Abstract
Although debated, most preeminent expert panels recommend routine screening for gestational diabetes mellitus (GDM). Among the many tests that have been used and evaluated for the screening of GDM, the fasting plasma glucose (FPG) remains very appealing. It is easy to administer, well tolerated, inexpensive, reproducible and patient friendly. However attractive, the FPG has given varied results in different populations and its use as a screening test for GDM remains uncertain. This review will objectively assess the available studies to find the real value of FPG as a screening test for GDM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite four decades of research, multiple aspects of gestational diabetes mellitus (GDM) still continue to be debated [1]. GDM has been called a riddle, wrapped in a mystery, inside an enigma [2]. It was originally defined to identify pregnant women, who are at a higher risk for developing type 2 diabetes, later in life. GDM is now being linked to many potential fetal and maternal complications in the index pregnancy [3]. There remains a lack of international consensus [4] on the screening, diagnosis, treatment and follow-up of GDM among well-respected panels like the American Diabetes Association (ADA) [5], World Health Organization (WHO) [6] and the American College of Obstetricians and Gynecologists (ACOG) [7], the Canadian Diabetes Association (CDA) [8], the Australasian Diabetes in Pregnancy Society (ADIPS) [9] and the European Association for the Study of Diabetes (EASD) [10]. This lack of agreement among the major diabetes associations continues to cause confusion about the ideal clinical approach to GDM [11].
Justification of screening for GDM
GDM does not fulfill many of the criteria, which make a disease eligible for screening [1]. There is absence of data establishing a clear link between screening for GDM with improved outcome of affected pregnancies [12]. After reviewing all the available data on GDM, at least three major authorities concur: not enough evidence exists to make a case for screening for GDM. The National Institute for Clinical Excellence (NICE) Antenatal Care Guidelines (United Kingdom) advises that routine screening for GDM should not be done [13]. The Health and Technology assessment made interim conclusions but stressed that further research is needed to make conclusions about screening for GDM [14]. The U.S. Preventive Services Task Force, after a rational review of all the existing studies, also takes an ambivalent view, i.e., “proof to recommend or not recommend routine screening for GDM is not sufficient” [1]. However, most well-respected diabetes associations like ADA, ADIPS, CDA and EASD advocate that screening for GDM is desirable.
Performance requirements of screening tests for GDM
Any good screening test should detect most, if not all, patients at risk for a disease. Ideally, a screening test should separate the diseased (more than cut-off threshold, i.e. a highly sensitive test) from the healthy population (less than cut-off threshold, i.e. a highly specific test). A perfect test would separate both these populations. However, usually due to overlap of these two populations, choosing an appropriate cut-off would help a test to be highly sensitive with minimum loss of specificity. If the test has a high-false-positive rate (FPR, the healthy patients with result higher than the chosen cut-off), more patients have to unnecessarily undergo the “gold-standard” diagnostic test. A hypothetical screening test with 100% sensitivity and 0% specificity is of no value; though all the diseased patients will be identified (i.e. 100% sensitivity) as all of them have values more that the selected cut-off, so will all the healthy patients (0% specificity, 100% FPR) be positive. Thus, the entire population to be screened, being positive for the screening test, would need to undergo the confirmatory diagnostic test [15].
Many tests have been used and evaluated for the screening of GDM. Some of these tests are: glycosuria; HBA1c; fructosamine; random plasma glucose; fasting plasma glucose; 50 g, 1-h glucose challenge test (GCT) and the oral glucose tolerance test (OGTT) [16]. The GCT remains the most popular screening test for GDM. The original study showed that it had a sensitivity of 79% with a specificity of 87%, i.e., a false-positive rate of 13%. It is the yardstick to compare all screening tests for GDM [5]. Hence, any study assessing the performance of a screening test should compare it with the performance of the GCT; this comparison being ideally done in its own population.
