Abstract
Purpose
The purpose of this study is to examine whether cesarean section in the first pregnancy is associated with the success or failure of programmed fetal growth phenotypes or patterns in the subsequent pregnancy.
Methods
We analyzed data from a population-based retrospective cohort of singleton deliveries that occurred in the state of Missouri from 1978 to 2005 (n = 1,224,133). The main outcome was neonatal mortality, which was used as an index of the success of fetal programming. Cox proportional hazard and logistic regression models were used to generate point estimates and 95% confidence intervals.
Results
Mothers delivering by cesarean section in the first pregnancy were less likely to deliver subsequent appropriate-for-gestational-age (AGA) neonates (OR 0.91, 95% CI 0.89–0.92) when compared with mothers delivering vaginally. Of the 1,457 neonatal deaths in the second pregnancy, 383 early neonatal and 95 late neonatal deaths were to mothers with cesarean section deliveries in the first pregnancy. When compared with women with a previous vaginal delivery, AGA neonates of women with a primary cesarean section had 20% increased risk of both neonatal (OR 1.20, 95% CI 1.05–1.37) and early neonatal (OR 1.23, 95% CI 1.05–1.43) death.
Conclusion
Our study suggests that previous cesarean section is a risk factor for neonatal mortality among AGA infants of subsequent pregnancy. Future prospective studies are needed to confirm these findings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cesarean section (C-section) deliveries account for a significant portion of all births in the United States. Vital statistics records have chronicled a steadily increasing frequency between 1996 and 2007 [1] and cesarean sections now account for almost one-third (31.8% in 2007) of all deliveries in the United States [1]. Certain maternal risk factors have been shown to be significantly associated with an increased risk of cesarean section deliveries; included are advanced maternal age, higher body mass index (BMI), Black race, and other maternal obstetric or medical characteristics (e.g., preeclampsia, diabetes mellitus, etc.) [2–5]. However, even in the absence of maternal risk factors, the increase in primary cesarean sections, physician preferences, and an increase in elective, non-emergency cesarean sections are all associated with the elevated frequency of cesarean deliveries [6–8].
Although cesarean section is invaluable in emergency situations, it is well recognized that there are certain inherent risks for maternal and infant morbidity and mortality. Previous studies have shown that even in the absence of medical risk factors, there may be an increased risk of stillbirth and infant mortality, among both mothers with primary or first time, cesarean section and those with a history of cesarean delivery [7, 9, 10]. Towner et al. [11] demonstrated that neurological injuries, hemorrhage, convulsions, and feeding difficulties were significantly higher among infants delivered by cesarean section as compared to those delivered vaginally. In a previous study, we evaluated the Missouri births between 1978 and 1997 for the association between cesarean sections in the first pregnancies and stillbirth in subsequent pregnancies [12]. Although in that study, we did not find an overall increased risk among mothers with a history of cesarean section, there was a 40% increased risk of stillbirth among Black mothers when compared with White mothers (stillbirth rate 9.3 vs. 6.8 per 1,000 births; OR 1.4, 95% CI 1.1–1.7) [12].
With the current trends in cesarean section delivery rates and the observed increase in morbidity and mortality in concurrent and subsequent pregnancies, it becomes increasingly important to perform more focused evaluation on other likely effects of cesarean section delivery on subsequent pregnancy outcomes. Accordingly, we undertook this study with the aim of examining whether cesarean section in the first pregnancy is associated with the success or failure of programmed fetal growth phenotypes or patterns in the subsequent pregnancy. We categorized fetal intrauterine growth phenotypes as small-for-gestational age (SGA), appropriate-for-gestational age (AGA), and large-for-gestational age (LGA), as was used in our previous study [12]. Using these patterns, we analyzed the success of fetal programming for each growth phenotype, defined as survival beyond the first 28 days of life, between mothers with prior vaginal versus cesarean section births. We hypothesize that a history of prior cesarean section delivery will directly influence the success of fetal programming in the subsequent pregnancy. We have formulated this hypothesis-based preliminary findings from our earlier research [12], as well as reports from the previously published literature.
