Abstract
Objective
To evaluate perinatal outcome of fetuses with isolated single umbilical artery (SUA), and specifically to examine whether an isolated SUA is an independent risk factor for perinatal mortality.
Methods
A population-based study was conducted, comparing pregnancies of women with and without SUA. Deliveries occurred between the years 1988–2006, in a tertiary medical center. Multiple gestations, chromosomal abnormalities and malformations were excluded from the analysis. Stratified analysis was performed using multiple logistic regression models to evaluate the association between SUA and perinatal mortality, while controlling for confounders.
Results
Out of 194,809 deliveries, 243 (0.1%) were of fetuses with isolated SUA. Fetuses with SUA were smaller (2,844 ± 733 vs. 3,197 ± 530 g, P < 0.001), and were delivered at an earlier gestational age (38.3 ± 3.0 vs. 39.3 ± 2.1 weeks, P < 0.001), when compared with fetuses with normal umbilical vessels. Mothers to fetuses with isolated SUA tended to have a history of infertility treatments (4.5 vs. 1.7%; P = 0.001) when compared with the comparison group. Fetuses with SUA had more complications, including fetal growth restriction (FGR 9.5 vs. 1.9%, P < 0.001), polyhydramnios (11.5 vs. 3.7%; P < 0.001) and oligohydramnios (6.6 vs. 2.2%; P < 0.001). Deliveries of SUA fetuses had higher rates of placental abruption (3.3 vs. 0.7%; P < 0.001), placenta previa (1.2 vs. 0.4%; P = 0.03) and cord prolapse (2.9 vs. 0.4%; P < 0.001). Higher rates of cesarean deliveries were noted in this group (23.9 vs. 12.2%; P < 0.001). SUA newborns had higher rates of low Apgar scores (<7) in one (11.8 vs. 3.7%; P < 0.001) and 5 min (3.5 vs. 0.4%; P < 0.001). Higher rates of perinatal mortality were noted in the SUA group, as compared to fetuses with normal umbilical vessels (6.6 vs. 0.9%, OR 7.78; 95% CI 4.7–13.0; P < 0.001). Using a multiple logistic regression model, controlling for possible confounders, such as FGR, oligohydramnios, polyhydramnios, prolapse of cord, maternal hypertension and diabetes mellitus, isolated SUA remained an independent risk factor for perinatal mortality (adjusted OR = 3.91, 95% CI 2.06–7.43; P < 0.001).
Conclusion
Isolated SUA in our population was noted as an independent risk factor for perinatal mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
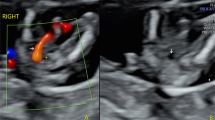
The umbilical cord is formed between day 13th and 38th after fertilization and contains two umbilical arteries and one umbilical vain [1]. Single umbilical artery (SUA) is the most common malformation of the umbilical cord and is associated with birth defects and chromosomal abnormalities [2]. There are number of theories explaining the appearance of an SUA: The first is primary agenesis of one of the arteries of the umbilical cord. The second theory claims that the appearance of an SUA is the result of a secondary atrophy or atresia of once healthy artery. A third theory describes the remaining of the alantoic artery of the primary umbilical cord (body stalk) as an explanation for the appearance of an SUA [3–5]. Embryological considerations as well as the finding of a blocked second umbilical artery in several cases of SUA are factors that support the second theory among the three [1, 6].
The incidence of SUA is 0.2–1.6% in euploids and 9–11% in uneuploid fetuses [6]. SUA is found in 4.6% of twin births and 1% of singletons [1]. Controversy exists regarding the significance of isolated SUA. A survey of eight articles revealed that SUA was found in 1.5% of spontaneous abortions and in 7% of pregnancies terminated due to severe malformations [1, 3]. It was also found that 15–18% of euploid fetuses developed intrauterine fetal growth restriction (FGR) and low birth weight [7–9]. Thummala et al. found a slight increase in renal abnormalities in neonates with SUA, although these findings were not confirmed by Doornebal et al. The latter found that renal abnormalities in fetuses with SUA were comparable with the general population. Both articles concluded that renal investigation is not warranted in the babies with SUA [10, 11]. A comparative examination of middle cerebral artery flow in fetuses with SUA and fetuses with normal umbilical cord showed no significant differences between the two groups [12].
