Abstract
Purpose
To assess the effects of Kampo, a traditional Japanese adaptation of Chinese herbal medicine, on peri- and postmenopausal women with sleep disturbances.
Methods
Among the records of 1,523 peri- and postmenopausal women who are enrolled in the Health and Nutrition Education Program at the Tokyo Medical and Dental University, Menopause Clinic, during 1995–2009, about 151 women suffering from moderate to severe sleep disturbances were retrospectively analyzed. These women had received only health/nutrition education (control; n = 77) or received treatment with one of the three major Kampo formulae: Tokishakuyakusan (TJ-23; n = 42), Kamishoyosan (TJ-24; n = 16), or Keishibukuryogan (TJ-25; n = 16) according to their “Sho” or symptom patterns. Subjective sleep parameters, menopausal symptoms, health-related quality of life, body composition, blood pressure, and pulse rate were compared before and after the intervention.
Results
The TJ-25 group had significantly higher body weight, body mass index, body fat, lean body mass, resting energy expenditure, and relatively high blood pressure and heart rate at baseline than the other groups. After ~5-month follow up, TJ-23 reduced the sleep disruption frequency, increased lean body mass, and decreased diastolic pressure. TJ-24 alleviated subjective sleep disturbances; improved difficulties in initiating sleep, disrupted sleep, and non-restorative sleep; and relieved headache/dizziness. TJ-25 improved subjective sleep disturbances, alleviated perspiration, and reduced systolic/diastolic pressure and heart rate.
Conclusions
Each of the Kampo formulae effectively alleviated sleep disturbances in Japanese peri- and postmenopausal women. Middle-aged female patients having sleeping disorder could successfully be treated using Kampo medicines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Insomnia is defined as difficulty in the initiation and/or maintenance of sleep and/or inadequate or poor quality of sleep that results in the impairment of daytime functioning, despite adequate opportunities and circumstances for sleep [1]. The symptom, known to affect 6–30% of the general population [2], is not merely an issue of sleep disruption but is known to cause general health problems, such as obesity [3], diabetes and impaired glucose tolerance [4], hypertension [5], metabolic syndrome [6], eventually leading to increased mortality [7].
Difficulty in sleeping is also fairly common in middle-aged women, and the prevalence of the symptom is known to increase from pre- to peri-, and postmenopause [8–10]. Although the exact mechanisms underlying the increase in the prevalence of troubled sleeping with the advanced stage of menopause are not fully understood, the association of sleep disturbance with vasomotor symptoms and depressed mood, at this stage in a woman’s life, has been well-documented [11–14]. We recently reported that sleep disturbance is highly prevalent in Japanese peri- and postmenopausal women [15]. Sleep disturbance, more often coexist with mood disturbance, was shown to deteriorate their health-related quality of life (HR-QOL) significantly. Our detailed analysis revealed that hormone therapy and hypnotics are both effective treatment regimens for improving sleep disturbances in this specific population [16].
In addition to conventional medicine, complementary and alternative medicines (CAM) are widely used across the world, especially by women and middle-aged individuals, people with higher levels of education and higher incomes, and people with chronic diseases or poor overall health [17]. It was reported that in the early 2000s, CAM was used by almost 50% of the middle-aged women in Western countries to alleviate menopausal symptoms [17, 18]. The percentage might be even higher at present because of the Women’s Health Initiative (WHI) reports on the negative aspects of hormone replacement therapy [19, 20]; however, insomnia or difficulty in sleeping is not among the principal reasons for the use of CAM in this population [17].
Kampo is a Japanese subdivision of traditional East Asian medicines (TEAMs), which was founded in the sixth century and was a local adaptation of Chinese herbal medicine (CHM). It is a more pragmatic approach than CHM; in that, a medical practitioner chooses one best formula for a patient out of some 150 ready-to-use formulae that are composed of approximately 160 herbal substances corresponding to the patient’s “Sho”, i.e., a pattern of symptoms [21, 22].
The use of Kampo medicine has been revived in Japan since its approval by the Ministry of Health and Welfare in 1976, and now it is one of the main treatment options for menopausal symptoms together with hormone therapy. Among the ~150 formulae that are currently available, three of them: Tokishakuyakusan (Tangkuei and peony powder, TJ-23), Kamishoyosan (Augmented rambling powder, TJ-24), and Keishibukuryogan (Cinnamon twig and poria pill, TJ-25), have been considered to be the best fits for women with menopausal symptoms.
