Summary
Purpose: The aim of the study was to determine the short- and long-term efficacy of an intensive and EMG-biofeedback-assisted pelvic floor muscle training (PFMT) program as a therapy of female stress or mixed urinary incontinence. Materials and methods: All women with stress or mixed urinary incontinence treated in the pelvic floor reeducation program at our clinic between September 1996 and March 2003 were included. EMG-biofeedback assisted PFMT was performed by specially trained therapists (one registered nurse and one midwife). Electric stimulation preceded PFMT if the pelvic floor muscle contractions were considered too weak for active training (Oxford < 2). Examinations included among others: conventional urodynamic studies prior to therapy, a stress provocation test (cough test), and determination of maximal pelvic floor muscle strength (Oxford-grading and electric EMG-potential). A retrospective chart review was performed. A questionnaire was administered for long-term follow-up. Results: Four hundred and thirty four women attended our PFR-program in this 7-year period. All 390 women with stress (80%) or mixed (20%) urinary incontinence were evaluated. Mean age: 52 years. Mean duration of incontinence: 6.7 years. Two hundred and sixty three women completed the training (group 1, average number of training sessions: 8.7), 127 patients ended therapy prematurely (group 2, average number of training sessions: 4.1). Short-term results at the end of the PFR-program are available for group 1. There was a statistically significant improvement of the stress provocation test (cough test). The data before the therapy was 141× SUI °III (60%); 50× SUI °II (21%), 24× SUI °I (10%), 20× SUI °0 (9%) as opposed to after the therapy 9× SUI °III (5%), 34× SUI °II (19%), 48× SUI °I (26%), 91× SUI °0 (50%). There was a significant increase in the Oxford-score by 1.2 points (2.9–4.1; P<0.001). Self-reported improvement of incontinence symptoms was 95%. The electric EMG-potentials almost doubled (11.3–20.5 μV; P<0.001). Long-term results (questionnaire) for all patients: the average follow-up time was 2.8 years (range: 3 months to 7 years). Three hundred and twelve (80%) of the questionnaires returned. Seventy-one percent of them self-reported a persisting improvement of their incontinence symptoms. Thirteen percent of all women underwent incontinence surgery following the completion of conservative therapy (9.2% group 1, 25% group 1; P<0.001). Conclusions: An intensive and EMG-biofeedback assisted PFMT is very effective. Often, avoidance of surgery is possible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary incontinence is common among women and has a tremendous impact on their quality of life. It is generally agreed that the first treatment choice should be the least invasive option with the lowest risk for adverse complications [8]. Pelvic floor muscle training (PFMT) is an accepted therapy to improve or cure symptoms of stress urinary incontinence (involuntary leakage from effort or exertion, or from sneezing or coughing) or mixed urinary incontinence (involuntary leakage also associated with urgency in addition to stress incontinence) [1, 7]. However, there are only few studies with a large number of patients that have reported long-term data on the efficacy of EMG-biofeedback assisted PFMT. The aim of the study was to evaluate the efficacy of an intensive and EMG-biofeedback controlled pelvic floor reeducation (PFR) program as a therapy of stress or mixed urinary incontinence with regard to short- and long-term subjective and objective outcome.
Patients and methods
We included all women who participated in our PFR program in September 1996 to March 2003. Admission into this program was basically offered to all women with stress urinary (SUI) of mixed incontinence that had an outpatient visit at our Urogynaecologic Clinic at the Department of Obstetrics and Gynaecology (University Hospital Munich–Großhadern). According to the criteria of the International Continence Society (ICS), usually women with a genital prolapse of grade 3 or 4 and who are not motivated could not participate in an active treatment protocol [1]. To avoid any selection bias, all women with stress or mixed incontinence were included for analysis. All records were reviewed. All patient’s data was documented carefully and from November 1999 onwards a computer based documentation software was included.
