Abstract
Objective
To assess the intention to use postpartum contraceptives and factors influencing use.
Method
A total of 423 consecutive consenting women attending the pregnancy and puerperal clinics at a university teaching hospital were interviewed using structured questionnaire.
Results
The prevalence of previous contraceptive use was 35.5%. Fifty-four percent of the respondents intended to use contraceptives after delivery, though 3% were yet to decide. Condoms (38.3%) followed by intrauterine contraceptive device (IUCD) 11.5%, were the most preferred choice of postpartum contraceptives. However, spermicide (0.4%) was the least preferred. Advanced age and high parity significantly predicted intention to use postpartum contraceptives (P = 0.02 and 0.01, respectively). Also high level of respondent’s education and family planning counseling by doctors and nurses increased the intention to use postpartum contraceptives (P = 0.03 and 0.01, respectively).
Conclusion
Family planning counseling and education play a vital role in increasing the use of contraceptives in the postpartum period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fertility control with the use of contraceptives is essential to the health and welfare of individuals, families and communities [1]. It is an important tool of preventive medicine that allows couples express their sexual needs without incurring unwanted pregnancies [2]. It has been noted than contraceptives demand fluctuates over the course of women’s reproductive life and as such, the timing of contraceptive service delivery, the choice and contraceptive use must all be considered for effective family planning [3].
Pregnancy and childbirth change priorities, attitudes and lifestyles of women. They have been found to be more receptive to discussions with their care providers regarding different contraceptive methods during this period. Thus, pregnancy and puerperal clinic visits provide opportunities to counsel women because their previous contraceptive method may no longer be desirable or ideal after childbirth [4]. The postpartum period is particularly important because adequate birth spacing can improve maternal and infants health [5].
The worldwide estimate of contraceptive prevalence was 55% with a low prevalence in most developing countries. In Nigeria, the prevalence ranges from 5 to 15% despite a high awareness of contraception [6]. While many studies have investigated the various characteristics of contraceptive users among adolescents, young people, undergraduates, married women and women folk in general, few have focused on the peripartal population [4]. This has led to poor understanding of the contraceptive needs of this target population. Although breast feeding has been shown to provide some measure of contraception [7], this benefit is not well understood by many mothers. Only amenorrhoeic women who exclusively breastfeed at regular intervals including night time during the first 6 months have the contraceptive protection equivalent to that provided by oral contraception [8].
Nursing mothers find it difficult to exclusively breastfeed after resumption of work or while they are students [9]. The consequence of this is many cases of unwanted and unintended pregnancies [2, 9] and its implication on maternal and child health. This study was designed to assess the intention to adopt postpartum contraception, to evaluate the factors influencing this intention and to determine the contraceptive preferences among pregnant and puerperal Nigerian women.
Subjects and methods
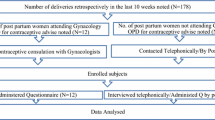
This was a cross-sectional descriptive study to assess the intended postpartum contraceptive use among pregnant and puerperal women in Lagos University Teaching Hospital (LUTH), Lagos, Nigeria and institutional ethical approval was obtained. The pregnancy and puerperal clinics run concurrently between 08:00 and 14:00 h, Monday through Friday with the exception of Wednesdays. The study was undertaken from 1 June 2007 to 30 September 2007. During this period, all consecutive consenting pregnant women either at the booking or subsequent pregnancy clinic visits and women that had given birth within past 6 weeks irrespective of the pregnancy outcome whether live births or stillbirths (puerperal women) were administered structured questionnaire to assess previous contraceptive usage, intention to use contraceptives post delivery, factors that influence their intention as well as their intended contraceptive choices. All puerperal women that had already commenced contraceptive use were excluded from the study. Fisher’s formula (N = Z 2 pq/d 2) was used to calculate the minimum sample size required, which was 196 [10]. This sample size was adjusted further to compensate for non-response rate of 20%. Thus the final minimum sample size was 235. Statistical analysis was performed using Epi-info 6.04 version, categorical variables were compared with chi-square test and Fisher exact test as appropriate while continuous variables were compared using t test. A P value of <0.05 was considered significant.