In this study, we compared the effects of the formulae TJ-23, TJ-24, and TJ-25 on the following: subjective sleep parameters, menopausal symptoms, HR-QOL, body composition, blood pressure, and pulse rate of peri- and postmenopausal women. Comparison was made by conducting a detailed analysis of the records of women who are enrolled in the Systematic Health and Nutrition Education Program, conducted at the Menopause Clinic of the Tokyo Medical and Dental University Hospital, during the past 15 years.
Methods
The details of the study population have been described in our previous reports [15, 16]. Briefly, we retrospectively analyzed the records of 1,523 Japanese peri- and postmenopausal women who were enrolled in the Systematic Health and Nutrition Education Program (SHNEP), conducted at the Menopause Clinic of the Tokyo Medical and Dental University Hospital, between March 1995 and December 2009. In this program, these women were examined by physicians who evaluated their health status and prescribed medicines for improving health, and by nutritionists who assessed their lifestyles and advised on appropriate diet and exercise regimens.
The mean (SD) age of the participants was 53.0 (7.2) years. Among the patients, 28.3% were classified to be in menopausal transition and 71.7% as postmenopausal based on the pattern of their menstrual cycles. A woman was defined as being in menopausal transition if she had had a menstrual period within the past 12 months, but had missed a period or had irregular cycles in the past 3 months; a woman was defined as postmenopausal if she had not had any menstrual period in the past 12 months [9, 23]. Doctors and nutritionists interviewed all the women at their initial visit and every 3 months, thereafter.
At each interview session, the women rated the severity of the following ten menopausal symptoms: hot flushes, perspiration, chilliness, irregular heartbeat, difficulty in sleeping, irritability, depressed mood, headache/dizziness, tiredness, and musculoskeletal pain. Rating was by using a 4-point scale that measured how often each symptom affected their daily life: none (never, 0 point), mild (rarely, 1 point), moderate (sometimes, 2 points), and severe (very often, 3 points). The severity of difficulty in sleeping scored in this system is referred to as “the subjective sleep disturbance score”, hereafter. Sleep quality was also assessed by the participants themselves and recorded in terms of sleep duration (h), sleep onset (easy, difficult, and neither easy nor difficult), sleep disruption (the number of awakenings per night), and sleep satisfaction (restorative, non-restorative, and neither restorative nor non-restorative) of the previous night.
The following physical characteristics were recorded: height (cm), weight (kg), body fat percentage (%), and lean body mass (kg), which were measured using a body composition analyzer MC-190EM (Tanita, Tokyo, Japan); and body mass index (BMI), which was calculated as weight (kg)/height2 (m2). Resting energy expenditure (Kcal/day) was measured using an indirect calorimeter VMB-005 N (Vine, Tokyo, Japan) as described elsewhere [24]. Further, blood pressure was measured using a sphygmomanometer BP-203 RV II (Colin, Tokyo, Japan), and pulse rate was recorded after a rest period of 5 min or more. The HR-QOL was also evaluated and scored using a self-administered, structured questionnaire developed and validated at our clinic, as described previously [15, 16]. Briefly, the questionnaire contains 38 items covering four domains of a women’s health during menopausal transition: physical health, mental health, life satisfaction, and social involvement. The participants respond to each item on a 4-point scale (strongly agree, 3; agree, 2; disagree, 1; strongly disagree, 0) or a binary scale (Yes, 1; No, 0). The QOL with respect to a domain is expressed as the total of the scores for each of the items: physical health, 9 items, 27 points; mental health, 12 items, 36 points; life satisfaction, 5 items, 15 points; and social involvement, 12 items, 16 points; the QOL is thus rated over 94 points.