A thorough urogynaecological examination was performed before inclusion in our PFR-program: a gynaecological examination was done to check for signs of genital atrophy and prolapse. Conventional urodynamic studies were performed as per the recommendations of the ICS [10]. A computer-assisted urodynamic unit was used (Andromeda Ellipse urodynamic system, AUDACT analysis software, Taufkirchen, Germany). The women were positioned on a gynaecological chair (half sitting). The intra-vesical (p ves) and intra-urethral (p ura) pressures [along the whole length of the urethra (urethral pressure profile); withdrawal speed: 1 mm/s] were recorded with a flexible multisensor microtip transducer catheter (Andromeda, 8 Charr, polyurethan) with a ventral orientation of the transducers at rest with a bladder volume of 100 ml. A stress provocation test (cough test, bladder-filling: 400 ml) was used to grade the severity of SUI: observation of jet-leakage of urine in supine position = SUI °III; jet-leakage of urine in the standing position = SUI °II; drop-leakage of urine in the standing position = SUI °I; no leakage during coughing = SUI °0. Assessment of pelvic floor muscle strength was performed with a vaginal palpation, the woman in the lithotomy position. The woman was instructed to contract the levator ani muscle as forcefully as possible. The effort was graded with the Oxford-score (0 = nil; 1 = flicker; 2 = weak; 3 = medium; slight lift of the examiners finger, no resistance, 4 = strong, sufficient to elevate the examiner’s finger against light resistance, 5 = very strong, sufficient to elevate the examiner’s finger against strong resistance). In addition, we determined the pelvic floor EMG-potentials with vaginal surface electrodes as an objective measure of the maximal pelvic floor contraction strength.
Long-term follow-up consisted of a postal questionnaire covering 18 items that was sent to all participants in August 2003. It included questions about rates of self-reported cure or improvement of incontinence symptoms, present severity of urine loss (amount and frequency), changes of incontinence symptoms since completion of the conservative therapy, life-quality, personal benefit with regard to the PFR participation (100-mm visual analogue scale: 0 = not at all; 10 = very much) and incontinence surgery since completion of the pelvic floor training program.
The PFR training was carried out by two specially trained therapists (one nurse, one midwife). According to our PFR concept all patients received a thorough incontinence counselling, individual instructions for pelvic floor exercises and supporting coping strategies. For PFR, women were carefully instructed to perform a correct pelvic muscle contraction. If the patient was not able to contract to an equivalent to Oxford 2, training was usually initiated with electric stimulation therapy. As soon as Oxford 2 was reached, therapy was performed by active contractions with biofeedback therapy. Then the patient was taught to contract the levator ani muscle fast and sustained with biofeedback control. Patients performed one to two 10 min training sessions per day at home for 3–6 months. The sessions were documented automatically, every time they did their exercises, by the EMG-biofeedback device in order to monitor the patients’ compliance. An EMG-controlled device with a vaginal electrode (ST2001, Haynl Electronic, Germany) was used for biofeedback. The probe has two electrodes that semi quantitatively record mass potentials produced by muscle contractions. The signal intensity is visualised on a light scale. Patients presented for follow-up visits every 4–12 weeks. The scheduled final session included a final assessment of incontinence symptoms and of various pelvic floor parameters (e.g. electric EMG-potentials, Oxford-score).
Statistics
For statistical analysis the SPSS-software (12.0) was used. Proportions were compared using the Chi-squared tests or Fisher’s exact test when appropriate. T test or Wilcoxon test was used for continuous variables (paired differences for electric EMG-potentials and Oxford-scores).