Materials and methods
Data source
This analysis was conducted using the maternally linked cohort data from the Missouri database. The database has proven to be highly reliable and valid, and is often considered a gold standard in the validation of other data sets using linkage procedures [12, 13]. Data used in this analysis included the full Missouri database, covering the 27-year period from 1978 to 2005. In this data file, unique identifiers were used to longitudinally link maternal health information to subsequent fetal and infant birth and death records. The specific methods and algorithm used in linking maternal obstetric and infant health data have been previously detailed [14].
Variables
This is a retrospective cohort study on women delivering two consecutive, singleton live births, with gestational ages between 20 and 44 weeks (n = 450,141) for both pregnancies. Because the exposure of interest was receipt of cesarean delivery in the first pregnancy, mothers in the first pregnancy were categorized based on the mode of delivery: vaginal or cesarean section groups. Cesarean section classification included those with coding for primary elective and primary emergency on birth records. Eligible women were then followed over time to their second pregnancy to assess the outcome of interest, which were intrauterine fetal programming patterns (or fetal growth phenotypes) and their success.
Fetal growth phenotype categories were created from the infants’ gestational ages and birth weights using population-based growth curves. Each category was defined as follows: SGA (less than 10th percentile of birth weights), LGA (greater than 90th percentile of birth weights), and AGA (10–90th percentile of birth weights) [15]. Infant gestational ages were used to create the following categories: term (at least 37 weeks), very preterm (32 weeks or less), and moderately preterm (33–36 weeks). Gestational ages were estimated based on the interval between the date of the last menstrual period (DLM) and the date of delivery of the neonate. In instances of discrepancy between the estimate and the infant’s birth weight (e.g., a term neonate having very low birth weight), the clinical estimate given on the vital records was used [16]. Previous studies have validated the use of the reported gestational age on the US birth certificates [17, 18]. The Tennessee Birth Record Study by Piper et al. [17] reported an overall agreement of 84.2% with medical records. Infant birth weights were used in the following categories: low birth weight (LBW <2,500 g), normal birth weight (NBW 2,500–3,999 g), and high birth weight (HBW ≥4,000 g).
As we have previously justified and published [19, 20], we used neonatal mortality as an index of the success of fetal programming. Neonatal mortality is defined as the death of the newborn before 28 days of life. We further delineated neonatal death into early (infant death from 0–7 days of life) and late (infant death from 7 to 27 days). Neonatal death, as opposed to infant mortality, was chosen as our outcome because of its close relation to pregnancy-associated events. To evaluate the risk of neonatal mortality, we divided infants into categories based on the mothers’ method of delivery in the first pregnancy and the neonates’ intrauterine growth phenotype and gestational ages. They were vaginal or c-section: SGA-term, SGA–moderately preterm, SGA-very preterm, AGA-term, AGA-moderately preterm, AGA-very preterm, LGA-term, LGA-moderately preterm, and LGA-very preterm. In this case, for example, an infant who was born to a woman who delivered via c-section in her first pregnancy and was born small-for-gestational age between 33 and 36 weeks gestation would be placed in the c-section-SGA-moderately preterm category. Infants who belonged to the primary vaginally delivered group were set as the referent category, which means, within each intrauterine growth group (SGA, AGA, and LGA) and gestational age category (term, moderately preterm, and very preterm), the subgroup in which mothers previously delivered vaginally was set as the referent.