Results
A total of 423 women were interviewed in the study period, 275 (65.01%) were pregnant while 148 (34.99%) were puerperal women. Overall the mean age of the 423 respondents was 30.6 ± 4.9 years (range 21–40 years) as shown in Table 1, the mean parity was 1.9 ± 1.2 (range 0–6) and the mean duration of marriage was 5.0 ± 3.9 years (range 0–22 years). Four hundred and six (96%) of the respondents were married while 372 (87.9%) were Christians of different dominations with the Pentecostals accounting for the largest proportion (50.3%). Only 13 (3.1%) of the respondents had no formal education while all their partners had formal education. One hundred and fifty (35.5%) had previously used contraceptives before even though 351 (83%) were aware of contraceptives. Two hundred and twenty-seven (54%) of the women intended to use contraceptives after delivery, 184 (43%) do not wish to use contraceptives while 12 (3%) were yet to decide as they wanted further consultations with their husbands, partners and friends. The reasons for wanting to use postpartum contraceptives are given in Table 2 while the reasons for not wanting to use postpartum contraceptives are given in Table 3. However, in 30 women, previous negative experiences with contraceptive use were the reasons given for not wanting to use contraceptives. These include heavy menstrual loss, severe uterine cramps (in previous intrauterine contraceptive device users), irregular menstrual bleeding (in previous users of injectables), excessive weight gain (in previous users of injectables and combined oral pills) and severe acne (in previous users of injectables, combined oral pills and implants). Table 4 shows the preferred postpartum contraceptive choices. Two unmarried students who had unplanned pregnancies following unprotected coitus preferred total abstinence until they are married. Table 5 shows factors that influenced contraceptive choices in these women.
There was no statistically significant difference between the pregnant and puerperal women in the aspect of intention to use contraception and preferred contraceptive method (P > 0.05) as well as work status when working women, non working women and students were compared also in the aspect of intention to use contraception and preferred contraceptive method (P > 0.05). Although majority of the women delivered vaginally (83.1%) compared to caesarean delivery (16.9%), there was no statistically significant difference in their intention to use contraception and preferred contraceptive method (P > 0.05).
The women’s age was found to be significantly associated with intention to use postpartum contraceptives (P = 0.02). The older the respondent, the more their desire to use contraceptives, with the age group 36–40 years accounting for the majority of intended postpartum contraceptive users (Table 1). Also, the level of education of the respondents and their partners, especially university education significantly predicted their intention to use postpartum contraceptives (P = 0.03, P = 0.02) (Tables 1, 6, respectively).
Contraceptive counseling during the course of pregnancy and delivery by doctors and nurses was found to significantly increase intention to use postpartum contraceptives (P = 0.01). Almost all the women counseled intended to use postpartum contraceptives compared to those not counseled (Table 6). Also the higher the parity ≥2 and the higher the intention to use postpartum contraceptives (P = 0.01) (Table 7). It was, however, noted that religion and duration of marriage was not significantly associated with postpartum contraceptive usage (P = 0.12 and P = 1.35, respectively).
Discussion
The prevalence of previous contraceptive use in this study was 35.5%, which is higher than 5–15% observed in other studies [6, 11, 12]. This may be attributed to the high level of contraceptive awareness (83%) observed among this study group. Over the years, the problem of the wide gap between awareness and usage of contraception had been reported [6, 11] which is also reflected in this study. The reasons for this apart from desire for more children could be attributed to religious beliefs, fear of side effects as well as husbands or partners objection to contraceptive usage. Fifty-four percent of the women studied intended to use a contraceptive postpartum which is similar to 58% [13] and 61% [9] in other studies but not as high as 87% of women who desired to use contraceptives after delivery in America [4]. The difference may be related to socio-economic differences in these parts of the world.