Of the 1,474 participants who rated the severity of difficulty in sleeping at their first visit, 747 (50.7%) reported that their daily life was either moderately (sometimes) or severely (very often) affected by difficulty in sleeping; these women were regarded as having sleep disturbances. Of these, 151 were selected for the present study, because they received only health/nutrition education, without any medical treatment (control; n = 77) or treatment with one of the three Kampo formulae: Tsumura Tokishakuyakusan Extract Granules (TJ-23; 7.5 g/day; n = 42), Tsumura Kamishoyosan Extract Granules (TJ-24; 7.5 g/day; n = 16), or Tsumura Keishibukuryogan Extract Granules (TJ-25; 7.5 g/day; n = 16), during the follow-up period of 144 ± 58 days (mean ± SD). The composition of the three formulae is detailed in Table 1. We excluded the following subjects: (1) those who were prescribed estrogen preparations; (2) those who were prescribed hypnotics or anxiolytics; (3) those who were prescribed Kampo formulae other than TJ-23, 24, and 25; (4) those who were prescribed additional drugs, which are known to affect sleep or hormonal status, such as antidepressants, antipsychotics, anti-histamines, anticonvulsants, oral contraceptive pills, gonadotropin-releasing hormone (GnRH) agonists, tamoxifen, raloxifene, beta-blockers, or glucocorticoids.
The records of these participants were examined for the baseline characteristics and for changes in subjective sleep disturbance scores, sleep quality measures, menopausal symptom scores, HR-QOL scores, body composition, blood pressure, and pulse rate.
The Tokyo Medical and Dental University Review Board approved the study protocol, and all the participants provided informed consent.
Statistical analyses were performed by one-way analysis of variance (ANOVA) followed by Tukey’s multiple comparison test, Wilcoxon’s matched pairs test, Mann–Whitney test, Fisher’s exact test, and Kruskal–Wallis test followed by Dunn’s multiple comparison test, and paired t test, as specified. The software Prism 5 (GraphPad Software, La Jolla, CA, USA) was used for this purpose.
Results
Background
The baseline characteristics of the study subjects are shown for each group in Table 2. These women were, on average, normotensive and not obese. There was no significant difference in the age or height among the treatment groups. However, the TJ-25 group showed significantly higher body weight, body mass index, body fat, lean body mass, and resting energy expenditure than any other group. Further, the systolic pressure, diastolic pressure, and pulse rate were relatively high in the TJ-25 group although the differences were not statistically significant.
Subjective sleep disturbance score and sleep quality measures
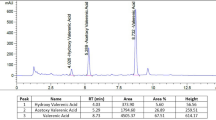
First, we compared the four treatment groups for the changes in the subjective sleep disturbance score and self-reported sleep quality measures after an interval of 5 months (144 ± 58 days, mean ± SD) (Table 3; Fig. 1). Improvement in the sleep disturbance scores after intervention was observed in every group, of which the groups TJ-24 and TJ-25 showed a significantly greater decrease (p < 0.05, Mann–Whitney test) than the control group. The self-reported sleep duration did not change with treatment in any of the four groups. The percentage of women reporting difficulty in initiating sleep (DIS) and non-restorative sleep (NRS) reduced substantially after intervention in the TJ-24 group (DIS, from 57 to 0%, p < 0.001; NRS, from 71 to 14%, p < 0.01, Fisher’s exact test), while there was a significant decrease in the frequency of disrupted sleep per night in the TJ-23 and TJ-24 groups. These findings indicate that Kampo medicine considerably improved the sleep quality in Japanese peri- and postmenopausal women with sleep disturbances, although they did not extend the sleep duration.
Percentage of women reporting a difficulty in initiating sleep (DIS) and b non-restorative sleep (NRS) in Japanese peri- and postmenopausal women with sleeping disorder, before and after intervention: open bars, before intervention; filled bars, after intervention. **p < 0.01; ***p < 0.001 versus pre-treatment, Fisher’s exact test
Menopausal symptoms
Second, the treatment groups were compared for changes in the menopausal symptom scores other than those for sleep disturbance (Table 4).
Although the post-interventional changes in these scores were minimal in all the four groups, the improvement in the score for perspiration in the TJ-25 group and that for the headache/dizziness in the TJ-24 group were significantly greater than that in the control group. That suggests that these Kampo medicines were effective in alleviating some menopausal symptoms of women with sleep disturbances.
Health-related quality of life
Third, the effects of the treatments on the HR-QOL scores of peri- and postmenopausal women with sleep disturbances were compared (Table 5). As described before [15, 16], the HR-QOL scoring system used was designed to cover four primary domains of the life of women in menopausal transition: physical health, mental health, life satisfaction, and social involvement. In the present study, the control group showed significant improvement in the domains of physical health, mental health, and life satisfaction as well as in the total HR-QOL score, indicating that SHNEP itself has the potential to enhance the HR-QOL of peri- and postmenopausal women with sleep disturbances. Similar improvement was observed in the other treatment groups except TJ-25, possibly due to the relatively high, if statistically insignificant, baseline scores of the group.