Covariates
Specific maternal sociodemographic and obstetric complication variables in the second pregnancy were used to assess differences between mothers delivering vaginally and those delivering via cesarean section. The association between maternal obstetric complications and the method of primary birth was assessed on a subset of the population with births between 1989 and 2005, since data collection on complications was not standard in the United States before that time. Maternal characteristics in the second pregnancy, as opposed to the first, were selected because the outcomes (fetal programming patterns and their success) were more likely to be influenced by characteristics in the second pregnancy. These variables included the following: maternal age (younger than 35 years or 35 years and older), race (Black or White), education (<12 years or 12 years or more), marital status (married or unmarried), smoking and alcohol use during pregnancy (yes or no), body mass index (BMI), adequacy of prenatal care (inadequate or adequate), and the inter-pregnancy interval.
The inter-pregnancy interval for each mother was calculated as the number of days between her first and second pregnancies, and was analyzed as a continuous variable. Adequacy of prenatal care (PNC) was assessed by the use of revised graduated index algorithm to describe and assess the level of prenatal care utilization [21, 22]. The trimester of care initiation, number of visits for the duration of the pregnancy, and the infant’s gestational age at birth were used to assess the adequacy of care. Women with missing PNC information, no PNC or those with suboptimal levels of care were classified as having inadequate prenatal care. BMI was calculated using maternal weight in kilograms divided by height in meters squared (kg/m2). Height was obtained from the measurement recorded at the first prenatal visit and pre-pregnancy weight as that reported by the mother during the first visit of each pregnancy [23]. Based on the Institute of Medicine (IOM) Guidelines, maternal pre-pregnancy BMI was categorized as non-obese (<30 kg/m2) and obese (30.0 kg/m2 or more) [24].
Statistical analysis
The Chi-squared (χ 2) test was used to perform crude frequency comparisons between mothers delivering vaginally versus those delivering via cesarean section with respect to selected sociodemographic characteristics and obstetric/medical complications. The independent samples t test was used to assess differences in the means of the inter-pregnancy interval variable between the two groups. We employed logistic regression modeling to compare the odds of fetal growth phenotypes (SGA, AGA, and LGA) across the two groups of women. For each analysis, we controlled for a previous SGA or LGA birth, respectively, as these are known risk factors for subsequent SGA and LGA births [25–27]. The proportionality of days to death and each level of neonatal mortality was assessed. If the proportionality assumption was met, the Cox proportional hazard modeling was used to calculate both crude and adjusted hazard estimates of mortality for each level of intrauterine growth phenotype for infants born via cesarean section. Otherwise, logistic regression modeling was used to calculate the odds ratio. The final model included infant gender, maternal age, race, education, marital status, tobacco use during pregnancy, adequacy of prenatal care, inter-pregnancy interval, and BMI. These variables were selected as potential confounders based on the literature and biologic plausibility. Including obstetric complications in the model produced the same estimates that are presented in Tables 3, 4, and 5. All tests of hypothesis were two-tailed with a type 1 error rate of 5%. Statistical analysis was performed using SAS version 9.2 (SAS Institute, Cary, NC, USA). The study was approved by the Institutional Review Board at the University of South Florida.
Results
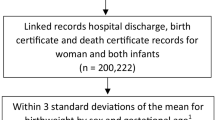
A total of 1,286,874 uniquely identified, singleton live births in the 27-year period between 1978 and 2005 were potentially available to be analyzed in this study. Data from 242,519 (18.8%) records were excluded when the data were restricted to the first two consecutive births for each mother. Records that did not have viable gestational ages of greater than 20 weeks and <44 weeks, totaling 58,405 (4.5%) records, were also excluded. Finally, 85,668 (6.7%) records without sibling pairs, implying only one birth was contributed by the mother in the cohort (n = 80,632); infant birth date, birth weight or death data (n = 1,362); or method of birth information (n = 3,672) was removed from the dataset. After excluding these records, the cohort used in this investigation consisted of 450,141 maternally linked, sibling-matched, singleton, and live birth records. These birth records were further divided into 303,698 vaginal and 146,443 cesarean section deliveries at baseline (first pregnancy).