Diagnosis and diagnostic criteria for GDM
The OGTT is the “gold standard” for the diagnosis of GDM, although it is a test with multiple problems. It is expensive and time-consuming. It is non-physiologic, unpleasant, not reproducible, unrelated to body weight and its predictive value may vary with ethnic origins [16]. Strong arguments have been made for both, retaining the OGTT [17] or abandoning it [18] in non-pregnant adults for the diagnosis of diabetes mellitus. But there has been no such deliberation for GDM. All the expert panels, including the ADA, agree that the OGTT is the confirmatory diagnostic test for GDM, despite the added problems of nausea and vomiting in pregnant women [19]. Hence, the OGTT continues to remain as the diagnostic test for GDM, due to lack of an alternative test.
There is no agreement on the glucose load (75 g vs. 100 g) or the criteria used for diagnosis of GDM [4]. For the 100-g OGTT, the original criteria developed by O’Sullivan and Mahan for whole blood were modified for plasma initially by the National Diabetes Data Group (NDDG), and later by Carpenter and Coustan. The latter thresholds were adapted by the ADA and are currently referred to as the ADA criteria. Though very popular in North America, they also enjoy a worldwide acceptance. The 75-g OGTT has multiple criteria, which are available for its interpretation. These are the thresholds advocated by major diabetic and medical associations like WHO, ADA, CDA, EASD, ADIPS and others as shown in Table 1. Major discrepancies are present among these criteria in their ability to identify women with GDM and their capacity to predict adverse pregnancy outcome [11].
Advantages of FPG as a screening test for GDM
The fasting plasma glucose (FPG) as a screening test for GDM is very attractive; it is easy to administer, well tolerated, inexpensive, reliable and reproducible. It would simplify the algorithm for GDM screening and diagnosis, which is well accepted to be cumbersome [20]. However appealing, the FPG has given varied results in different populations; its use as a screening test in pregnancy remains ambiguous [16]. Many experts agree that though the fasting glucose appears to be promising, further testing is required to ensure satisfactory sensitivity/specificity in various populations [20]. The British Medical Association, in its 2004 guideline agreed that fasting glucose may be as sensitive and predictive of morbidity as glucose tolerance testing, but further work is required to confirm this finding [21].
Historical overview
The feasibility of using FPG as a screening test was originally reported by Mortensen et al. [22]. It was subsequently popularized by Sacks et al. [23]. In 1997, the expert committee of the ADA recommended using the FPG (in non-pregnant adults) instead of the OGTT, for the diagnosis of diabetes mellitus. This ADA reliance, on the FPG for diabetes mellitus diagnosis, has been the reason for the resurgence of interest in the fasting plasma glucose as a screening test for GDM. The WHO (1999) guidelines also emphasized the importance of FPG in the diagnosis of DM in non-pregnant adults.
Subsequently, many studies while studying other tests for GDM screening, incidentally found the usefulness of FPG [24] or otherwise [25]. However, the ADA reliance on FPG in non-pregnant patients has been controversial. The FPG alone does not identify individuals at increased risk of death associated with impaired glucose tolerance [26] and post-challenge hyperglycaemia [27], which is done so by the OGTT. No such controversy exists for the diagnosis of GDM with the OGTT continuing to remain as the confirmatory test.
Problems with studies on FPG as a screening test for GDM
The drawback of many of the earlier studies on FPG as a screening test for gestational diabetes was in the selection criteria, which biased the patients towards having an increased risk for GDM [28]. Any surrogate screening test (e.g. FPG) must not be assessed using a population of the “sickest of the sick” and the findings extrapolated to “the population at large” [29]. A pre-selection of patients on the basis of clinical history or positive GCT creates a higher prevalence, improving the predictive value of the FPG.
Another problem is trying to interpret results in different populations, which have (a) varying prevalence and (b) differing criteria being used for the diagnosis of GDM (Table 1). Also, many studies on FPG as a screening test for GDM use the fasting glucose value of the OGTT, instead of FPG being done separately. This assumes perfect reproducibility of the fasting plasma glucose. But for a few anecdotal reports, the day-to-day reproducibility of the FPG during pregnancy has not been reported [30].
Another pitfall of most studies on FPG as a screening test is that they compare the result of one test (the FPG) to another test (OGTT) rather than examining how the test predicts adverse health outcome [1]. The ideal study would validate FPG with maternal and fetal outcome in a large cohort; but no such studies are available.
