Abstract
Objective
This meta-study intends to elucidate schizophrenia–pregnancy inferences.
Methods
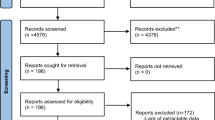
A total of 63 quasi-randomized, case–control, linkage studies on outcomes of singleton pregnancies in women with schizophrenia are identified through PubMed, ACOG, and SCOPUS. A sample of 216 pregnant and puerperal women with schizophrenia, allocated from studies of level I–IIA evidence, is compared with a sample of 487 births to unaffected women. Calculations use births as unit of analysis. Poisson regression model is used in exchangeable correlation structure.
Results
Older age (2.13), excessive smoking (1.85) and less antenatal care (1.92) in women with schizophrenia determine high risk for prematurity (2.08), including miscarriages (2.04) and preterm birth (1.98). Neonates to mothers with schizophrenia are profiled with twice likelihood of low Apgar scores (2.22), intrauterine growth retardation (2.16), and congenital defects (2.1). Poor maternal–fetal attachment and preoccupation about fetus are related to negative symptoms of schizophrenia (−0.518), length of antipsychotic treatment (−0.304) and are not associated with maternal age (0.216). Postpartum period is eventful with psychotic relapse (7.86), and parenting difficulties (11.2).
Conclusions
After adjusting for age, parity, unhealthy behaviors, length of antipsychotic treatment, and maternal–fetal attachment, maternal schizophrenia remains predictive to prematurity and postpartum psychosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Studies conducted in aftermath of deinstitutionalization suggest a significant increase in pregnancies among women with serious mental illnesses [35, 40, 50, 53]. The incidence and prevalence of perinatal poor outcomes in women with schizophrenia are being controversially reported to be higher [3, 5, 10, 14, 16, 17, 21, 41, 43, 45, 51, 60], or similar to that in general population [6, 29, 33, 56 ]. The modifying impact of excessive smoking [11, 19, 54 ], older age [ 47, 55], unplanned pregnancy [36, 54], low parity [30, 52], exposure to antipsychotics [4, 18, 56], delayed recognition of pregnancy and labor signs [6, 7, 34–36], poor attachment to fetus [2, 9, 22, 27, 30, 45, 49], less prenatal care [5, 6, 25, 51], associative medical conditions [47], and the extent to which pregnancy outcomes are intrinsically related to schizophrenia [59, 62, 63] remain as major themes of debates.
Several studies suggest that schizophrenia and schizoaffective disorders are independent risk factors for congenital malformations [16, 18, 21, 59]. Women with schizophrenia have more unwanted pregnancies, less prenatal care, and reduced likelihood of having a partner or spouse. These are significant disadvantages that compound the risks for mother and child in addition to the direct impact of schizophrenia [12, 39, 57]. Women with prominent negative symptoms and chronic course of schizophrenia have significantly higher rates of obstetrical complications and lower Apgar scores (0–3) than women with prominent positive symptoms [25]. Newborns to mothers with schizophrenia show significantly reduced arousal—associated with neurological abnormality and deviant sensitivity to stimulation, but not with obstetric complications [47, 48]. Children of women with schizophrenia have higher rates of sudden infant death syndrome (SIDS) [23, 26]. Mothers with schizophrenia and their infants are more likely to have poorer interactions (sensitivity and responsiveness) than mothers with affective disorders and their infants [28, 33].
Other studies suggest that schizophrenia–pregnancy inferences are determined mainly by unhealthy behaviors (smoking, poor diet, less care and connection to fetus) [11]. Pregnant women with schizophrenia are at lower risk of preeclampsia. There are no other differences in the incidence of specific complications, such as placenta previa, placental abruption, and abnormal fetal presentation. There is no significant difference between pregnancy outcomes in women who give birth before and after the onset of schizophrenia. Nevertheless, women with schizophrenia are at an increased risk of in-partum interventions: C-section, vaginal-assisted delivery, amniotomy, and pharmacological induction or augmentation of labor [6, 24].