Table 1 shows the crude frequency comparison between women experiencing a vaginal birth and those delivering via cesarean section in their first pregnancy, with respect to certain social and demographic characteristics. Women having vaginal deliveries in their first pregnancies were more likely to be younger, Black, to have less education and be unmarried in the second pregnancy when compared with women who delivered via cesarean section (P < 0.0001). Conversely, mothers who underwent cesarean section in the first pregnancy were more likely to be obese, non-smokers, to have had adequate level of prenatal care and, on average, have had longer intervals between their first and second pregnancies (P < 0.0001).
The results presented in Table 2 correspond to the subset of women whose first deliveries were between 1989 and 2005. It shows the association between method of birth in the first pregnancy and common maternal obstetric complications in the second. When compared with women who experienced primary vaginal deliveries, women with cesarean sections in the first pregnancy had significantly higher frequencies of obstetric complications in their second pregnancy, including preeclampsia, placenta abruption, and placenta previa. The frequency of eclampsia, chronic hypertension, and diabetes was approximately two times higher as compared to the primary vaginal delivery cohort. The presence of anemia, however, was not different between the cohorts of women (P = 0.9936).
There were 31,118 (7.1%) SGA, 356,019 (79.6%) AGA, and 60,006 (13.3%) LGA infants delivered in the cohort of secondary pregnancies. Table 3 shows the differences between method of delivery in the first pregnancy and infant intrauterine growth phenotype in the second pregnancy. Mothers delivering by cesarean section in the first pregnancy were less likely to deliver subsequent AGA neonates (OR 0.91, 95% CI 0.89–0.92) when compared with mothers delivering vaginally. In contrast, first-time cesarean section delivered mothers were about 3% more likely to deliver LGA neonates in their second pregnancies (OR 1.03, 95% CI 1.01–1.05) than mothers delivering vaginally. The frequency of SGA-delivered neonates was not significantly different between the cohorts of mothers (OR 1.00, 95% CI 0.97–1.02). The results were similar for the different birth weight and gestational age categories (Table 3).
In the second pregnancy, there were 1,147 early neonatal and 310 late neonatal deaths, totaling 1,457 neonatal deaths in this cohort. Of these, 383 early neonatal and 95 late neonatal deaths were to mothers with cesarean section deliveries in the first pregnancy. The frequency of neonatal (P = 0.8228), early neonatal (P = 0.5342), and late neonatal (P = 0.4785) mortality was not significantly different between the cohorts (not shown). Table 4 reports the overall adjusted risk estimates for neonatal, early neonatal, and late neonatal death in the second pregnancy, by each intrauterine growth phenotype, for mothers who delivered via cesarean section in the first pregnancy. For most phenotypes, there were not significantly increased risks for subsequent neonatal death for women with a history of prior cesarean section. Of exception, as compared to women with a previous vaginal delivery, AGA neonates of women with a primary cesarean section had 20% increased risk of both neonatal (OR 1.20, 95% CI 1.05–1.37) and early neonatal (OR 1.23, 95% CI 1.05–1.43) death.
Table 5 shows the adjusted risks of neonatal, early neonatal and late neonatal mortality based on the intrauterine growth phenotypes and gestational age groups. For each phenotype-age group, infants of mothers with a previous vaginal birth were set as the referent category. Almost all c-section-SGA-, AGA-, and LGA-term infants demonstrated a significantly reduced risk of neonatal mortality. LGA-term infants, however, did not show a significantly reduced risk of late neonatal mortality. Infants in all intrauterine growth phenotypes and born moderately preterm did not have a significantly associated risk of neonatal mortality. The infants of women with a primary cesarean section and born very preterm were at increased risk of neonatal mortality for all gestational age categories. The lowest risk were for infants who were born LGA, although these infants exhibited an almost eightfold increased likelihood of early neonatal mortality (OR 7.84, 95% CI 3.32–18.51). Infants who were c-section-AGA-very preterm exhibited greater than 76-fold increased risk of early neonatal mortality as compared to vaginal-AGA-very preterm infants (OR 76.87, 95% CI 64.03–92.28).