FPG screening for GDM: studies with a selection bias
Sacks et al. [23] screened 4,661 pregnant women with the 50-g GCT. In the 968 (21.2%) women with a positive screen who underwent the OGTT, 141 (3.1%) women had GDM. The bias was that all the women did not undergo the definitive OGTT, but only those with a positive GCT. A threshold of 4.9 mmol/l (88 mg/dl) gave a sensitivity/specificity of 80/40%.
Aguiar et al. [31] screened 261 pregnant women at the State University Hospital of Rio de Janeiro, Brazil with the 50-g GCT. Of the 100 women with the positive test, only 77 underwent the 100-g OGTT using NDDG criteria for diagnosis of GDM. They recommend using a FPG threshold of 5.2 mmol/l (93 mg/dl), which showed a sensitivity of 81.3% with a specificity of 74.4%.
Agarwal et al. [32, 33] carried out two studies on FPG as a screening test in their high-risk population. Both the studies had a selection bias and used the 100-g OGTT (ADA criteria) for the diagnosis of GDM. All patients were screened, either clinically or with the 50-g GCT. This resulted in a very high GDM prevalence in an already high-risk population at 27 and 31.2%, respectively, for the two studies.
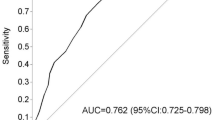
Rey et al. [34] reported the performance of FPG on a 75-g OGTT using the Canadian Diabetes Association criteria, which are very similar to (but slightly more stringent) the ADA criteria. This study had only 188 subjects; the AUC for FPG was 0.81 (95% CI: 0.72–0.90). However, the women were prescreened by the GCT, introducing a bias into assessing the FPG performance.
Senanayake et al. [35] used FPG for screening a high-risk population from Sri Lanka. The women were preselected with risk-factor screening, giving a higher GDM prevalence (27.7%), in their high-risk population. A threshold of 4.7 mmol/l, yielded a sensitivity/specificity of 82.7/67%.
FPG screening for GDM: studies without any selection bias
Reichelt et al. [36] performed a comprehensive study using 5,010 women without any pre selection bias. The FPG performed well to pick up the sub-category of DM (2 h > 11.1 mmol/l), which had only 16/5,020 (0.3%) women but poorly in the majority sub-category of gestational impaired glucose tolerance (GIGT, 2 h = 7.8–11.0 mmol/l) with 363/5,020 (7.2%) women. At their suggested optimal threshold of 4.7 mmol/l, both the sensitivity and specificity in the majority sub-group of GIGT were an unacceptable 68%. If the cut-off was dropped to 4.5% mmol/l, the sensitivity/specificity without sub-groupings (as most studies have done) would be 81.5/54%, with 51% women less than this threshold. Thus, nearly half of their patients would have to undergo the OGTT, to pick up 80% who had GDM. Despite their high false-positive rate, they try to make a case (unsuccessfully, in our view) for FPG as a screening test for GDM. Obtaining slightly worse false-positive rate (57% vs. 46%), Sacks et al. [30] conclude that FPG is not a useful test to screen for GDM as should have been the conclusion of Reichelt’s study.
Peruchini et al. [28] showed an excellent performance of the FPG, in their cohort of 520 pregnant women. They used the ADA criteria with the 3 h, 100-g OGTT. FPG showed an acceptable performance of combined sensitivity and specificity. The study had no pre-selection bias but the overall number of patients was very small. This usefulness of the FPG as a screening test with the 3 h, 100-g OGTT using ADA criteria, having never been duplicated, needs further validation in a larger cohort.
Tam et al. [37] from the Chinese University of Hong Kong, compared 50-g GCT, FPG, 2-h post-breakfast, random glucose and plasma fructosamine in 942 pregnant women. The diagnosis of GDM, which was based on WHO criteria, showed a prevalence of 13%. The AUC for GCT, FPG and 2-h glucose were similar and much better than random glucose and plasma fructosamine. They recommend that rather than using the GCT or post-breakfast glucose, the FPG is a better test for universal screening of GDM (threshold of 4.1 mmol/l.).