Recently, a research comparing the incidence of FGR and perinatal mortality between fetuses with and without SUA, after excluding major fetal anomalies, concluded that both outcomes were similar and, therefore, concluded that serial antepartum ultrasound for fetal growth is not necessary in managing pregnancies complicated by isolated SUA [13]. Nevertheless, the subject of managing pregnancies with SUA remains controversial, and today all SUA fetuses are considered as high risk pregnancies [14]. The present study was designed to evaluate perinatal outcome of fetuses with SUA, and specifically to examine whether an isolated SUA is an independent risk factor for perinatal mortality.
Materials and methods
A population-based study comparing all singleton pregnancies above 500 g and 22 weeks gestation with and without SUA was conducted. The deliveries occurred between the years 1988 and 2006 at the Soroka University Medical Center. This is a tertiary and the sole hospital in the Negev, the southern part of Israel. The hospital serves the entire obstetrical population in this region. Thus, the study is based on the non-selective data. SUA newborns are known to have higher rates of congenital malformations and chromosomal aberrations [15, 16]. To investigate the association between SUA and various pregnancy and labor complications, we excluded from our analysis fetuses with congenital malformations and chromosomal aberrations. Our sample is composed of 194,809 births, 243 of which had an isolated SUA.
Data were collected from the computerized perinatal database that consists of information recorded directly after delivery by an obstetrician. Only four skilled medical secretaries examine the information routinely before entering it into the database. Coding is done after assessing the medical prenatal care records as well as the routine hospital documents. These procedures assure maximal completeness and accuracy of the database. The midwives evaluate routinely the placenta and cord after delivery and basically SUA was detected and confirmed (if was previously observed by ultrasound) postnatally.
Statistical analysis was performed with the SPSS package. Categorical variants were examined by χ2 test. Comparison of means was calculated using t test or one-way ANOVA. A multivariable logistic regression model, with backward elimination, was constructed to find independent risk factors associated with SUA and to evaluate the association between SUA and perinatal mortality while controlling for confounders. Stratified analysis, using the Mantel–Haenszel technique was used to assess the association between SUA and other variables with clinical significance while controlling for possible confounders. Odds ratios (OR) and their 95% confidence interval (CI) were computed. P < 0.05 was considered statistically significant.
Results
During the study period and after excluding multiple gestations, chromosomal abnormalities and malformations, there were 194,809 deliveries, of which 243 were of fetuses with isolated SUA. Table 1 shows the general clinical characteristics of women with and without SUA pregnancies. Women with SUA tended to deliver at an earlier gestational age, and have smaller babies. There was also a higher rate of infertility treatment in this group, but there was no significant difference in recurrent abortions rate between the two groups.
Table 2 presents this analysis. Pregnancies of fetuses with SUA had more complications, including FGR, polyhydramnios and oligohydramnios. Deliveries of SUA fetuses had higher rate of placental abruption, true knot of umbilical cord and cord prolapse. Higher rates of cesarean deliveries were noted in this group. Higher rate of perinatal complications was noted in the SUA group including low Apgar scores (<7) in one and 5 min and higher rates of perinatal mortality (defined as all cases of intrauterine fetal death, intrapartum death and postpartum mortality).
To further investigate the association between SUA and perinatal mortality, a multivariable analysis, with backward elimination was constructed. After controlling for other possible factors affecting perinatal mortality, such as FGR, diabetes, hypertension, polyhydramnios, oligohydramnios, maternal age, gestational age, cord prolapse and true knot of umbilical cord, SUA remained an independent risk factor for perinatal mortality (OR 3.91, 95% CI 2.06–7.43).
Discussion
The major finding of our study is that SUA is an independent risk factor for perinatal mortality. It was noted as a risk factor for perinatal mortality after excluding cases with congenital malformations and chromosomal aberrations, and also using a multivariable analysis to eliminate possible confounders affecting perinatal mortality. Isolated SUA was also recognized as a risk factor for other major pregnancy complications.
Previous studies regarding isolated SUA have drawn different conclusions. Bombrys et al. [10] have not found a higher rate of perinatal mortality and FGR when comparing isolated SUA to newborns with normal umbilical cord. They have concluded that an isolated SUA pregnancy should be followed up as a normal umbilical cord pregnancy, once a detailed ultrasound has been performed to rule out associated anomalies. Our research has found a significant association between isolated SUA and adverse pregnancy outcomes, including FGR and perinatal mortality, and thus it may be prudent to treat all isolated SUA pregnancies as high risk pregnancies, with tighter follow-up and ultrasound evaluations.