Discussion
In our study population, there were consistent and significant differences between the mothers’ primary method of delivery and their social, demographic, and obstetric characteristics in the secondary pregnancies. We sought to determine whether fetal intrauterine growth patterns in the second pregnancy differed based on the delivery method the mother experienced in the first pregnancy. Our hypothesis postulates that the success of fetal programming in the second pregnancy, evidenced by the infant living beyond the neonatal period, would be directly affected by the mothers’ mode of delivery in the first pregnancy. On the whole in our analysis, we were able to confirm that these relationships were present at significant levels of association.
In this study, mothers with a primary cesarean delivery were less likely to deliver an AGA neonate in a subsequent pregnancy, but not significantly more likely to deliver an SGA neonate. They did, however, have a higher frequency of delivering LGA infants than women with the previous vaginal deliveries. Although in contrast to our findings, a Norwegian study of sibship births between 1967 and 2003 found that women with a primary cesarean section had an increased risk of delivering a small-for-gestational age infant in a subsequent pregnancy [28]. In that study, the researchers evaluated women who had two or three pregnancies. For the study cohort with two pregnancies, mothers with an initial cesarean section had a 30% increased risk of delivering a SGA infant in her second pregnancy (OR 1.3, 95% CI 1.3–1.4). Mothers with three pregnancies had approximately the same risk of their third infants being born small-for-gestational age, regardless of whether she had one or two previous cesarean section deliveries [28]. Previous studies in Finland [29] and Australia [30] found similar increased risks for low birth weight, preterm birth, and SGA among second or third gestation infants when the mother experienced a primary cesarean delivery.
Further, we sought to determine whether there were increased risks of early death to successive infants with a maternal history of cesarean section deliveries. With the exception of AGA infants having an increased risk of neonatal and early neonatal mortality, we did not find a significantly increased risk of death after primary cesarean section for the other fetal growth phenotypes.
We further analyzed the data based on the gestational age of the neonate. For all gestational growth phenotypes, infants born at term and whose mothers had a prior c-section delivery demonstrated a reduced risk of mortality. Conversely, almost all neonates born prematurely were at a significantly higher risk of neonatal death. The increased risk of mortality remained consistent across intrauterine growth phenotypes, but was highest among AGA neonates. These results support the results of our previous study which demonstrated that preterm SGA neonates have a significantly increased risk of neonatal death as compared to term, non-SGA infants (OR 17.4, 95% CI 17.0–17.7) [31]. In an additional study, we sought to determine whether previous cesarean delivery was a significant risk factor for stillbirth in subsequent pregnancies. Although our analysis in that study did not show an overall increased risk of stillbirth based on the mother’s prior mode of delivery (P = 0.2), when the analysis was stratified by maternal race, Black mothers with a previous primary cesarean section delivery showed a 40% increased likelihood for stillbirth in the second pregnancy (OR 1.40, 95% CI 1.1–1.7) [31].
Studies have reported that increased placental dysfunction, including placenta previa and placenta abruption, are possible after an initial cesarean section [32, 33]. These relationships could potentially be the link that explains the relationship evidenced between previous cesarean delivery and the increased risk of neonatal mortality. These are important associations of note, considering the increasing frequency of primary elective cesarean sections in the United States. With the realization that initial cesarean sections will likely lead to subsequent sections, it is important to recognize the potential for immediate and long-term effects of choosing a cesarean section, especially when the need is not absolutely necessary.