Postpartum is a time of increased risk for exacerbation of schizophrenia. Negative symptoms of schizophrenia, such as apathy or difficulty expressing emotions, may contribute to under stimulation or neglect of the child, and high rates of custody loss [36, 54]. The absence of formal DSM-IV diagnostic criteria for postpartum psychosis promotes disparate treatment under the law [49]. There are limited data on the use of widely prescribed second generation antipsychotics in pregnant and breastfeeding women with mental disorders. For ethical reasons, research on these subjects mostly relies on collection of single datasets of cases to establish treatment guidelines [27]. Several studies support the use of atypical psychotropics, such as, olanzapine or risperidone, during breast feeding [2, 4, 13, 15, 20]. Authors recommend that the decision to breast feed be made after individual risk–benefit analysis that includes recording severity and frequency of symptoms of maternal mental illness, level of family support, woman’s general cooperation with treatment, ability to closely monitor the newborn, understand early warning signs of exposure to antipsychotics in breastfed newborn, and supply the health staff with timely and reliable informants.
Current research on maternal–infant health is replete with discussions on attachment and bonding. Maternal–fetal attachment (MFA) or the “umbilical affect” is about psychosocial commitment of a pregnant woman to her fetus, and the response of the fetus to this commitment [33]. Biologically, the MFA is explained by neuroendocrine interactions and exchanges of catecholamines, including epinephrine, norepinephrine and dopamine [1, 8, 28, 31, 37, 38, 61]. MFA is manifested in behaviors that demonstrate care and commitment to the fetus and include nurture (eating well, abstaining from illicit substances), comforting (stroking the belly), and physical preparation (buying baby clothes and equipment) [7, 32]. The frequency and intensity of MFA behaviors increase with advancing gestational age, particularly after the onset of fetal movements at 18–22 gestational weeks [28, 38]. MFA is consistently related to pregnancy planning, strength of marital relationship, social support, gestational age, and maternal depression and anxiety [45, 46]. From a clinical perspective, approximately 8% of women develop minimal attachment to fetus [44].
Maternal–fetal attachment scale (MFAS) was developed by Cranley [8] and is equipped to quantify 24 items of the following five subscales: role taking, differentiation of self from fetus, interaction with fetus, attributing features to the fetus (fetal image, or physical and kinesthetic awareness of fetus), and giving of self. Condon [7] suggests a 19-item scale of two underlying dimensions: affective experiences (closeness/distance, tenderness/irritation, pleasure in interaction, distress at fantasized loss, conceptualization of the fetus as a ‘person’) and intensity of preoccupation (amount of time spent thinking about fetus, talking and palpating fetus).
Given the scant discussions on maternal–fetal conflicts (MFC) in the existing obstetrical knowledge, this review classifies the following MFC for their further use as mediators of perinatal adverse outcomes: (1) behavioral/cultural (vegetarian or reduced diet, smoking, informed assent for treatment or termination of pregnancy) [3, 10, 12, 56] (2) psychosocial (serious mental illness, illicit drug use, alcoholism) [7, 28, 35, 38, 57], (3) environmental (informed or uninformed exposure to environmental hazards, such as vibration, chemicals, heavy metals, and bio-hazards), (4) obstetrical (placental defects, such as preeclampsia, uterine fibroids and septum; abnormal placentation—mostly cervical), (5) medical (preexisting diseases [diabetes mellitus, hypertension, thyroid dysfunction, cancer, lupus], vertically transmitted infections [cytomegalovirus, HIV, chlamydia trachomatis, hepatitis C, herpes simplex, active toxoplasmosis, rubella]), (6) biological (Rhesus and LHA conflicts), (7) iatrogenic (diagnostic errors and malpractice) [42, 52], (8) paternal (unwanted pregnancy, financial instability, older age, poor relationships and poor attachment) [58] (9) legal—conflict between legal infrastructures (Supreme Court and State Laws) [14, 24], (10) bioethical (conflicts between Committee Statements, like American Academy of Pediatrics, American College of Obstetricians and Gynecologists) [42].
