision in such circumstances to define the phase of the menstrual cycle. Our assumptions regarding the possibility of the accurate assessment of the phase of the menstrual cycle by the calendar method are confirmed by the results of other studies where all menstrual cycle phases were verified by measuring circulating concentrations of estradiol, progesterone and sometimes gonadotropins. Very few cases, if any, were discarded due to the anovulatory menstrual cycle hormonal pattern [3, 21, 22]. We are incapable of assessing whether the age at menarche and a previous use of oral contraceptives influence TT because such data have not been collected.
Only few patients were able to recollect the appropriate timing of their last syncope with regard to the phase of menstrual cycle. Therefore, any potential relationship could not be established.
Conclusions
-
1.
The distribution of the positive and negative TT results as well as syncope and presyncope as a result of TT does not differ throughout the menstrual cycle.
-
2.
The diagnostic TT in premenopausal women with unexplained syncope could be performed irrespective of the phase of the menstrual cycle. The sensitivity of TT does not depend on the phase of the menstrual cycle.
-
3.
The duration of the loss of consciousness is longer during the perimenstrual phase of the menstrual cycle independently of the higher syncope number and the lower heart rate at TT termination.
-
4.
During postovulatory phase, the cardioinhibitory reaction is less frequent than in perimenstrual and ovulatory phases.
-
5.
The fluctuation in the levels of the female sex hormones does not change the susceptibility to the neurocardiogenic reflex provocation, but influences its course assessed as the VASIS type of the neurocardiogenic reaction and the duration of the loss of consciousness.
References
Bethea CL, Lu NZ, Gundlah C, Streicher JM (2002) Diverse actions of ovarian steroids in the serotonin neural system. Front Neuroendocrinol 23:41–100
Theodorakis GN, Markianos M, Zarvalis E, Livanis EG, Flevari P, Kremastinos DT (2000) Provocation of neurocardiogenic syncope by clomipramine administration during the head-up tilt test in vasovagal syndrome. J Am Coll Cardiol 36:174–178
Meendering JR, Torgrimson BN, Houghton BL, Halliwill JR, Minson CT (2005) Menstrual cycle and sex affect hemodynamic responses to combined orthostatic and heat stress. Am J Physiol Heart Circ Physiol 289:H631–H642
Claydon VE, Younis NR, Hainsworth R (2006) Phase of the menstrual cycle does not affect orthostatic tolerance in healthy women. Clin Auton Res 16:98–104
Fehring RJ, Schneider M, Raviele K (2006) Variability in the phases of the menstrual cycle. J Obstet Gynecol Neonatal Nurs 35:376–384
Bartoletti A, Gaggioli G, Menozzi C, Bottoni N, Del Rosso A, Mureddu R et al (1999) Head-up tilt testing potentiated with oral nitroglycerin: a randomized trial of the contribution of a drug-free phase and a nitroglycerin phase in the diagnosis of neurally mediated syncope. Europace 1:183–186
Wieling W, van Lieshout JJ, ten Harkel AD (1998) Dynamics of circulatory adjustments to head up tilt and tilt back in healthy and sympathetically denervated subjects. Clin Sci 94:347–352
Brignole M, Menozzi C, Del Rosso A, Costa S, Gaggioli G, Bottoni N et al (2000) New classification of haemodynamics of vasovagal syncope: beyond the VASIS classification. Analysis of the pre-syncopal phase of the tilt test without and with nitroglycerin challenge. Vasovagal Syncope International Study. Europace 2:66–76
Brignole M, Alboni P, Benditt D, Bergfeldt L, Blanc JJ, Bloch Thomsen PE (2001) Task Force on Syncope, European Society of Cardiology. Guidelines on management (diagnosis and treatment) of syncope. Eur Heart J 22:1256–1306
Sudhor K, Elster MD, Jenning GI, Komesaroff PA (1997) Estrogen supplementation decreases nor-epinephrine induced vasoconstriction and total body norepinephrine spillover in perimenopausal women. Hypertension 30:1538–1543
Mercuro G, Podda A, Pitzalis L, Zoncu S, Mascia M, Melis GB et al (2000) Evidence of a role of endogenous estrogen in the modulation of autonomic nervous system. Am J Cardiol 85:787–789
Goldstein DS, Levinson P, Keiser HR (1983) Plasma and urinary catecholamines during the human ovulatory cycle. Am J Obstet 146:824–829
Nakagawa M, Ooie T, Takahashi N, Taniguchi Y, Anan F, Yonemochi H et al (2006) Influence of menstrual cycle on QT interval dynamics. Pacing Clin Electrophysiol 29:607–613
Sato N, Miyake S, Akatsu J, Kumashiro M (1995) Power spectral analysis of heart rate variability in healthy young women during the normal menstrual cycle. Psychosom Med 57:331–335
Dimitriev DA, Saperova EV, Dimitriev AD, Karpenko IuD (2007) Features of cardiovascular functioning during different phases of the menstrual cycle. Ross Fiziol Zh Im I M Sechenova 93:300–305
Moran VH, Leathard HL, Coley J (2000) Cardiovascular functioning during the menstrual cycle. Clin Physiol 20:496–504
Flevari P, Leftheriotis D, Komborozos C, Fountoulaki K, Dagres N, Theodorakis G et al (2009) Recurrent vasovagal syncope: comparison between clomipramine and nitroglycerin as drug challenges during head-up tilt testing. Eur Heart J 30:2249–2253
Mosqueda-Garcia R, Furlan R, Tank J, Fernandez-Violante R (2000) The elusive pathophysiology of neurally mediated syncope. Circulation 102:2898–2906
Grubb BP, Kosinski D, Samoil D, Pothoulakis A, Lorton M, Kip K (1995) Postpartum syncope. Pacing Clin Electrophysiol 18:1028–1031
van Dijk N, Quartieri F, Blanc JJ, Garcia-Civera R, Brignole M, Moya A, PC-Trial Investigators et al (2006) Effectiveness of physical counterpressure manoeuvres in preventing vasovagal syncope: the Physical Counterpressure Manoeuvres Trial (PC-Trial). J Am Coll Cardiol 48:1652–1657
Minson CT, Halliwill JR, Young TM, Joyner MJ (2000) Influence of the menstrual cycle on sympathetic activity, baroreflex sensitivity, and vascular transduction in young women. Circulation 101:862–868
Hirshoren N, Tzoran I, Makrienko I, Edoute Y, Plawner MM, Itskovitz-Eldor J et al (2002) Menstrual cycle effects on the neurohumoral and autonomic nervous systems regulating the cardiovascular system. J Clin Endocrinol Metab 87:1569–1575
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zyśko, D., Gajek, J., Terpiłowski, Ł. et al. Effects of the menstrual cycle phases on the tilt testing results in vasovagal patients. Arch Gynecol Obstet 286, 429–435 (2012). https://doi.org/10.1007/s00404-012-2308-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-012-2308-4