Abstract
Objective
To compare the effects of either a 5 or 7.5 mg daily dose of Letrozole in PCOS women undergoing ovulation induction and timed intercourse.
Design
Prospective randomized trial.
Setting
Academic infertility care center.
Patients
Sixty-seven PCOS patients with infertility.
Interventions
Patients were randomly divided into two groups and treated with either 5 mg/day (30 patients, group 1) or 7.5 mg/day (37 patients, group 2) Letrozole for 5 days starting from day 3 of the menstrual cycle. When the leading follicle reached 18 mm in diameter, ovulation was triggered by an injection of HCG and timed intercourse was advised thereafter.
Main outcome measures
The primary outcome measures were the number of follicles and days to reach mature follicle and the secondary endpoints were endometrial thickness, day 7 testosterone level, ovulation and pregnancy rates.
Results
The mean age, BMI, duration of infertility and basal hormone levels in both groups were similar. There was no significant difference in the endometrial thickness (7.87 ± 1.67 vs 7.16 ± 2.04), the number of intermediate (0.83 ± 0.75 vs 0.62 ± 0.76) and mature follicles (1.13 ± 1.11 vs 1.22 ± 1.03) on days 12–14 between group 1 and 2, respectively. The days to reach mature follicle were similar in both groups (12.8 ± 1.36 vs 12.6 ± 1.22). Also there was no significant difference in the day 7 testosterone level and day 21 progesterone level between the two. Ovulation occurred in 90 and 89.2% of patients in group 1 and 2, respectively without a statistically significant difference. The pregnancy rate per first ovulatory cycle was 25.8% in group 1 and 21.2% in group 2 without significant difference. No OHSS was observed in either group.
Conclusion(s)
The results of this study did not show any advantage to the use of 7.5 mg/day over 5 mg/day dose of Letrozole as the first line treatment for induction of ovulation in women with PCOS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Polycystic ovary syndrome (PCOS) is the major cause of anovulatory infertility. Clomiphene citrate (CC) is the most commonly used oral agent for ovulation induction in this group, but there are some drawbacks with the use of it. Clomiphene citrate is a selective estrogen receptor modulator with a long half life (2 weeks) and long lasting estrogen receptor (ER) depletion [1, 2]. Prolonged ER depletion may have an adverse effect on the cervical mucus and endometrium in 15–50% of patients [3, 4] causing a discrepancy between ovulation and conception rates, and higher incidence of miscarriage [5–8]. In addition, prolonged estrogen receptor down regulation can lead to multiple follicular growths and increased risk of multiple pregnancies and ovarian hyper stimulation syndrome (OHSS) which is of great concern in PCOS patients [9]. Also, clomiphene resistance occurs in 15–20% of patients and is not predictable before beginning the treatment [7].
Letrozole, a non-steroidal aromatase inhibitor, has been introduced as a new treatment option, which can challenge CC for ovulation induction in anovulatory women [10, 11]. Letrozole blocks estrogen production by inhibition of aromatization and in this way releases the hypothalamic-pituitary axis from estrogenic negative feedback. Due to its short half life (45 h) and the lack of down-regulation of estrogen receptors [12] Letrozole may have less negative effects on the endometrium and cervix in the late follicular phase [13, 14]. Because Letrozole does not deplete estrogen receptors, normal central feedback mechanisms remain intact and mono-ovulation should occur in 5 day course of treatment [13]. This is an advantage in PCOS, because theoretically it can reduce the risk of multiple pregnancy and OHSS [13, 15].
There are several reports confirming the efficacy of Letrozole superior to clomiphene [14, 16–19] or at least equal [15, 20–22] to clomiphene in ovulation and pregnancy rates.
Different doses of Letrozole ranging from 2.5 to 7.5 mg/day have been used in these studies, but there have been very few studies comparing different doses of Letrozole for ovarian stimulation in PCOS patients.
There are two studies in women with unexplained infertility [24, 32] and one in PCOS patients [23] in which increasing the Letrozole dose resulted in more mature follicles. Based on the results of these studies increasing the dose of Letrozole could increase the number of mature follicles which is of great concern in infertility treatment.
Considering the number of mature follicles and the duration of stimulation as primary outcomes, the aim of this study was to compare 5 mg/day with 7.5 mg/day Letrozole in PCOS patients.
Materials and methods
The study was conducted in the infertility clinic of a tertiary referral centre (Vali-E-asr Hospital–Tehran University of Medical Sciences) as a randomized controlled trial, between March 2009 and February 2010. The hospital research ethics board approved the study and all participants gave informed consent before inclusion in trial.