Sample
Of the 85 retrieved papers, only 63 studies on presentation of schizophrenia in pregnancy and postpartum are eligible according to specific inclusion criteria: singleton pregnancies, and reported statistical power (0.05 maximum alpha level, 95% CI, maximum type II error of 0.80). A sample of 216 pregnant and puerperal women with schizophrenia is selected for exploratory data from studies of levels I–IIA evidence. A sample of 487 births to women without mental illnesses is used for control.
Methods
Studies published between 1977 and 2010 are identified through PubMed, ACOG, PsycINFO and SCOPUS. Results from different reports are combined to produce a pooled odds ratio according to the Mantel–Haenszel method, using both fixed, and random effects models. Pooled estimates of candidate factors, and outcomes from a sample of 216 pregnant and puerperal women with schizophrenia are compared with a sample of 487 births to women without mental illnesses—randomly selected from obstetrical data identified with the help of the same Mesh terms. Maternal–fetal attachment subscales are modeled as process variables to explain factor–outcome relationships.
Factors
A variety of personal, clinical, and behavioral variables are considered in a model to predict perinatal outcomes. Personal characteristics include maternal age, parity, and marital status. Clinical features include gestational age, onset of schizophrenia, its course, antipsychotic treatment, vertical infections, fetal distress, preeclampsia, and intrauterine growth retardation (IUGR). Behavioral factors, include smoking, diet, illicit drug use, number of antenatal visits, and the means of maternal–fetal attachment sub-scales: affective experiences (closeness, tenderness, pleasure in interaction, distress at fantasized loss, conceptualization of fetus as a ‘person’) and intensity of preoccupation (amount of time spent palpating, interacting with fetus).
Measurable outcomes
Frequencies of binary variables (prevalence and incidence of miscarriages, stillbirth, preeclampsia, abnormal fetal presentation, oligohydramnios, placental abruption and presentation, augmented labor, C-section, obstetrical forceps, small for gestational age newborns, birth defects, sudden infant death syndrome, postpartum psychosis and parenting difficulties) are modeled as outcomes, and odds of numerical variables (Apgar scores, weight/height of the newborn and duration of postpartum psychosis) are used as linear functions exposed to factors.
Data analysis
Calculations use births as unit of analysis. One-way analysis of variance (ANOVA) is used for continuous data; Kruskal–Wallis ANOVA is used for ranked ordinal data; and chi-squared (χ2) is used where data are categorical. Descriptive statistics are used to profile characteristics of samples. For binary variables, relative risk (RR) and its 95% confidence interval (CI) are computed on an intention-to-treat basis. Continuous data are presented by weighted mean difference statistic, with a 95% CI. For each variable, frequency tables are obtained and distributions examined for the presence of outliers, and missing data. Crude odds ratios with 95% CI not containing unity are followed up by adjusting the OR for maternal age, parity, onset of schizophrenia, and length of antipsychotic treatment. For multivariate models for scored outcomes, generalized estimating equations are used with an exchangeable correlation structure into which a Poisson regression is fitted. Data are analyzed with Epi-Info (version 3.5.1), and ASSISTAT (version 7.5β) programs.
Results
Table 1 profiles the samples. The absent data are marked as missing values (mv): as can be seen in Table 1, mothers with schizophrenia are older (RR 2.13, 95% CI 1.41–2.86), have shorter relationships with partners (OR 0.86, 95% CI 0.64–1.17), are twice likely to smoke (RR 1.85, 95% CI 1.02–2.67), lack in antenatal vitamin intake (RR 1.92, 95% CI), and have higher odds for definite obstetrical complications (RR 2.08, 95% CI 1.04–6.14), including miscarriages (RR 2.04, 95% CI 0.88–1.28), and preterm labor (RR 1.98, 95% CI 0.19–2.79). Newborns to mothers with schizophrenia are profiled with lower Apgar scores (RR 2.22, 95% CI 0.56–8.84), are at twice increased risk for growth retardation (RR 2.16, 95% CI 1.48–3.87), and congenital defects (RR 2.1, 95% CI 1.1–3.8). Postpartum period in women with schizophrenia is characterized with high risk for psychotic relapse (RR 7.86, 95% CI 2.1–17.8), and parenting difficulties (RR 11.2, 95% CI 4.48–23.6). Schizophrenia group is profiled with lower risk for preeclampsia, fetal malposition, and placenta previa (RR 0.81, 0.67, and 0.78, correspondingly). When compared with unaffected mothers, no significant differences are noted regarding stillbirth, precipitate delivery, augmented labor, and non-elective C-section (RR 1.1, 1.22, 1.08, and 0.95, correspondingly). No data are found on mother-to-child transmitted infections, oligohydramnios, and applications of obstetrical forceps in women with schizophrenia.