The most preferred intended postpartum contraceptive choice in this survey was condom (38.3%), followed by IUCD (11.5%) and Billing’s method (9.7%). The condom was also adjudged the commonest contraception used among the postpartum population in one study [9]. In another study, oral contraceptives and condoms remained the methods most likely considered for use after pregnancy [4]. On the contrary, injectables followed by rhythm method were the common contraceptive methods in another study [2]. The choice of intended postpartum contraceptives by respondents in this study may have been guided by their previous knowledge and use of contraceptives as only 101 (23.9%) of the respondents had contraceptive counseling. Also, their husbands or partners being the major factor indicated by respondents that influenced choice of postpartum contraceptives could have contributed significantly to these choices. It is necessary that health care providers counsel pregnant and puerperal women and their husband and partners on the benefits of contraception as well as allay any fears about side effects. It is not enough to get preoccupied with care of index pregnancies only, such counseling should be continuous and re-enforced during subsequent visits irrespective of how busy such clinics are.
The main reason indicated by the women for not wanting to use postpartum contraceptives was their desire to have more children (47.8%). Another study also identified this as the main reason for non-contraceptive use where it accounted for 36.3% [6]. On the other hand, the desire for child spacing and prevention of further pregnancies were the major reasons for intended use of postpartum contraceptive as found in this study. Also, the finding that higher parity ≥2 and the higher the intention to use postpartum contraceptives compared to lower parity may be associated with increasing age, higher educational level and desire for limited children as confirmed by other similar studies [9, 14, 15]. However, no significant association was found in another study [6].
Advancing age of women was observed to significantly increase the desire to use postpartum contraceptives in this study (P = 0.02). This increase was progressive until it peaked at 36–40 years age range. This is similar to findings in other studies [2, 14]. However, in a developed country, this peak of contraceptive use was at much lower age range [16]. It is expected that a woman’s contraceptive need and preference would change positively over the course of her reproductive age. This accounts for the positive association between the postpartum contraceptives and age. However, a sharp decline in contraceptive prevalence has been noticed close to menopause [2].
The level of education of the women and their partner was found to be significantly related to the desire to use postpartum contraceptives in this study (P = 0.03, 0.02, respectively). This association had been noted in other studies [2, 14, 17]. Level of education above secondary school significantly predicted the use of postpartum contraceptives. Education is a powerful tool for information and empowerment. With good education, couples are aware of the health and economic dangers posted by unplanned pregnancies and the benefits conferred by use of contraceptives to plan and limit child bearing.
Husbands and partners have been shown to contribute significantly to the use and choice of postpartum contraceptives in this study. Other studies have shown that having and living with a partner, predicted intention to use contraceptives [13, 18]. This shows that any factor that influence the partner’s attitude toward contraceptives will also affect the use of postpartum contraceptives either negatively or positively. Thus women do not have full control of their reproductive lives [2]. This gives credence to the fact that husbands or partners need active counseling in order to improve contraceptive acceptance and usage among these women.
The role of health care providers as regards contraceptive use cannot be over-emphasized. Women who received family planning advice during antenatal care were significantly more likely to use contraceptives postpartum than those who did not [3]. In this study, contraceptive counseling by doctors and nurses significantly increase intention to use postpartum contraceptives (P = 0.01). However, only 101 (23.9%) of the women in this study were actually counseled on postpartum contraceptives during pregnancy or even after delivery whereas 87% had the opportunity in another study done else where [4]. It is important to integrate into the antenatal care program, counseling of the women as well as their husbands or partners.
Some of the negative beliefs that were responsible for lack of desire for postpartum contraceptive use identified in this survey like reduction in the chances of future conception after contraceptive use and negative effects on the baby during breast feeding were also observed in another study [3]. It is expected that healthcare providers offer adequate counseling and education to nullify these negative beliefs, offset fears about the negative side effects and also to enable fully informed choices.
Religion did not significantly influence intention to use postpartum contraceptives (P = 0.12) even though the majority of women with intention to use postpartum contraceptives were Christians. This was contrary to the findings in other studies [2, 6, 9, 19]. Similarly, duration of marriage was not a predictor of postpartum contraceptive usage in this study (P = 1.35).