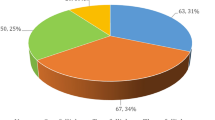
The flowchart of participants has been shown in Fig. 1. We studied 67 PCOS patients with infertility who underwent ovulation induction and timed intercourse for the first time. Polycyctic ovary syndrome was diagnosed by the Rotterdam criteria [25]. All patients were less than 35 years old with at least 1 year of infertility with no other infertility factor. Patients were randomly allocated using computer-generated random table into two Letrozole (Letrofem, Iran Hormone, Iran) treatment groups: 5 mg/day (group 1 = 30), 7.5 mg/day (group 2 = 37).
Both treatments were administered from days 3–7 of cycle. Withdrawal bleeding was achieved using 10 mg medroxy progesterone acetate tablets, for 10 days, before stimulation. Transvaginal ultrasound examinations were performed on cycle day 3 to confirm the absence of ovarian cysts before starting the treatment. All patients were monitored by transvaginal ultrasound for the mean follicular diameter and endometrial thickness between days 12–14 of the cycle. If necessary, subsequent ultrasound scans were performed until at least one follicle reached 18 mm. The mean follicular diameter was measured by taking the mean of two internal follicular diameters. The endometrial thickness was measured in the sagital plane and the maximum anteroposterior endometrial diameter was measured. The HCG injection 10,000 IU intramuscular (Pregnyl-Organon-Holland) was given when at least one follicle measured ≥ 18 mm and timed intercourse was advised every other day from the night of HCG administration for 1 week. The serum testosterone (ng/ml) concentration was measured on day 7 of the cycle (the last day of Letrozole administration) by radioimmunoassay (RIA) using direct antibody coated tube method (Immunotech-France) and serum progesterone (ng/ml) concentration was measured on day 21 of the cycle by a two-site electrochemiluminescent sandwich immunoassay system (Elecsys 2010; Roche Diagnostics GmbH-Germany).
A progesterone level ≥ 10 ng/ml was considered as ovulatory. Pregnancy was diagnosed on the basis of a β-HCG concentration greater than 10 IU/L and a positive gestational sac viewed by the ultrasound.
We evaluated the number and size of follicles and endometrial thickness on days 12–14, the number of days to reach mature follicle, day 7 testosterone level, day 21 progesterone level, ovulation and pregnancy rates. Only the first treatment cycle was included in the analysis.
Statistical analysis
Using PASS software and based on two previous studies [24, 32], a sample size of 30 subjects in each group would provide 80% power to detect a significant difference in the number of mature follicles (1.1 ± 0.0 vs 1.3 ± 0.1) and duration of stimulation (11.4 ± 0.4 vs 11.7 ± 0.4) between two groups (with a significant level of 0.05).
Data analysis was performed using SPSS version 13. Results were expressed in the form of mean ± SD and percentages. The Chi-squared test was used to compare proportions. Student’s t test and one-way analysis of variance (ANOVA) were used to compare means, as appropriate. Statistical significance was set at P < 0.05.
Results
Eighty patients were recruited of which four did not begin the cycle due to ovarian cyst and nine were lost to follow up. Figure 1 shows the flow of participants.
There were no statistically significant differences between the two groups regarding age, BMI, duration of infertility, basal hormone level and endometrial thickness on cycle day 3 (Table 1).
The ovulation induction data for the two groups is given in Table 1.
There were no significant statistical differences in the endometrial thickness (7.87 ± 1.67 vs 7.16 ± 2.04), and the number of mature follicles (1.13 ± 1.11 vs 1.22 ± 1.03) on days 12–14 between the two groups. Also there was no evidence for any significant difference between the groups regarding duration to reach a dominant follicle (12.8 ± 1.36 vs 12.6 ± 1.22), cycle day 7 serum testosterone level and cycle day 21 serum progesterone level. The ovulation and pregnancy rate per cycle were 90 and 23.3% in the 5 mg group, and 89.2 and 18.9% in the 7.5 mg group (P > 0/05) without statistically significant difference between the two. One twin pregnancy occurred in each group and there was one first trimester abortion in the 7.5 mg group. No OHSS was reported in either group.
Discussion
About 55–75% of PCOS patients have anovulatory infertility [26]. Among studies comparing Letrozole with clomiphene in PCOS patients with infertility, some have evaluated Letrozole in CC-resistant PCOS patients [16, 17, 19, 22] and the others have compared it with clomiphene as the first line treatment [14, 15, 18, 20, 21]. Considering ovulation and pregnancy rates, in all of these studies Letrozole is at least as effective as clomiphene in PCOS with additional advantages including reduced risk of multiple pregnancies and OHSS [9], absence of deleterious effect on cervical mucus and endometrial development [14] and need for less monitoring during ovarian stimulation [27]. Results from a multicentric retrospective study [28] and a randomized trial [29] did not detect any difference in malformation rates for newborns after treatment with Letrozole compared with treatment with clomiphene.