Maternal–fetal attachment (MFA) in women with schizophrenia confers lower quality and preoccupation scores (OR 0.78, and 0.45, respectively). Weak negative associations are found between quality of attachment to fetus and length of antipsychotic treatment (r 2 = −0.304), as well as with years in partner relationships (r 2 = −0.298). Substantial negative associations are found between preoccupation about fetus and negative syndrome-scale (r 2 = −0.518). No associations are found between the age of women and quality of attachment, and preoccupation about fetus (r 2 = 0.216 and r 2 = 0.289, correspondingly).
Figure 1 illustrates citatometric weight of pooled perinatal outcomes and their determinants in reviewed sample:
It is shown that studies are focused on more descriptions of perinatal risk factors to women with schizophrenia rather than outcomes. Smoking, unintended pregnancy, exposure to antipsychotics, poor maternal–fetal attachment, poor fetal image remain the major themes. Preterm labor, non-elective C-section, small for gestational age (SGA) newborns, low Apgar scores, and postpartum psychosis are the mostly reported outcomes. No data are identified on mother-to-child transmitted infections, oligohydramnios, and applications of obstetrical forceps in women with schizophrenia.
Discussion
In line with previous studies [16, 19, 21, 23, 39, 47, 48, 59, 63], our findings suggest that older age (14.8%, RR 2.13), smoking (29.6%, RR 1.85), and less antenatal vitamin intake (28.2%,RR 1.92) relate to perinatal risk in schizophrenia. Women with schizophrenia confer higher rates of cumulative obstetrical complications (45.8%, RR 2.08), including miscarriages (5.1%, RR 2.04), and preterm labor (5.1%, RR 1.98). The most salient findings in neonates to mothers with schizophrenia are lower 5-min Apgar scores (6.5%, RR 2.22), intrauterine growth retardation (7.4%, RR 2.16), and congenital defects (5.09%, RR 2.1), including holoprosencephaly, microcephaly, spina bifida, and chromosomal syndromes (RR 2.1). Similar findings are reported by Hizkiyahu [16], Nilsson [39], Schneid-Kofmanan [47], Jablensky [21], and others. Postpartum in schizophrenics is specified with high rates of psychotic relapse (37.5%, RR 7.86), and parenting difficulties (31 %, RR 11.2). Consistent with other studies [6, 11], our findings suggest that women with schizophrenia have lower rates of preeclampsia (5.5%, RR 0.81), fetal malposition (2.3%, RR 0.67), and placenta previa (0.9%, RR 0.78). When compared with unaffected mothers, no significant differences are noted regarding stillbirth, precipitate and augmented labor, non-elective C-section, and SIDS.
In line with existing data [25, 33, 43], we found that the quality of maternal–fetal attachment and preoccupation with fetus were not associated with age of women, but were substantially related to the exposure to antipsychotics (r 2 = −0.304), marital relationships (r 2 = −0.298), and negative symptoms of schizophrenia (r 2 = −0.518).
Smoking, exposure to antipsychotics, unintended pregnancies, poor maternal–fetal attachment, poor fetal image were the most discussed themes in studies on maternal schizophrenia. Preterm labor, non-elective C-section, SGA newborns, low Apgar scores, and postpartum psychosis were the mostly met outcomes in studies related to maternal schizophrenia. There were no discussions on vertically transmitted infections, oligohydramnios, and assisted labor with obstetrical forceps in women with schizophrenia in the reviewed literature.