In this study, although we collected data on the subset of women with recorded common maternal obstetric and medical complications, one limitation of our study is that, due to the nature of the database, we did not consider the underlying reasons for maternal cesarean section in first delivery or the cause for subsequent neonatal deaths for individual records. Previous studies [34, 35] have shown that the use of customized growth curves, which can account for variations inherent to a particular maternal characteristics, such as ethnicity and parity, provides more precise measurements and classification of intrauterine growth phenotypes. In the present study, we used population-based growth curves to classify the phenotypes. As such, some infants could have been placed into categories that would have been more accurately assigned had we used customized growth curves. In addition, without information regarding the indication for cesarean delivery (whether elective or medically necessary), we were not able to determine the exact reason for each cesarean section. However, we were able to examine the overall impact of maternal medical complications on neonatal deaths in subsequent pregnancies and including these variables as potential covariates in our model did not alter the estimates; thus providing evidence that factors other than obstetric complications may have a significant influence on fetal/infant outcomes in subsequent pregnancies.
One strength of our study is the access to a relatively large sample size and the ability to control for a number of factors that could have confounded our results. In addition, by including only women with two subsequent deliveries, we controlled for the potentially confounding factors associated with multiple previous cesarean sections, although this may not be a significant contributory factor. Dalveit et al. [28] used the Norwegian birth records for first, second, and third pregnancies and analyzed whether method of delivery significantly contributed to maternal complications, such as placenta previa and preeclampsia. Among women experiencing a third birth, the risk of development of many complications for women with two previous sections remained the same as, or lower than, that among women who had only one prior cesarean section. An additional strength of this study is the population-based design which enhances the external validity of our findings and reduces the risk of bias arising from sample selection, a source of concern in data derived from individual health facilities.
In summary, we found that mothers with a primary cesarean delivery were less likely to deliver an neonate in a subsequent pregnancy and had a higher frequency of delivering LGA infants than women with previous vaginal deliveries. AGA infants delivered to mothers with a history of c-section exhibited an increased risk of neonatal and early neonatal mortality, whereas other fetal growth phenotypes did not show an increased risk of death after primary cesarean section. Future prospective studies are needed to confirm these findings.
References
Heron M et al (2010) Annual summary of vital statistics: 2007. Pediatrics 125(1):4–15
Chu SY et al (2007) Maternal obesity and risk of cesarean delivery: a meta-analysis. Obes Rev 8(5):385–394
Getahun D et al (2009) Racial and ethnic disparities in the trends in primary cesarean delivery based on indications. Am J Obstet Gynecol 4: 422e1–422e7
Paramsothy P et al (2009) Interpregnancy weight gain and cesarean delivery risk in women with a history of gestational diabetes. Obstet Gynecol 113(4):817–823
Patel RR et al (2005) Prenatal risk factors for caesarean section. Analyses of the ALSPAC cohort of 12, 944 women in England. Int J Epidemiol 34(2):353–367
Bailit JL, Love TE, Mercer B (2004) Rising cesarean rates: are patients sicker? Am J Obstet Gynecol 191(3):800–803
MacDorman MF et al (2006) Infant and neonatal mortality for primary cesarean and vaginal births to women with “no indicated risk”, United States, 1998–2001 birth cohorts. Birth 33(3):175–182
Menacker F (2005) Trends in cesarean rates for first births and repeat cesarean rates for low-risk women: United States, 1990–2003. Natl Vital Stat Rep 54(4):1–8
Smith GC et al (2002) Risk of perinatal death associated with labor after previous cesarean delivery in uncomplicated term pregnancies. JAMA 287(20):4684–4690