Body composition and resting energy expenditure
Since it has been reported that sleep deprivation leads to obesity [3], we next analyzed the effects of the Kampo medicines on the body composition (body weight, body mass index, body fat, and lean body mass) and resting energy expenditure of peri- and postmenopausal women with sleep disturbances (Table 6).
As described above, the women who were prescribed TJ-25 showed significantly higher body weight, body mass index, body fat, lean body mass, and resting energy expenditure than any other group at baseline before the intervention. None of the treatments induced a considerable change in the parameters, except that the TJ-23 group showed a minor increase in lean body mass; moreover, TJ-25 administration reduced the higher resting energy expenditure to a level similar to that in the other groups although the difference was statistically insignificant.
Blood pressure and pulse rate
Short-sleep and low-sleep efficiency indices have been reported as risk factors for developing hypertension [5]. Taking this into consideration, we assessed the post-interventional changes in the blood pressure and the pulse rate of the peri- and postmenopausal women with sleep disturbances (Fig. 2).
Changes in a systolic pressure, b diastolic pressure, and c pulse rate in Japanese peri- and postmenopausal women with sleep disturbance after intervention: open bars, before intervention; filled bars, after intervention. mean ± standard error. *p < 0.05; **p < 0.01; ***p < 0.001 versus pre-treatment, paired t test
As described above, the women who were prescribed TJ-25 showed higher, if not significantly different, systolic and diastolic pressure and pulse rate at baseline before intervention. The TJ-23 group showed a reduction in the diastolic pressure (76.4–72.0 mmHg), while all the parameters decreased significantly in the TJ-25 group (systolic pressure, 133.0–125.8 mmHg; diastolic pressure, 83.2–80.2 mmHg; pulse rate, 80.7–76.6 mmHg).
Discussion
Present study is a retrospective study on the effect of Kampo medicines on sleep disturbances. This study comprised of 151 Japanese peri- and postmenopausal women who participated in an education program that was conducted by a menopause clinic in Tokyo, Japan, for the past 15 years. These women received health/nutrition education with or without one of the three Kampo formulae: Tokishakuyakusan (Tangkuei and peony powder, TJ-23), Kamishoyosan (Augmented rambling powder, TJ-24), or Keishibukuryogan (Cinnamon twig and poria pill, TJ-25).
Among the ~150 Kampo formulae currently available, these three have been considered to be the most suitable for women who are suffering from climacteric symptoms and are widely used in current menopause treatments in Japan. Each formula is indicated for a specific “Sho”, or symptom pattern, as summarized in a recent extensive review of traditional East Asian medicines (TEAMs) [22]. TJ-23 is mainly used for those who are easily fatigued and have generally weak muscles with their waist and lower limbs susceptible to cold, showing suidoku (fluid retention) and deficiency patterns (chills, heavy head, edema, vertigo, etc.). TJ-24 is indicated for those who have delicate constitution and are easily fatigued and apt to have autonomic disorders as well as vasomotor symptoms (hot flushes), shoulder stiffness, various psychoneurotic symptoms including anxiety and mood disturbance. TJ-25 is indicated for those who show an oketsu (blood stagnation) pattern (hot flushes with cold legs, neck aches and stiffness) with a solid constitution, ruddy face, and pain at either side of the navel on palpation.
The participants of our study were prescribed these Kampo formulae generally according to the definition above, which was to some extent confirmed by the fact that women who took TJ-25 had significantly higher body weight, body mass index, body fat, lean body mass, and resting energy expenditure and relatively high blood pressure and heart rate.
In spite of their popularity in Japanese menopause therapy, few articles have been published in English reporting the effects of Kampo medicines on menopausal symptoms [22, 25–27], none of which specifically analyzes their effects on the sleep disturbances of peri- and postmenopausal women. In our study, all of the three formulae TJ-23, 24, and 25 were efficient in improving sleep disturbances in Japanese peri- and postmenopausal women, with each of them exhibiting slightly different treatment effects. TJ-23 reduced the frequency of sleep disruption, additionally increasing lean body mass, and decreasing diastolic blood pressure. TJ-24 effectively alleviated subjective sleep disturbances; improved difficulties in initiating sleep, disrupted sleep, and non-restorative sleep; and relieved headache and dizziness. TJ-25 improved subjective sleep disturbances, alleviated perspiration, and reduced systolic and diastolic blood pressure and heart rate.