Limitations and strength
Owing to its design, this study enables omit variables: for example, intrauterine growth retardation could be both, cause and consequence of psychotic relapse in pregnancy. Next, a possibility of type II error may exist in studies that do not suggest increased perinatal risks and adverse outcomes. The strength of this study is first in its multi-dimensional assessments. Secondly, it classifies and prioritizes maternal–fetal conflicts.
Conclusions
Findings of this study inform the following key messages for antenatal care of women with schizophrenia: (1) maternal schizophrenia is not intrinsically predictive for preeclampsia, stillbirth, placenta previa, fetal malposition, augmented labor, non-elective C-section and sudden infant syndrome, (2) older age, less parity, shorter marital relationships, excessive smoking, poor antenatal care are significant disadvantages that compound the risks for mother and child, and determine increased cumulative rate of obstetrical complications (45.8%) in this population, (3) given the complexity of direct and indirect factors affecting pregnancy outcomes in women with schizophrenia, the maternal–fetal attachment scale is helpful in monitoring and measuring indirect perinatal risk factors, and preventing related adverse outcomes. (4) After adjusting for potential confounders women with schizophrenia remain at higher risks for miscarriages (5.1%), preterm birth (5.1%), having newborns with twice lower Apgar scores (6.5%), intrauterine growth retardation (7.4%), and congenital defects (5.09%).
Implications for research
Attesting to the complex and diverse nature of maternal schizophrenia are wide variations in such relevant factors as these: premorbid personality patterns of the patients, their breastfeeding history, onset of illness, types of precipitants which presumably actuate the disease, racial/cultural specifics, level of patient–provider communication, social support, among others. The role of parity, maternal–fetal attachment, maternal–fetal conflicts and their association with negative symptoms of schizophrenia, hold promise for facilitating further research.
References
Ahern N, Ruland JP (2003) Maternal–fetal attachment. J Perinat Educ 12(4):27–35
Aichhorn W, Stuppaeck C, Whitworth AB (2005) Risperidone and breast-feeding. J Psychopharmacol 19:211–213
Alhusen JL (2008) A literature update on maternal–fetal attachment. J Obstet Gynecol Neonat Nurs 37(3):315–328
Altshuler LL, Cohen L, Szuba MP et al (1996) Pharmacological management of psychiatric illness during pregnancy: dilemmas and guidelines. Am J Psychiatry 153:592–606
Bennedsen BE, Mortensen PB, Olesen AV et al (1999) Preterm birth and intra-uterine growth retardation among children of women with schizophrenia. Br J Psychiatry 175:239–245
Bennedsen BE, Mortensen PB, Olesen AV et al (2001) Obstetric complications in women with schizophrenia. Schizophr Res 47(203):167–175
Condon JT (1993) The assessment of antenatal emotional attachment: development of a questionnaire instrument. Br J Med Psychol 66(pt 2):167–183
Cranley MS (1981) Development of a tool for the measurement of maternal attachment during pregnancy. Nurs Res 30:281–284
Dev V, Krupp P (1995) Adverse event profile and safety of clozapine. Rev Contemp Pharmacother 6:197–208
Dudzinski DM, Sullivan M (2004) When agreeing with the patient is not enough: a schizophrenic woman requests pregnancy termination. Law Ethics Psychiatry
Ellman LN, Huttenen M, Lönnqvist J et al (2007) The effects of genetic liability for schizophrenia and maternal smoking during pregnancy on obstetrical complications. Schizophr Res 93(1–3):229–236
Field MA (1989) Controlling the woman to protect the fetus. Law Med Health Care 17(2):114–129