Agarwal et al. [38] conducted one study on 1,685 subjects, using the WHO (1999) diagnostic criteria on the 75-g OGTT. The high-false-positive rate made the FPG an inappropriate test for screening for GDM, though it still had value in limiting the number of OGTTs.
Agarwal et al. [39] argued that the variation in FPG performance observed in many studies, may be due to the differing diagnostic criteria used. They compared the effect of four differing diagnostic criteria applied to same 75-g OGTT undergone by a cohort of 4,602 pregnant women. The performance of the FPG a screening test was highly dependent upon the choice of the diagnostic criteria. It was a very useful test to screen for GDM when the ADA criteria (as applied to the 75-g OGTT) were used for making the diagnosis. With the other three criteria (WHO, ADIPS and EASD), at an acceptable sensitivity of 85%, the high FPR and poor specificity would limit its utility as a screening test.
Table 2 summarizes some of the major studies on FPG as a screening test for GDM. We have used a sensitivity of 80–85% to compare the various studies. This was chosen as the most popular test for GDM screening, the GCT, as pointed out earlier, showed a sensitivity of 79%. In general, the studies with a selection bias are not of much use in assessing the value of FPG as a screening test. The studies without a selection bias show that FPG is dependent on the criteria used for diagnosis of GDM. With the WHO criteria, three studies [36, 38, 39] confirm that the poor specificity and high-false-positive rate, would limit the usefulness of FPG as a screening test. However with the ADA criteria, two studies [28, 39] showed a good and acceptable performance. Perucchini’s oft-quoted study [28] used the 100-g OGTT, but had just 520 patients, and needs to be replicated. The other [39] used the 75-g OGTT and was carried out in a high-prevalence population. Moreover, the ADA criteria are usually applied to the 100-g OGTT and uncommonly to the 75-g OGTT, as done in this study. Thus, more studies are needed to reinforce these findings.
FPG screening for GDM: supplementary studies
Atilano et al. [24] tried to find better alternatives to the complicated screening and diagnostic algorithm for GDM. They used the GCT with an abnormally elevated glucose values to predict GDM. In 52 women with a GCT result ≥10.3 mmol/l, only 57% had GDM; even in those women with the GCT result ≥11 mmol/l, only 69% had GDM. Thus, surprisingly, a very abnormal GCT did not perform well to “rule-in” GDM. The performance of an elevated FPG, despite the few patients, was remarkable. An FPG ≥ 5.8 mmol/l predicted GDM in an impressive 96% of their 24 pregnant women. They suggest that an elevated FPG alone may be an “acceptable method of identifying GDM and it may discriminate the highest-risk pregnancies complicated by GDM.” They also recommended that the FPG results should be validated in studies with larger sample sizes, which have been done in subsequent studies.
Maegawa et al. [25] compared multiple screening tests for GDM in 749 pregnant women from 11 Japanese hospitals. The diagnostic test was the 75-g OGTT using criteria of the Japan Diabetes Society. A FPG threshold of 4.7 mmol/l, reached a sensitivity/specificity combination of 71.4/83% and 75/90.6% in the first trimester and at 24–28 weeks, respectively. However, they had only 22 (2.9%) women who had GDM with 14 (63.6%) being diagnosed in the first trimester and the remaining 8 (36.4%) being diagnosed later.
FPG screening for GDM: early pregnancy
The latest bulletin of the ACOG acknowledges that the benefits of treating GDM, if it can be identified early in pregnancy [7]. Glucose screening in early pregnancy can detect 40–96% of GDM, depending on the population and gestational age of initial assessment [40]. Most studies on early pregnancy screening of GDM have used the 50-g GCT. In women with “early-onset GDM,” glucose screening could avoid some diabetes-related complications like hydroamnios, preterm delivery, neonatal hypoglycemia and perinatal death. They are more likely to be hypertensive with higher glycemic values and requiring insulin therapy [41]. Thus, they may represent a high-risk GDM sub-group; an early diagnosis with treatment would result in better prognosis [42].