The most favorable dose of Letrozole for ovulation induction in PCOS patients has not been determined.
In this study on general PCOS patients increasing the dose of Letrozole from 5 to 7.5 mg neither increased the number of growing follicles nor decreased the duration to reach mature follicle. There was no significant difference regarding endometrial thickness, ovulation and pregnancy rates between two groups. The group taking 7.5 mg Letrozole did not have higher day 7 testosterone level, compared to 5 mg group. Although we did not check estradiol level during early to mid-follicular phase, based on similar day 7 testosterone level, we can conclude that 7.5 mg Letrozole did not decrease more intensely the estradiol level in this period, than the 5 mg Letrozole. Subsequently similar number of follicles and endometrial thickness on days 12–14, and similar duration of stimulation were shown in both groups.
One explanation to this effect is that both groups were from general PCOS patients with similar BMI and day 3 testosterone and estradiol levels.
Comparing different doses of Letrozole in clomiphene resistant PCOS patients and in those with higher BMI or androgen levels may reveal different results, which can be assessed in future studies. Another explanation for similar results in this study is that both treatments began on cycle day 3 and continued till day 7 of the cycle. Because Letrozole has a short half life and does not deplete estrogen receptors, increasing estradiol levels as the follicles grow and intact central feedback mechanisms in mid to late follicular phase result in suppression of FSH and atresia of the non-dominant growing follicles, after withholding Letrozole on day 7 of the cycle. In the study of Badawy et al. [30] comparing 2.5 mg Letrozole for 10 days with 5 mg Letrozole for 5 days, both beginning on cycle day 1 in 218 clomiphene resistant PCOS patients, the total number of follicles was significantly greater (6/7 ± 0/3 vs 3/9 ± 0/4) in the long Letrozole group. In their study extending the duration of Letrozole and not increasing the dose of it resulted in more follicles and pregnancy rates. The higher number of total follicles in short Letrozole group (5 mg/day) compared to the 5 mg/day arm of this study (3/9 ± 0/4 vs 1/97 ± 1/10) can be due to earlier beginning of treatment in their study compared to our study (cycle day 1 vs cycle day 3). The results of our previous study comparing single high dose Letrozole with multiple low dose administration in treatment of anovulatory infertility is in accordance with their findings [31]. On the other hand, there are studies in which increasing the dose of Letrozole resulted in higher number of follicles. In the study of Yang et al. [23] on 76 PCOS patients comparing 2.5 mg with 5 mg Letrozole for 5 days stating from day 3 of the cycle, the total number of mature follicles and pregnancy rate was higher in the 5 mg group. In their study there was no difference regarding days to reach mature follicle between groups. Also in the study of Al-Fadhli et al. [24] on 72 patients with unexplained infertility comparing 2.5 mg with 5 mg Letrozole, the number of mature follicles (1.1 ± 0.0 vs 1.3 ± 0.1) and pregnancy rate (5.9% vs 26.3%) was higher in 5 mg group, without significant difference in the duration to achieve a mature follicle (11.4 ± 0.4 vs 11.7 ± 0.4). Similar to the findings of Al-Fadhli et al., the study of Badawy et al. [32] on 179 patients with unexplained infertility comparing three different doses of Letrozole (2.5, 5, 7.5 mg) reported a significant dose- dependent increase in the total number of follicles with the most follicles yielded following the 7.5 mg dose (1.0 ± 0.0 vs 1.4 ± 0.1 vs 3.4 ± 0.3) (Table 2). But contrary to the studies of Yong and Al-Fadhli, in their study there was a dose-dependent decrease in the duration to reach a mature follicle with increasing doses of Letrozole (12.4 ± 0.3 vs 11.6 ± 0.5 vs 9.6 ± 0.4), and regarding pregnancy rate there was no significant difference between three groups. This discrepancy in the results between studies may be due to recruitment of different populations.
In our study increasing the Letrozole dose from 5 to 7.5 mg neither increased the number of follicles nor decreased the duration to reach mature follicle.