Results
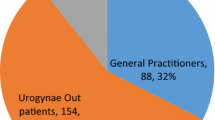
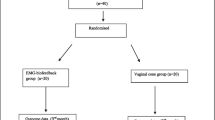
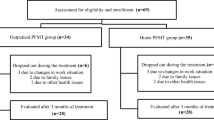
Four hundred and thirty four women participated in the PFR program at the Urogynaecologic Outpatient Clinic at our Department of Obstetrics and Gynaecology. For the analysis we included all women with stress or mixed urinary incontinence resulting in 390 patients. Twenty-nine patients (6.7%) with pure urge incontinence, five patients with unclear diagnosis, and ten patients that participated in our PFR program because of reasons other than urinary incontinence (“pelvic floor muscle weakness”, descensus genitalis without urinary incontinence, pure anal incontinence etc.) have been excluded. Patient characteristics of the remaining 390 women are listed in Table 1. We identified two groups of patients: 263 (67%) women completed the training (group 1) and 127 patients broke off therapy prematurely (group 2). Reasons for breaking off the training program included among others: pregnancy, lack of time or motivation to hold onto the training protocol. Short-term results are only available for group 1 and are listed in Table 2. Long-term results (average follow-up: 2.9 years, range: 3 months to 7 years) include all patients (groups 1 and 2). The return rate of the questionnaires was 80% (n=312) . The return rate in group 1 was significantly higher than in group 2 (229 [87%] vs 83 [65%]; P<0.001). Table 3 shows the rates of incontinence surgery for all patients, for groups 1 and 2. Table 4 shows the long-term results of all patients, inclusive and exclusive of those women on whom an incontinence surgery was done after finishing with our PFMT program. The average number of sessions in group 1 was 8.7±3.3 and in group 2 4.1±3.0 (P<0.001). Table 5 shows the improvement of, termed in German “Leidensdruck”—the perceived burden of suffering due to symptoms of urinary incontinence before and after PFMT with regard to long-term follow-up. At follow-up, 30% still performed PFMT daily, 29% weekly, 35% rarely, 7% never (no significant difference between group 1 and group 2; data not shown).
Discussion
This is one of the largest studies that evaluates PFMT for conservative therapy of stress or mixed urinary incontinence. We present a comprehensive analysis of the efficacy of an intensive PFR program over a time period of 7 years with 390 patients. We found a significant and long lasting therapeutic effect of PFMT. It is important to realise, that prior to therapy more than half of the women had a high grade stress incontinence (grade III on stress provocation test), whereas directly after completion of the therapy only 5% women had a SUI °III. Simultaneously, the pelvic floor contraction strength has increased considerably (Oxford-score 2.9–4.1) and the measured electric EMG-potentials have almost doubled from 11.3 μV to 21.5 μV. This observation is paralleled by the high number of self-reported improvement (94%) and patients’ satisfaction with the therapeutic result (Table 2). This shows, that PFMT is effective even with severe urinary incontinence. Improvement can be demonstrated by both subjective and objective means.
More important than these short-term results are the self-reported long-term results assessed with a thoroughly designed questionnaire, that was sent to all 390 patients. The return rate of 80% is acceptably high and is able to give a clear picture of the efficacy of our PFR program. Overall, after 3 years, 71% of all women still report a persisting improvement of their urinary incontinence symptoms (Table 4). It is interesting that those women who broke off the therapy prematurely (group 2) show similar results in comparison to the general study population (data not shown). However, the return rate in group 2 is considerably lower (65%) than in group 1 (87%). Thus, it is possible that failure rates in group 2 are underreported.
PFMT is the most commonly used physical therapy in the treatment of urinary incontinence. A Cochrane systematic review found that PFMT was more effective than no treatment or placebo [7]. There are several studies that have focused on long-term results of PFMT. The reported rates of successful outcomes (cure and/or improvement) range between 36% and 71% with various follow-up time periods ranging from 3 months up to 10 years [3, 6, 9, 11, 12]. Thus, our long-term success rate of 71% is within the high range of the reported rates found in literature. However, studies of PFMT varied in terms of the characteristics of participants (e.g. inclusion of patients with urgency or urge incontinence, definition of SUI etc.), the parameters of PFMT programs (e.g. number of contractions, number of exercise sessions per day etc.) and the use of PFMT as a single intervention or in combination with other techniques (e.g. biofeedback, electric stimulation) and with regard to the definition of success (e.g. self-reported cure rates, with or without pad weight testing etc). For that reason, comparison of treatment results is difficult.