Although the exact mechanism by which these Kampo medicines alleviate sleep disturbances is unknown, Mizowaki et al. revealed that the anxiolytic effect of Tokishakuyakusan (TJ-24) is mediated by γ-amino-butyric acid (GABA)-A receptors in a study assessing the social interaction of male mice [28]. One of the common ingredients of TJ-23 and TJ-24, Japanese Angelica Root, might be the key herb that acts through GABAA receptors to facilitate sleep [29]. On the other hand, Shinno et al. speculated that the improvement in subjective and objective sleep parameters induced in patients with dementia by another Kampo formula, Yokukansan (TJ-54), is likely to be explained by its serotonergic effect [30]. As TJ-54 shares five of its seven ingredients with TJ-24, their effects on sleep disturbance could have some mechanisms in common.
In addition to the improvement in sleep disturbances, Keishibukuryogan (TJ-25) was shown to decrease relatively high blood pressure and pulse rate to the normal level. As sleep deprivation is known to raise blood pressure and pulse rate due to elevated sympathetic tone [31], the improvement in sleep induced by TJ-25 could contribute to the reduction in blood pressure and pulse rate. The formula is also known to alleviate oketsu (blood stagnation) by improving a number of vascular and hemorheological parameters. In cholesterol-fed male rabbits, Keishibukuryogan (TJ-25) has been shown to inhibit lipid peroxide formation and to reduce the number of atheromatous plaques in the aorta [32] as well as to preserve the endothelium-dependent vascular relaxation of the aorta by inhibiting the release of superoxides from neutrophils [33]. Endothelium-dependent relaxation and hemorheological parameters were also restored by Keishibukuryogan in diabetic male rats [34]. On the other hand, Keishibukuryogan promoted red blood cell (RBC) membrane viscoelasticity by increasing intracellular ATP content, thus enhancing RBC deformability, which is supposed to contribute to the normalization of hemorheological parameters [35]. These mechanisms in combination could explain the blood pressure-lowering effect of TJ-25. More directly, one of the main ingredients of the formula, cinnamon, has been revealed to have anti-hypertensive effects in an animal experiment: in the study by Preuss et al., the herb when mixed in the diet was shown to reduce blood pressure in spontaneously hypertensive rats in a dose-dependent manner [36].
The reason why the three Kampo formulae: TJ-23, 24, and 25, used in our study, that share some of their components (Table 1) have different effects on peri- and postmenopausal women with sleep disturbances could be explained by the original concept of Kampo medicine, i.e., each mixture of herbs has synergistic effects somewhat different from those of its individual components; this has been in part verified experimentally, for example, in a murine model of cardiac transplantation [37]. In the study by Zhang et al., Saireito (TJ-114) showed its full immunosuppressive effect against the rejection of allografts only when the original formula of the herbal mixture was administered.
A limitation of our study is that the assessment of the sleep quality of the participants was based on their subjective reports on the previous nights, which may not be necessarily representative of the whole study period in some cases and may not correctly reflect objective sleep parameters. Further, its retrospective study design introduced disparity between the study groups, although the philosophy of Kampo medicine that each individual should be administered a specific mixture of herbs according to their “Sho” or symptom patterns makes a randomized study design on this topic difficult to perform.
In conclusion, each of the three major Kampo formulae, Tokishakuyakusan (TJ-23), Kamishoyosan (TJ-24), and Keishibukuryogan (TJ-25) was effective in improving sleep disturbances in Japanese peri- and postmenopausal women. Middle-aged women who suffer from difficulties in sleeping but are reluctant to take estrogens or hypnotics due to their unfavorable side effects could be successfully treated by these Kampo medicines as long as the appropriate formula is selected based on each woman’s “Sho”, or symptom patterns.