Compared to 75–80% ovulation rate [33] and up to 22% pregnancy rate per ovulatory cycle in PCOS women treated with clomiphene [34], in this small study overall ovulation rate and pregnancy rate per ovulatory cycle was 89/6% and 23/3% in the first cycle of treatment. Although it was not statistically significant we observed a slightly higher endometrial thickness and pregnancy rate and lower miscarriage rate in 5 mg group. This may be due to persistence of aromatase inhibition and subnormal endometrial development in 7.5 mg dose. One twin pregnancy in each arm of this study is in contrast with mono-ovulation hypothesis. Delayed clearance of the drug or relative aromatase deficiency and increased sensitivity to endogenous FSH increase after Letrozole treatment in some PCOS patients may explain this finding. Anyway the small number of pregnancies in each arm excludes any conclusion about twin pregnancy rate in this study.
The limitation of our study was that only the first treatment cycle was included in the analysis, and we did not check the patients for LUF syndrome. This is the first study which compares day 7 testosterone level in PCOS after treatment with two different doses of Letrozole.
Larger adequately powered randomized trials are needed to make a definite conclusion about the optimal dose of Letrozole in the treatment of PCOS related infertility.
In conclusion, the results of this small series suggests that compared with the daily dose of 5 mg, 7.5 mg of Letrozole offers no benefit regarding number of follicles, endometrial thickness, ovulation and pregnancy rate as a first line treatment for induction of ovulation in general PCOS patients. We suggest that extending the duration of Letrozole may result in higher number of follicles and higher doses may be beneficial in special conditions like resistance to lower doses, or higher BMI.
References
Young SL, Opsahl MS, Fritz MA (1999) Serum concentrations of enclomiphene and zuclomiphene across consecutive cycles of clomiphene citrate therapy in anovulatory infertile women. Fertil Steril 71(4):639–644
Mikkelson TJ, Kroboth PO, Cameron WJ, Dittert LW, Chungi Y, Manberg PJ (1986) Single-dose pharmacokinetics of clomiphene citrate in normal volunteers. Fertil Steril 46(3):392–396
Gonen Y, Casoer RF (1990) Sonographic determination of an adverse effect of clomiphene citrate on endometrial growth. Hum Reprod 5(6):670–674
Sereepapong W, Triratanachat S, Sampatanukul P, Pruksananonda K, Boonkasemsanti K, Reinprayoon D (2000) Effects of clomiphene citrate on the endometrium of regularly cycling women. Fertil Steril 73(2):287–291
Homburg R (2005) Clomiphene citrate—end of an era? a mini-review. Hum Reprod 20(8):2043–2051 Epub 2005 May 5
Al-Fozan H, Al-Khadouri M, Tan SL, Tulandi T (2004) A randomized trial of Letrozole versus clomiphene citrate in women undergoing superovulation. Fertil Steril 82(6):1561–1563
Franks S, Adams J, Mason H, Polson D (1985) Ovulatory disorders in women with polycystic ovary syndrome. Clin Obstet Gynecol 12(3):605–632
Kistner RW (1965) Induction of ovulation with clomiphene citrate (clomid). Obstet Gynecol Survey 20(6):873–900
Mitwally M, Biljan M, Casper R (2005) Pregnancy outcome after the use of an aromatase inhibitor for ovarian stimulation. Am J Obstet Gynecol 192(2):381–386
Mitwally M, Casper RF (2000) Aromatase inhibition: a novel method of ovulation induction in women with polycystic ovarian syndrome. Reprod Technol 10:244–247
Mitwally M, Casper R (2001) Use of aromatase inhibitor for ovulation induction in patients with an inadequate response to clomiphene citrate. Fertil Steril 75(2):305–309
Casper RF (2003) Letrozole: ovulation or superovulation? Fertil Steril 80(6):1335–1337 discussion 1339
Casper RF, Mitwally MF (2006) Review: aromatase inhibitors for ovulation induction. J Clin Endocrinol Metab 91(3):760–771 Epub 2005 Dec 29
Baruah J, Roy kk, Rahman SM, Kumar S, Sharma JB, Karmakar D (2009) Endometrial effects of Letrozole and clomiphene citrate in women with polycystic ovary syndrome using spiral artery Doppler. Arch Gynecol Obstet 279(3):311–314 Epub 2008 Jul 3
Badawy A, Aal IA, Abulatta M (2009) Clomiphene citrate or Letrozole for ovulation induction in women with polycysiic ovarian syndrome: a prospective rundomized trial. Fertil Steril 92(3):849–852