Theoretically, FPG is not a good method to screen for GDM in early pregnancy. GDM can be considered as type 2 DM evolving in months, rather than years. The worsening insulin resistance is initially compensated by augmentation of insulin production, resulting in a normal fasting glucose. Therefore, as in type 2 DM, the initial abnormality is only post-prandial [16]. Thus, FPG will miss some of those in the early, post-prandial phase. This was confirmed by Sack’s study on FPG screening in early pregnancy [30]; this study is undoubtedly the most-comprehensive and the best-designed study among all the studies in this review. The conclusion was that the false-positive rate, being very high at 57% obviates its use as a screening test in early pregnancy. Similar high-false-positive rates were obtained in other studies on FPG as a screening test in early pregnancy [40]. But with advancing pregnancy, as the patient becomes more glucose intolerant, the FPG may have potential to screen for GDM, later in pregnancy.
In high-risk populations, the case for universal screening during early pregnancy, is strong. The incidence of type 2 DM is increasing world-over and it is occurring more and more at a younger age [11]. As these young women become pregnant, pregnancy is the first time they would be tested for glucose intolerance. Thus, testing all women during early pregnancy is all the more necessary in high-risk populations to identify every woman with pregestational diabetes.
Value of the FPG to simplify the diagnostic approach
The OGTT is often used as both, the screening and the diagnostic test for GDM. This one-step method is advocated by the ADA for high-risk populations. In regions using this approach, the FPG has another potential use: it can be used to limit the number of OGTTs with minimal loss of sensitivity.
A two threshold “rule-in and rule-out” algorithm has been proposed to achieve this purpose [33]. Briefly, two (instead of one) cut-off values are used for a screening test (FPG, in this case). The higher cut-off, which has an inherently increased specificity, is used to “rule-in” the disease under consideration (GDM); while the lower cut-off with its innately increased sensitivity is used to “rule-out” the disease. Subjects who have FPG values, in between these two selected thresholds, are considered “indeterminate” and require the OGTT. Thus, initial testing by FPG can significantly decrease the number of the OGTTs needed for the diagnosis of GDM [38, 39].
In such populations, the laboratory should offer FPG on a stat basis. Based on the result, the decision to stop or proceed with the OGTT can be made: (a) with the higher FPG threshold, it may be possible to “rule-in” GDM in a reasonable number of women using the FPG alone with 100% specificity. The smaller the numerical value of this FPG threshold in the diagnostic criteria (Table 1), the more the number of women who could be “ruled-in” with GDM, and (b) Also, the lower FPG cut-off chosen (in this two-threshold algorithm) can “rule-out” GDM in additional women, who also would not need the OGTT. As seen in Table 2, the number of women below this selected threshold can vary from 25 to 70%, in whom the OGTT can be avoided. Overall, using this algorithm, the FPG could potentially avoid nearly three-fourths (ADA criteria) to over one-third of the OGTTs, depending on the criteria, which were used for the diagnosis of GDM [39]. Other countries and regions, using alternate tests like the GCT, may find it cost-effective to screen with the one-step OGTT with the FPG helping to economize and simplify the diagnostic approach.
Conclusions
Based on the available data, the FPG has two prime uses: (1) FPG as a screening test using one-threshold value: most studies, as pointed in this review, show that FPG is a more sensitive than specific test for GDM screening. Thus, initial testing by FPG would be more useful to “rule-out” rather than “rule-in” GDM. The utility of the FPG as a screening test appears to be dependent upon the diagnostic criteria used. When the ADA diagnostic criteria are used with the 75-g [39] or the 100-g OGTT [28], it appears to be a good test for the screening of GDM. With the other criteria, including the commonly used WHO diagnostic criteria, the poor specificity at any acceptable sensitivity, poor positive predictive value and high-false-positive rate, would limit its usefulness as a screening test. (2) FPG as a screening test using two-threshold values: in populations using or considering the one-step approach to screening and diagnosis of GDM, the FPG could help to avoid 30–70% of the demanding OGTT, again, depending on the diagnostic criteria used for GDM diagnosis [38, 39].
More studies from different populations, without any selection bias, are needed. Only such larger studies, especially those validating the use of FPG against pregnancy outcome [43], will assess its real value as a screening test for GDM.