Smith GC, Pell JP, Dobbie R (2003) Caesarean section and risk of unexplained stillbirth in subsequent pregnancy. Lancet 362(9398):1779–1784
Towner D et al (1999) Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med 341(23):1709–1714
Salihu HM et al (2006) Risk of stillbirth following a cesarean delivery: Black–White disparity. Obstet Gynecol 107(2 Pt 1):383–390
Martin J et al (2003) Development of the matched multiple birth file. In: 1995–1998 matched multiple birth dataset, NCHS CD-ROM series 21, no. 13a. National Center for Health Statistics, Hyattsville
Herman AA et al (1997) Data linkage methods used in maternally-linked birth and infant death surveillance datasets from the United States (Georgia, Missouri, Utah and Washington State), Israel, Norway, Scotland and Western Australia. Paediatr Perinat Epidemiol 11(Suppl 1):5–22
Alexander GR et al (1998) What are the fetal growth patterns of singletons, twins, and triplets in the United States? Clin Obstet Gynecol 41(1):114–125
Taffel S, Johnson D, Heuser R (1982) A method of imputing length of gestation on birth certificates. Vital Health Stat 2 93:1–11
Piper JM et al (1993) Validation of 1989 Tennessee birth certificates using maternal and newborn hospital records. Am J Epidemiol 137(7):758–768
Wingate MS et al (2007) Comparison of gestational age classifications: date of last menstrual period vs. clinical estimate. Ann Epidemiol 17(6):425–430
Salihu HM et al (2008) AGA-primed uteri compared with SGA-primed uteri and the success of subsequent in utero fetal programming. Obstet Gynecol 111:935–943
Salihu HM et al (2009) Success of programming fetal growth phenotypes among obese women. Obstet Gynecol 114:333–339
Alexander GR, Cornely DA (1987) Prenatal care utilization: its measurement and relationship to pregnancy outcome. Am J Prev Med 3(5):243–253
Alexander GR, Kotelchuck M (1996) Quantifying the adequacy of prenatal care: a comparison of indices. Public Health Rep 111(5):408–418
Herman AA, Yu KF (1997) Adolescent age at first pregnancy and subsequent obesity. Paediatr Perinat Epidemiol 11(Suppl 1):130–141
Parker JD, Abrams B (1992) Prenatal weight gain advice: an examination of the recent prenatal weight gain recommendations of the Institute of Medicine. Obstet Gynecol 79(5 Pt 1):664–669
Ananth CV et al (2009) Recurrence of fetal growth restriction in singleton and twin gestations. J Matern Fetal Neonatal Med 22(8):654–661
Okah FA et al (2010) Risk factors for recurrent small-for-gestational-age birth. Am J Perinatol 27(1):1–7
Walsh CA et al (2007) Recurrence of fetal macrosomia in non-diabetic pregnancies. J Obstet Gynaecol 27(4):374–378
Daltveit AK et al (2008) Cesarean delivery and subsequent pregnancies. Obstet Gynecol 111:1327–1334
Hemminki E, Shelley J, Gissler M (2005) Mode of delivery and problems in subsequent births: a register-based study from Finland. AJOG 193:169–177
Kannare R et al (2007) Risks of adverse outcomes in next birth after a first cesarean delivery. Obstet Gynecol 109:270–276
Kristensen S et al (2007) SGA subtypes and mortality risk among singleton births. Early Hum Dev 83:99–105
Lydon-Rochelle M et al (2001) First-birth cesarean and placental abruption or previa at second birth. Obstet Gynecol 97(5 Pt 1):765–769
Hemminki E, Meriläinen J (1996) Long-term effects of cesarean sections: ectopic pregnancies and placental problems. Am J Obstet Gynecol 174(5):1569–1574
Gardosi J, Francis A (2009) Adverse pregnancy outcome and association with small for gestational age birthweight by customized and population-based percentiles. Am J Obstet Gynecol 201(1):28.e1–28.e8
Gardosi J (2006) New definition of small for gestational age based on fetal growth potential. Horm Res 65(Suppl 3):15–18
Acknowledgments
This study was funded by a Grant from the Flight Attendant Medical Research Institute (FAMRI: 024008) to the first author (Hamisu Salihu, MD, PhD). The funding agency did not play any role in any aspect of the study. We thank the Missouri Department of Health and Senior Services for providing the data files used in this study.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salihu, H.M., Bowen, C.M., Wilson, R.E. et al. The impact of previous cesarean section on the success of future fetal programming pattern. Arch Gynecol Obstet 284, 319–326 (2011). https://doi.org/10.1007/s00404-010-1665-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-010-1665-0