Gardiner SJ, Kristensen JH, Begg EJ et al (2003) Transfer of olanzapine into breast milk, calculation of infant drug dose, and effect on breast-fed infants. Am J Psychiatry 160:1428–1431
Hendrick V (2006) Psychiatric disorders in pregnancy and the postpartum: principles and treatment. (Current Clinical Practice Series) Hardcover, Humana Press
Hill RC, McIvor RJ, Wojnar-Horton RE et al (2000) Risperidone distribution and excretion into human milk: case report and estimated infant exposure during breast-feeding. J Clin Psychopharmacol 20:285–286
Hizkiyahu R, Levy A, Sheiner E (2009) Pregnancy outcome of patients with schizophrenia. Am J Perinatol 27(1):19–23
Howard LM, Kumar R, Thornicroft G (2001) Psychosocial characteristics and needs of mothers with psychotic disorders. Br J Psychiatry 178:427–432
Howard LM (2005) Fertility and pregnancy in women with psychotic disorders. Eur J Obstetrics Gynecology Reprod Biol 119:3–10
Hultman CM, Cnattingius S, Olausson PO et al (2008) Schizophrenia and offspring’s risk for adverse pregnancy outcomes and infant death. Br J Psychiatry 193:311–315
Ilett KF, Hackett LP, Kristensen JH et al (2004) Transfer of risperidone and 9-hydroxyrisperidone into human milk. Ann Pharmacother 38:273–276
Jablensky AV, Morgan V, Soc MS et al (2005) Pregnancy, delivery, and neonatal complications in a population cohort of women with schizophrenia and major affective disorders. Am J Psychiatry 162:79–91
Jeffries JJ, Plummer E, Thornton JF, Seeman MV (1999) Living and working with schizophrenia, 2nd edn, Hardcover
King-Hele SA, Abel KM, Webb RT et al (2007) Risk of sudden infant death syndrome with parental mental illness. Arch Gen Psychiatry 64(11):1323–1330
Kolder VE, Gallagher J (1987) Court-ordered obstetrical interventions. N Engl J Med 316(19):1192–1196
Kotlicka AM, Gmitrowitcz A, Sobow TM et al (2001) Obstetrical complications and Apgar score in early-onset schizophrenic patients with prominent positive and prominent negative symptoms. J Psychiatr Res 35(4):249–257
Lee HC, Lin HC (2009) Maternal bipolar disorder increased low birth weight and preterm births: a nationwide population-based study. J Affect Disord 121(1–2):100–105
Lee A, Giesbrecht E, Dunn E et al (2004) Excretion of quetiapine in breast milk. Am J Psychiatry 161:1715–1716
Lerum CW, LoBiondo-Wood G (1989) The relationship of maternal age, quickening, and physical symptoms of pregnancy to the development of maternal–fetal attachment. Birth 16:13–17
Lin HC, Chen IJ, Chen YH et al (2010) Maternal schizophrenia and pregnancy outcome: does the use of antipsychotics make a difference? Schizophr Res 116(1):55–60
Lindgren K (2001) Relationships among maternal-fetal attachment, prenatal depression, and health practices in pregnancy. Res Nurs Health 24(3):203–217
Maret SM (1989) Frank Lake’s maternal–fetal distress syndrome:—an analysis, Chap. 3, Caldwell University, Caldwell
Maskenzie TB, Nagel TC (1986) When a pregnant woman endangers her fetus. Hastings Center Report 16(1):24–25
McIntosh AM, Homes S, Gleeson S et al (2002) Maternal recall bias, obstetric history and schizophrenia. Br J Psychiatry 181:520–525
Miller LJ, Shah A (1999) Major mental illness during pregnancy. Primary Care Update for OB/GYNS 6(5, 10):163–168
Miller LJ (2007) Comprehensive care of pregnant mentally ill women. J Behav Health Serv Res
Miller LJ (1997) Sexuality, reproduction, and family planning in women with schizophrenia. Schizophr Bull 23(4):623–635
McK. Doan H, Cox NL et al (2003) The maternal fetal attachment scale: some methodological pondering. J Prenat Perinat Psychol Health 18(2):167–188
Muller ME (1993) Development of the prenatal attachment inventory. Western J Nurs Res 15:199–215
Nilsson E, Lichtenstein P, Cnattingius S et al (2002) Women with schizophrenia: pregnancy outcome and infant death among their offspring. Schizophr Res 58:221–229