Conclusion
Various factors have been identified in this study as influencing the intention to use postpartum contraceptives. Adequate family planning counseling and education by doctors and nurses of pregnant and puerperal women can modify many of these factors. This education must be extended to their husbands and partners as they play pivotal roles in contraceptive usage. Also improvement in the educational level of the populace will go a long way in improving acceptance of contraceptives in the postpartum period and beyond.
References
World Health Organization (WHO) Family Planning Reproductive Health: health information package of the WHO African Region AFR/INF/99.1
Ogbonna C, Pam IC (2006) A cross sectional study on contraceptive use among married women in Jos, Plateau State. Nig Med Pract 50:107–109
Barber SL (2007) Family planning advice and postpartum contraceptive use among low-income women in Mexico. Int Fam Plann Persp 33:6–12
Cwiak C, Gellasch T, Zieman M (2004) Peripartum contraceptive attitude and practices. Contraception 70:383–386
Levitt C, Shaw E, Wong S, Kaczorowski J, Springate R, Sellors J, Enkin M (2004) Systematic review of the literature on postpartum care: selected contraception methods, postpartum Papanicolaou test and rubella immunization. Birth 31:203–212
Oye-Adeniran BA, Adewole IF, Umoh AV, Oladokun A, Gbadagesin A, Ekanem EE, Yusuf B, Odeyemi KA, Iwere N, Mahmoud P (2006) Community based study of contraceptive behaviour in Nigeria. Afri J Reprod Health 10:90–104
Kennedy KI (1996) Postpartum contraception. Clin Obstet Gynaecol Int Pract Res 10:1–25
Gray RH, Campbell OM, Apelo R, Eslami SS, Zacur H, Ramos RM, Gehret JC, Labbok MH (1990) Risk of ovulation during lactation. Lancet 335:25–29
Ogbonna C, Pam IC (1999) Postpartum contraception: a study of a cohort of nursing mothers in Jos University Teaching Hospital, Jos, Plateau State. Nig Q J Hosp Med 9:293–295
Lwanga SK, Lemeshow S (1991) Sample size determination in health studies: a practical manual. World Health Organization, Geneva (WHO), pp 1–25
Obisesan KA, Adeyemo AA, Fakokunde BO (1998) Awareness and use of family planning methods among married women in Nigeria. East Afr Med J 75:135–138
Population Reference Bureau (2003) 2003 World Population Data Sheet of the Population Reference Bureau.
Newman SJ, Goldberg AB, Aviles R, Molina de Perez O, Foster-Rosales AF (2005) Predictors of contraception knowledge and use among postpartum adolescents in El Salvador. Am J Obstet Gynecol 192:1391–1394
Tehrani FR, Farahani FKA, Hashemi MS (2001) Factors influencing contraceptive use in Tehran. Fam Pract 18:204–208
Ameh N, Sule ST (2007) Contraceptive choices among women in Zaria, Nigeria. Niger J Clin Pract 10:205–207
United States Department of Health and Human Services (2003). Use of Contraception and of Family Planning Services in the US. Centre for Disease Control and Prevention. National Centre for Health Statistics. 1982–2002. A Fact Sheet for Advance Date No. 350
Fikree FF, Khan A, Kadir MM, Sajan F, Ralhbar MH (2001) What influence contraceptive use among young women in urban squatter settlement of Karachi, Pakistan. Int Fam Plann Persp 27:130–135
Harper C, Callegari L, Raine T, Blum M, Darney P (2004) Adolescent clinic visits for contraception: support from mothers, male partners and friends. Perspect Sex Reprod Health 36:88–92
Onuzurike BK, Uzochukwu BSC (2001) Knowledge, attitude and practice of family planning amongst women in a high density low income urban area of Enugu, Nigeria. Afri J Reprod Health 5:83–89
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Adegbola, O., Okunowo, A. Intended postpartum contraceptive use among pregnant and puerperal women at a university teaching hospital. Arch Gynecol Obstet 280, 987–992 (2009). https://doi.org/10.1007/s00404-009-1056-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-009-1056-6