References
Silber MH (2005) Chronic insomnia. N Engl J Med 353(8):803–810. doi:10.1056/NEJMcp043762
Ohayon MM (2002) Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev 6(2):97–111
Cappuccio FP, Taggart FM, Kandala N-B, Currie A, Peile E, Stranges S, Miller MA (2008) Meta-analysis of short sleep duration and obesity in children and adults. Sleep 31(5):619–626
Gottlieb DJ, Punjabi NM, Newman AB, Resnick HE, Redline S, Baldwin CM, Nieto FJ (2005) Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med 165(8):863–867. doi:10.1001/archinte.165.8.863
Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE, Punjabi NM (2006) Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep 29(8):1009–1014
Hall MH, Muldoon MF, Jennings JR, Buysse DJ, Flory JD, Manuck SB (2008) Self-reported sleep duration is associated with the metabolic syndrome in midlife adults. Sleep 31(5):635–643
Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR (2002) Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry 59(2):131–136. doi:10.1001/archpsyc.59.2.131
Dennerstein L, Dudley EC, Hopper JL, Guthrie JR, Burger HG (2000) A prospective population-based study of menopausal symptoms. Obstet Gynecol 96(3):351–358
Kravitz HM, Ganz PA, Bromberger J, Powell LH, Sutton-Tyrrell K, Meyer PM (2003) Sleep difficulty in women at midlife: a community survey of sleep and the menopausal transition. Menopause 10(1):19–28
NIH (2005) National Institutes of Health State-of-the-Science Conference Statement: management of menopause-related symptoms. 12 Part 1 142:1003–1013
Ohayon MM (2006) Severe hot flashes are associated with chronic insomnia. Arch Intern Med 166(12):1262–1268. doi:10.1001/archinte.166.12.1262
Ensrud KE, Stone KL, Blackwell TL, Sawaya GF, Tagliaferri M, Diem SJ, Grady D (2009) Frequency and severity of hot flashes and sleep disturbance in postmenopausal women with hot flashes. Menopause 16(2):286–292
Zervas IM, Lambrinoudaki I, Spyropoulou AC, Koundi KL, Voussoura E, Tzavara C, Verdeli H, Aravantinos L, Creatsa M, Paparrigopoulos T (2009) Additive effect of depressed mood and vasomotor symptoms on postmenopausal insomnia. Menopause 16(4):837–842
Joffe H, Soares CN, Thurston RC, White DP, Cohen LS, Hall JE (2009) Depression is associated with worse objectively and subjectively measured sleep, but not more frequent awakenings, in women with vasomotor symptoms. Menopause 16(4):671–679
Terauchi M, Obayashi S, Akiyoshi M, Kato K, Matsushima E, Kubota T (2010) Insomnia in Japanese peri- and postmenopausal women. Climacteric 13(5):479–486. doi:10.3109/13697130903353478
Terauchi M, Obayashi S, Akiyoshi M, Kato K, Matsushima E, Kubota T (2010) Effects of oral estrogen and hypnotics on Japanese peri- and postmenopausal women with sleep disturbance. J Obstet Gynaecol Res doi:10.3109/13697130903353478
Brett KM, Keenan NL (2007) Complementary, alternative medicine use among midlife women for reasons including menopause in the United States: 2002. Menopause 14(2):300–307
van der Sluijs CP, Bensoussan A, Liyanage L, Shah S (2007) Women’s health during mid-life survey: the use of complementary and alternative medicine by symptomatic women transitioning through menopause in Sydney. Menopause 14(3):397–403
HI W (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the women’s health initiative randomized controlled trial. JAMA 288(3):321–333. doi:10.1001/jama.288.3.321
HI W (2004) Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the women’s health initiative randomized controlled trial. JAMA 291(14):1701–1712. doi:10.1001/jama.291.14.1701
Yu F, Takahashi T, Moriya J, Kawaura K, Yamakawa J, Kusaka K, Itoh T, Morimoto S, Yamaguchi N, Kanda A (2006) Traditional Chinese medicine and kampo: a review from the distant past for the future. J Int Med Res 34:231–239
Scheid V, Ward T, Cha W-S, Watanabe K, Liao X (2010) The treatment of menopausal symptoms by traditional East Asian medicines: review and perspectives. Maturitas 66(2):111–130