References
Brody SC, Harris R, Lohr K (2003) Screening for gestational diabetes: a summary of the evidence for the U.S. Preventive Services Task Force. Obstet Gynecol 101:380–392
Agarwal MM, Dhatt GS, Punnose J, Koster G (2006) Gestational diabetes remains a riddle wrapped in a mystery inside an enigma. Acta Obstet Gynecol Scand 85:763
Greene MF (1997) Screening for gestational diabetes mellitus. N Engl J Med 337:1625–1626
Vogel N, Burnand B, Vial Y, Ruiz J, Paccaud F, Hohlfeld P (2000) Screening for gestational diabetes: variation in guidelines. Eur J Obstet Gynecol Reprod Biol 91:29–36
Gestational Diabetes Mellitus (2004) Position statement American Diabetes Association. Diab Care 27(Suppl 1):S88–S90
World Health Organization (1999) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1. Diagnosis and classification of diabetes mellitus. Report of a WHO Consultation, WHO, Geneva
American College of Obstetricians, Gynecologists (2001) Clinical management guidelines for obstetrician–gynecologists. Gestational diabetes. ACOG Practice Bulletin 30. Obstet Gynecol 98:525–538
Canadian Diabetes Association Clinical Practice Guidelines Expert Committee (2003) Canadian Diabetes Association Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. Can J Diabetes 27(Suppl 2):S99–S105
The Australasian Diabetes in Pregnancy Society (1998) Gestational diabetes mellitus guidelines. Med J Aust 169:93–97
Report of the Pregnancy and Neonatal Care Group of the European Association for the Study of Diabetes (1996) Diabet Med 13:S43–S53
Agarwal MM, Dhatt GS, Punnose J, Koster G (2005) Gestational diabetes: dilemma caused by multiple international diagnostic criteria. Diabet Med 22:1731–1736
Greene MF, Solomon CG (2005) Gestational diabetes mellitus—time to treat. N Engl J Med 352:2544–2546
National Collaborating Centre for Women’s, Children’s Health (2003) Antenatal care: routine care for the healthy pregnant woman. RCOG Press, London
Scott DA, Loveman E, McIntyre L, Waugh N (2002) Screening for gestational diabetes: a systematic review and economic evaluation. Health Technol Assess 6:1–172
Agarwal MM, Dhatt GS, Punnose J, Koster G (2005) Gestational diabetes: a reappraisal of HBA1c as a screening test. Acta Obstet Gynecol Scand 84:1159–1163
Hanna FWF, Peters JR (2002) Screening for gestational diabetes; past, present and future. Diabet Med 19:351–358
Tuomilehto J (2002) Point: a glucose tolerance test is important for clinical practice. Diab Care 25:1880–1882
Davidson MB (2002) Counterpoint: the oral glucose tolerance test is superfluous. Diab Care 25:1883–1885
Agarwal MM, Punnose J, Dhatt GS (2004) Gestational diabetes: problems associated with the oral glucose tolerance test. Diab Res Clin Pract 63:73–74
Rey E (1999) Screening for gestational diabetes mellitus. Br Med J 319:798–799
BMA (2004) Diabetes mellitus: an update for healthcare professionals. http://www.bma.org.uk/ap.nsf/Content/Diabetes/$file/diabetes.pdf
Mortensen HB, Molsted-Pedersen L, Kuhl C, Backer P (1985) A screening procedure for diabetes in pregnancy. Diabete Metab 11:249–253
Sacks DA, Greenspoon JS, Fotheringham N (1992) Could the fasting plasma glucose assay be used to screen for gestational diabetes? J Reprod Med 37:907–909
Atilano LC, Lee-Parritz A, Lieberman E, Cohen AP, Barbieri R (1999) Alternative methods of diagnosing gestational diabetes mellitus. Am J Obstet Gynecol 181:1158–1161
Maegawa Y, Sugiyama T, Kusaka H, Mitao M, Toyoda N (2003) Screening tests for gestational diabetes in Japan in the 1st and 2nd trimester of pregnancy. Diab Res Clin Pract 62:47–53