Begum MR, Ferdous J, Begum A, Quadir E (2009) Comparison of efficacy of aromatase inhibitor and clomiphene citrate in induction of ovulaltion in polycystic ovarian syndrome. Fertil Steril 92(3):853–857
Sohrabvand F, Ansari Sh, Bagheri M (2006) Efficacy of combined metformin–Letrozole in comparison with metformin–clomiphene citrate in clomiphene-resistant infertile women with polycystic ovarian disease. Hum Reprod 21(6):1432–1435
Atay V, Cam C, Muhcu M, Cam M, Karateke A (2006) Comparison of Letrozole and clomiphene citrate in women with polycystic ovaries undergoing ovarian stimulation. J Int Med Res 34(1):73–76
Ganesh A, Goswami SK, Chattopadhyay R, Chaudhury K, Chakravarty B (2009) Comparison of Letrozole with continuous gonadotropins and clomiphene-gonadotropin combination for ovulation induction in 1387 PCOS women after clomiphene citrate failure: a randomized prospective clinical trial. J Assist Reprod Genet 26(1):19–24 Epub 2009 Jan 7
Bayar U, Basaran M, Kiran S, Coskun A, Gezer S (2006) Use of an aromatase inhibitor in patients with polycystic ovary syndrome: a prospective randomized trial. Fertil Steril 86(5):1447–1451
Zeinalzadeh M, Basirat Z, Esmailpour M (2010) Efficacy of Letrozole in ovulation induction compared to that of clomiphene citrate in patients with polycystic ovarian syndrome. J Reprod Med 55(1–2):36–40
Abu Hashim H, Shokeir T, Badawy A (2010) Letrozole versus combined metformin and clomiphene citrate for ovulation induction in clomiphene-resistant women with polycystic ovary syndrome: a randomized controlled trial. Fertil Steril 94(4):1405–1409 Epub 2009 Sep 3
Yang MQ, Quan S, Li H, Song YL, Xing FQ (2008) Effect of two different doses of Letrozole in promoting ovulation in infertile women with polycystic ovarian syndrome. Nan Fang Yi Ke Da Xue Xue Bao 28(11):2060–2061
Al-Fadhli R, Sylvestre C, Buckett W, Tan SL, Tulandi T (2006) A randomized trial of superovulation with two different doses of Letrozole. Fertil Steril 85(1):161–164
The Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group, Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (2004) Fertil Steril 81(1):19–25
Guzick D (1998) Polycystic ovary syndrome.symptomatology,pathophysiology and epidemiology. Am J Obstet Gynecol 179(6 Pt 2):S89–S93
Casper RF (2009) Letrozole versus clomiphene citrate: which is better for ovulation induction? Fertil Steril 92(3):858–859 (Epub 2007 Jun 27)
Tulandi T, Martin J, Al-Fadhli R, Kabli N, Forman R, Hitkari J et al (2006) Congenital malformations among 911 newborns conceived after infertility treatment with Letrozole or clomiphene citrate. Fertil Steril 85(6):1761–1765 (Epub 2006 May 2)
Badawy A, Shokeir T, Allam AF, Abdelhady H (2009) Pregnancy outcome after ovulalion induction with aromatase inhibitors or clomiphene citrate in unexplained infertility. Acta Obstet Gynecol Scand 88(2):187–191
Badawy A, Mosbah A, Tharwat A, Eid M (2009) Extended Letrozole therapy for ovulation induction in clomiphene-resistant women with polycystic ovary syndrome: a novel protocol. Fertil Steril 92(1):236–239 (Epub 2008 Aug 15)
Ramezanzadeh F, Seifi J, Masumi M, Jafarabadi M (2007) Single dose Letrozole versus 5 day course in ovulation induction for in vivo fertilization. Hum Reprod 22(Suppl 1):IJ36
Badawy A, Mitwally M, Fawzy M (2007) Randomized controlled trial of three doses of Letrozole for ovulation induction in patients with unexplained inferlilily. Reprod Biomed Online 14(5):559–562
Messinis IE (2005) Ovulation induction: a mini review. Hum Reprod 20(10):2688–2697
Thessaloniki ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Consensus on infertility treatment related to polycystic ovary syndrome (2008). Fertil Steril 89(3):505–5022. (Epub 2008 Feb 20)
Acknowledgments
We would like to greatly thank the Deputy of Research of Tehran university of Medical Sciences and experts of Vali-E-asr infertility Research Center. Also we would like to thank Mr Mojtaba Meshkat and Mr Ehsan Sobhani who helped us during the study.
Conflict of interest
All of the authors do not have any conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ramezanzadeh, F., Nasiri, R., Sarafraz Yazdi, M. et al. A randomized trial of ovulation induction with two different doses of Letrozole in women with PCOS. Arch Gynecol Obstet 284, 1029–1034 (2011). https://doi.org/10.1007/s00404-011-1951-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-011-1951-5