Soules MR, Sherman S, Parrott E, Rebar R, Santoro N, Utian W, Woods N (2001) Executive summary: stages of reproductive aging workshop (STRAW). Climacteric 4(4):267–272. doi:10.1080/cmt.4.4.267.272
Akiyoshi M, Owa Y, Sugiyama M, Obayashi S, Aso T (1998) An evaluation of resting energy expenditure (ree) in japanese women during perimenopausal period. J Jpn Menopause Soc 6(2):197–202
Yasui T, Yamada M, Uemura H, Ueno S-i, Numata S, Ohmori T, Tsuchiya N, Noguchi M, Yuzurihara M, Kase Y, Irahara M (2009) Changes in circulating cytokine levels in midlife women with psychological symptoms with selective serotonin reuptake inhibitor and Japanese traditional medicine. Maturitas 62(2):146–152
Yasui T, Matsui S, Yamamoto S, Uemura H, Tsuchiya N, Noguchi M, Yuzurihara M, Kase Y, Irahara M (2010) Effects of Japanese traditional medicines on circulating cytokine levels in women with hot flashes. Menopause doi:10.1097/gme.1090b1013e3181e5063c
Ushiroyama T, Ikeda A, Sakuma K, Ueki M (2005) Chai-Hu-Gui-Zhi-Gan-Jiang-Tang regulates plasma interleukin-6 and soluble interleukin-6 receptor concentrations and improves depressed mood in climacteric women with insomnia. Am J Chinese Med 33(5):703–711
Mizowaki M, Toriizuka K, Hanawa T (2001) Anxiolytic effect of Kami-Shoyo-San (TJ-24) in mice possible mediation of neurosteroid synthesis. Life Sciences 69(18):2167–2177
Matsumoto K, Kohno S-I, Qjima K, Tezuka Y, Kadota S, Watanabe H (1998) Effects of methylenechloride-soluble fraction of Japanese angelica root extract, ligustilide and butylidenephthalide, on pentobarbital sleep in group-housed and socially isolated mice. Life Sciences 62(23):2073–2082
Shinno H, Inami Y, Inagaki T, Nakamura Y, Horiguchi J (2008) Effect of Yi-Gan San on psychiatric symptoms and sleep structure at patients with behavioral and psychological symptoms of dementia. Prog Neuropsychopharmacol Biol Psychiatry 32(3):881–885
Lusardi P, Zoppi A, Preti P, Pesce RM, Piazza E, Fogari R (1999) Effects of insufficient sleep on blood pressure in hypertensive patients. Am J Hypertens 12(1):63–68
Sekiya N, Tanaka N, Itoh T, Shimada Y, Goto H, Terasawa K (1999) Keishi-bukuryo-gan prevents the progression of atherosclerosis in cholesterol-fed rabbit. Phytother Res 13(3):192–196
Sekiya N, Goto H, Tazawa K, Oida S, Shimada Y, Terasawa K (2002) Keishi-bukuryo-gan preserves the endothelium dependent relaxation of thoracic aorta in cholesterol-fed rabbit by limiting superoxide generation. Phytother Res 16(6):524–528
Goto H, Shimada Y, Sekiya N, Yang Q, Kogure T, Mantani N, Hikiami H, Shibahara N, Terasawa K (2004) Effects of Keishi-bukuryo-gan on vascular function and hemorheological factors in spontaneously diabetic (WBN/kob) rats. Phytomedicine 11(2/3):188–195
Hikiami H, Goto H, Sekiya N, Hattori N, Sakakibara I, Shimada Y, Terasawa K (2003) Comparative efficacy of Keishi-bukuryo-gan and pentoxifylline on RBC deformability in patients with “oketsu” syndrome. Phytomedicine 10:459–466
Preuss HG, Echard B, Polansky MM, Anderson R (2006) Whole cinnamon and aqueous extracts ameliorate sucrose-induced blood pressure elevations in spontaneously hypertensive rats. J Am Coll Nutr 25(2):144–150
Zhang Q, Iwami D, Aramaki O, Yakubo S, Nishimura K, Ishige A, Watanabe K, Matsuno K, Shirasugi N, Niimi M (2009) Prolonged survival of fully mismatched cardiac allografts and generation of regulatory cells by sairei-to, a japanese herbal medicine. Transplantation 87:1787–1791
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Terauchi, M., Hiramitsu, S., Akiyoshi, M. et al. Effects of three Kampo formulae: Tokishakuyakusan (TJ-23), Kamishoyosan (TJ-24), and Keishibukuryogan (TJ-25) on Japanese peri- and postmenopausal women with sleep disturbances. Arch Gynecol Obstet 284, 913–921 (2011). https://doi.org/10.1007/s00404-010-1779-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-010-1779-4