Strengths of this study include the large sample size, enabling ample power to achieve statistical significance; other strength of this study is that the database upon which it is based was compiled using meticulous attention to detail by a highly skilled staff of medical secretaries. The limitations of this study mainly stem from its retrospective design.
In conclusion, in our population, SUA was noted as an independent risk factor for perinatal mortality. Because the diagnosis of isolated SUA carries significant medical and financial implications, further prospective studies including more data on both mother and child, should verify our results to formulate the correct approach for managing these cases.
References
Prucka S, Clemens M, Craven C, McPherson E (2004) Single umbilical artery: what does it mean for the fetus? A case–control analysis of pathologically ascertained cases. Genet Med 6:54–57
Csécsei K, Kovács T, Hinchliffe SA, Papp Z (1993) Incidence and associations of single umbilical artery in prenatally diagnosed malformed, midtrimester fetuses: a review of 62 cases. Am J Med Genet 46(2):248–249
Persutte WH, Hobbins J (1995) Single umbilical artery: a clinical enigma in modern prenatal diagnosis. Ultrasound Obstet Gynecol 6(3):216–229
Romero R, Pilu G, Jeanty P, Ghidini A, Hobbins JC (eds) (1988) Prenatal diagnosis of congenital anomalies. Appleton & Lange, Norwalk
Tanimura T, Ezaki KI (1968) Single umbilical artery found in Japanese embryos. Proc Congenit Anom Res Assoc Jpn 8:27
Predanic M, Perni SC, Friedman A, Chervenak FA, Chasen ST (2005) Fetal growth assessment and neonatal birth weight in fetuses with isolated single umbilical artery. Obstet Gynecol 105:1093–1097
Catanzarite VA, Hendricks SK, Maida C, Westbrook C, Cousins L, Schrimmer D (1995) Prenatal diagnosis of the two vessel cord: implications for patient counseling and obstetric management. Ultrasound Obstet Gynecol 5:98–105
Jauniaux E, De Munter C, Pardou A, Elkhazen N, Rodesch F, Wilkin P (1989) Evaluation echographique du syndrome de l’artere ombilicale unique: une serie de 80 cas. J Gynecol Obstet Biol Reprod 18:341–348
Leung AKC, Robson WLM (1989) Single umbilical artery: a report of 159 cases. Am J Dis Child 143:108–111
Thummala MR, Raju TN, Langenberg P (1998) Isolated single umbilical artery anomaly and the risk for congenital malformations: a meta-analysis. J Pediatr Surg 33(4):580–585
Doornebal N, de Vries TW, Bos AF, de Vries NK (2007) Screening infants with an isolated single umbilical artery for renal anomalies: nonsense? Early Hum Dev 83(9):567–570
Hershkovitz R, Sheiner E, Mazor M (2006) Middle cerebral artery blood flow velocimetry among healthy fetuses with a single umbilical artery. J Ultrasound Med 25(11):1405–1408
Bombrys AE, Neiger R, Hawkins S, Sonek J, Croom C, McKenna D, Ventolini G, Habli M, How H, Sibai B (2008) Pregnancy outcome in isolated single umbilical artery. Am J Perinatol 25(4):239–242
Maternal-Placental-Fetal Unit (2007) Fetal and early neonatal physiology. In: Decherney AH, Goodwin TM, Nathan L, Laufer N (eds) Current diagnosis and treatment OBS & GYN. McGraw-Hill, New York, p 170
Mu SC, Lin CH, Chen YL, Sung TC, Bai CH, Jow GM (2008) The perinatal outcomes of asymptomatic isolated single umbilical artery in full-term neonates. Pediatr Neonatol 49(6):230–233
Deshpande SA, Jog S, Watson H, Gornall A (2009) Do babies with isolated single umbilical artery need routine postnatal renal ultrasonography? Arch Dis Child Fetal Neonatal Ed 94(4):F265–F267 [Epub 8 Jan 2009]
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Burshtein, S., Levy, A., Holcberg, G. et al. Is single umbilical artery an independent risk factor for perinatal mortality?. Arch Gynecol Obstet 283, 191–194 (2011). https://doi.org/10.1007/s00404-009-1326-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-009-1326-3