The DECODE Study Group (Diabetes Epidemiology: Collaborative Analysis Of Diagnostic Criteria in Europe) (1999) Glucose tolerance and mortality: comparison of WHO and American Diabetes Association diagnostic criteria. Lancet 354:617–621
DECODE Study (Diabetes Epidemiology: Collaborative Analysis Of Diagnostic Criteria in Europe) (1999) Consequences of the new diagnostic criteria for diabetes in older men and women. Diab Care 22:1667–1671
Perucchini D, Fischer U, Spinas GA, Huch R, Huch A, Lehmann R (1999) Using fasting plasma glucose concentrations to screen for gestational diabetes mellitus: prospective population based study. BMJ 319:812–815
Henderson AR (1993) Assessing test accuracy and its clinical consequences: a primer for receiver operating characteristic curve analysis. Ann Clin Biochem 30:521–539
Sacks DA, Chen W, Wolde-Tsadik G, Buchanan TA (2003) Fasting plasma glucose test at the first prenatal visit as a screen for gestational diabetes. Obstet Gynecol 101:1197–1203
de Aguiar LG, de Matos HJ, de Brito Gomes M (2001) Could fasting plasma glucose be used for screening high-risk outpatients for gestational diabetes mellitus? Diab Care 24:954–955
Agarwal MM, Hughes PF, Ezimokhai M (2000) Screening for gestational diabetes in a high risk population using fasting plasma glucose. Int J Gynecol Obstet 68:147–148
Agarwal MM, Hughes PF, Punnose J, Ezimokhai M (2000) Fasting plasma glucose as a screening test for gestational diabetes in a multi-ethnic, high-risk population. Diabet Med 17:720–726
Rey E, Hudon L, Michon N, Boucher P, Ethier J, Saint-Louis P (2004) Fasting plasma glucose versus glucose challenge test: screening for gestational diabetes and cost effectiveness. Clin Biochem 37:780–784
Senanayake H, Seneviratne S, Ariyaratne H, Wijeratne S (2006) Screening for gestational diabetes mellitus in southern Asian women. J Obstet Gynaecol Res 32:286–291
Reichelt AJ, Spichler ER, Branchtein L, Nucci LB, Franco LJ, Schmidt MI (1998) Fasting plasma glucose is a useful test for the detection of gestational diabetes. Brazilian Study of Gestational Diabetes (EBDG) Working Group. Diab Care 21:1246–1249
Tam WH, Rogers MS, Yip SK, Lau TK, Leung TY (2000) Which screening test is the best for gestational impaired glucose tolerance and gestational diabetes mellitus? Diab Care 23:1432
Agarwal MM, Dhatt GS, Punnose J, Koster G (2005) Gestational diabetes in a high-risk population: using the fasting plasma glucose to simplify the diagnostic algorithm. Eur J Obstet Gynecol Reprod Biol 120:39–44
Agarwal MM, Dhatt GS, Punnose J (in press) Gestational diabetes: utility of fasting plasma glucose as a screening test depends upon the diagnostic criteria. Diabet Med
Agarwal MM, Dhatt GS, Punnose J, Zayed R (in press) Gestational diabetes: fasting and post-prandial glucose as first prenatal visit screening tests in a high-risk population. J Reprod Med
Svare JA, Hansen BB, Molsted-Pedersen L (2001). Perinatal complications in women with gestational diabetes mellitus. Acta Obstet Gynecol Scand 80:899–904
Bartha JL, Martinez-Del-Fresno P, Comino-Delgado R (2000) Gestational diabetes mellitus diagnosed during early pregnancy. Am J Obstet Gynecol 182:346–350
Ouzilleau C, Roy MA, Leblanc L, Carpentier A, Maheux P (2003) An observational study comparing 2-hour 75-g oral glucose tolerance with fasting plasma glucose in pregnant women: both poorly predictive of birth weight. CMAJ 168:403–409
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Agarwal, M.M., Dhatt, G.S. Fasting plasma glucose as a screening test for gestational diabetes mellitus. Arch Gynecol Obstet 275, 81–87 (2007). https://doi.org/10.1007/s00404-006-0245-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-006-0245-9