Ogle A, Mazzullo L (2002) Before your pregnancy: a 90 day guide for couples on how to prepare for a healthy conception, Hardcover
Ostler T (2009) Mental illness in peripartum period. Zero to Three 29(5)
Pinkerton JV, Finerty JJ (1996) Resolving the clinical and ethical dilemmas involved in fetal–maternal conflicts. Am J Obstet Gynecol 175(2):289–295
Preti A, Cardascia L, Zen T et al (2000) Risk for obstetric complications and schizophrenia. Psychiatry Res 96(2):127–139
Righetti PL, Dell’Avanzo M, Grigio M et al (2005) Maternal/paternal antenatal attachment and fourth-dimensional ultrasound technique: a preliminary report. Br J Psychol 96(Pt 1):129–137
Riley D (1995) Perinatal mental health, Hardcover. Radcliffe Medical Press, Oxford
Salisbury A, Law K, LaGasse L et al (2003) Maternal–fetal attachment. JAMA 289:1701
Schneid-Kofman N, Sheiner E, Levy A (2008) Psychiatric illness and adverse pregnancy outcome. Int J Gynecol Obstet 101(1):53–56
Schubert EW, Blennow G, McNeil TF (1996) Wakefulness and arousal in neonates born to women with schizophrenia: diminished arousal and its association with neurological deviations. Schizophr Res 22(1):49–59
Spinelli MG (2004) Maternal infanticide associated with mental illness: prevention and the promise of saved lives. Am J Psychiatry 161:1548–1557
Susser ES, Gorman JM, Brown AS (1999) Prenatal exposures in schizophrenia, vol 56, Hardcover, American Psychiatric Publishing
Tsai-Ching L, Chin-Shyan C, Chung Ping AL (2009) Do children of parents with mental illness have lower survival rate? A population-based study. Comprehensive psychiatry (in press)
Van Bogaert LJ (2006) Rights of and duties to non-consenting patients—informed refusal in the developing world. Develop World Bioethics 6(1):13–22
Wan MW, Moulton S, Abel KM (2008) A review of mother–child relational interventions and their usefulness for mothers with schizophrenia. Arch Womens Mental Health 11(3):171–179
Yaeger D, Smith HG, Altshuler LL (2006) Atypical antipsychotics in the treatment of schizophrenia during pregnancy and the postpartum. Am J Psychiatry 163:2064–2070
Yarcheski A, Mahon NE, Yarcheski TJ et al (2009) A meta-analytic study of predictors of maternal-fetal attachment. Int J Nurs Studies 46(5):708–715
Yaris F, Yaris E, Kadioglu M et al (2004) Use of polypharmacotherapy in pregnancy: a prospective outcome in a case. Prog Neuropsychopharmacol Biol Psychiatry 28(3):603–605
Yun Y, Phillips LJ, Cotton S et al (2005) Obstetric complications and transition to psychosis in an ‘ultra’ high risk sample. Aust N Zealand J Psychiatry 39(6):460–466
Zammit S, Allebeck P, Dalman C et al (2003) Paternal age and risk for schizophrenia. Br J Psychiatry 183:405–408
Zammit S, Lewis S, Gunnell D (2007) Schizophrenia and neural tube defects: comparisons from an epidemiological perspective. Schizophr Bull 33(4):853–858
Zax M, Sameroff AJ, Babijian HM (1977) Birth outcomes in the offspring of mentally disordered women. Am J Orthopsychiatry 47(2):218–230
Zimerman A, Doan H, McK (2003) Prenatal attachment and other feelings and thoughts during pregnancy in three groups of pregnant women. J Prenatal Perinatal Psychol Health 18(2):131–148
Zipursky RB, Schulz SC (1987) Seasonality of birth and CT findings in schizophrenia. Biol Psychiatry 22(10):1288–1292
Zornberg GL, Buka SL, Tsuang MT (2000) The problem of obstetrical complications and schizophrenia. Schizophr Bull 26(2):249–256
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Matevosyan, N.R. Pregnancy and postpartum specifics in women with schizophrenia: a meta-study. Arch Gynecol Obstet 283, 141–147 (2011). https://doi.org/10.1007/s00404-010-1706-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-010-1706-8