An important measure of treatment’s success is the rate of incontinence surgery after completion of therapy. In our study, only 13% of all patients had undergone operative treatment after finishing the PFMT (Table 3). This rate is lower than that of other studies. Hahn reports in a comparable study with a similar follow-up period of 2–7 years, a surgery rate of 25% [6]. In our study, the surgery rate in group 1 is considerably lower (9%) than in group 2 (25%). This allows different interpretations: it could be that motivation and compliance of the women in group 2 are lower than in group 1 (perhaps partly explaining the lower return rate of the questionnaires in group 2). It seems to be obvious that efficacy is correlated to patient compliance. However, it is possible that women in group 1 experienced an improvement of their incontinence symptoms earlier (already after the first sessions) than the women in group 2, resulting in a positive reinforcement, thus increasing the compliance and motivation. This signifies that actually women in group 2 had a lower a priori success rate of conservative treatment. Nevertheless, it is not possible to sort out factors that could predict success (data not shown). That is why, offering a conservative approach to all women with stress or mixed urinary incontinence is justified.
PFMT can be done with or without assisted biofeedback techniques to help an individual isolate the relevant muscles. However, results of different studies and systematic reviews on whether PFMT with biofeedback is better than PFMT alone are conflicting. Some studies report in favour of added biofeedback [4, 5]. Other studies, including the recent Cochrane meta-analysis, did not find a benefit from added biofeedback [2, 7, 13]. As a consequence, the authors of the Cochrane review postulate that “there is clearly a need for a regularly updated and comprehensive systematic review of the effectiveness of PFMT for women with urinary incontinence,...”. Due to our study design we cannot answer the question whether PFMT with biofeedback is superior to PFMT without biofeedback. From our data, however, we can conclude that an intensive and EMG-biofeedback assisted PFMT is an effective therapy in treating women with stress or mixed urinary incontinence.
Conclusion
An intensive pelvic floor training with EMG-controlled biofeedback therapy is very effective. Avoidance of an operative therapy is often possible. For that reason, conservative therapy should be offered to most women with stress or mixed urinary incontinence prior to surgery.
References
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck P, Victor A, Wein A (2003) The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 61(1):37–49
Berghmans LC, Hendriks HJ, Bo K, Hay-Smith EJ, de Bie RA, van Waalwijk van Doorn ES (1998) Conservative treatment of stress urinary incontinence in women: a systematic review of randomized clinical trials. Br J Urol 82(2):181–191
Cammu H, Van Nylen M, Amy JJ (2000) A 10-year follow-up after Kegel pelvic floor muscle exercises for genuine stress incontinence. BJU Int 85(6):655–658
de Kruif YP, van Wegen EE (1996) Pelvic floor muscle exercise therapy with myofeedback for women with stress urinary incontinence: a meta-analysis. Physiotherapy 82(2):107–113
Glavind K, Laursen B, Jaquet A (1998) Efficacy of biofeedback in the treatment of urinary stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct 9(3):151–153
Hahn I, Milsom I, Fall M, Ekelund P (1993) Long-term results of pelvic floor training in female stress urinary incontinence. Br J Urol 72(4):421–427
Hay-Smith EJ, Bo Berghmans LC, Hendriks HJ, de Bie RA, van Waalwijk van Doorn ES (2001) Pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst Rev (1):CD001407
Holroyd-Leduc JM, Straus SE (2004) Management of urinary incontinence in women: scientific review. JAMA 291(8):986–995
Jundt K, Peschers UM, Dimpfl T (2002) Long-term efficacy of pelvic floor re-education with EMG-controlled biofeedback. Eur J Obstet Gynecol Reprod Biol 105(2):181–185
Lose G, Griffiths D, Hosker G, Kulseng-Hanssen S, Perucchini D, Schafer W, Thind P, Versi E (2002) Standardisation of urethral pressure measurement: report from the Standardisation Sub-Committee of the International Continence Society. Neurourol Urodyn 21(3):258–260
McIntosh LJ, Frahm JD, Mallett VT, Richardson DA (1993) Pelvic floor rehabilitation in the treatment of incontinence. J Reprod Med 38(9):662–666
Stein M, Discippio W, Davia M, Taub H (1995) Biofeedback for the treatment of stress and urge incontinence. J Urol 153(3 Pt 1):641–643
Weatherall M (1999) Biofeedback or pelvic floor muscle exercises for female genuine stress incontinence: a meta-analysis of trials identified in a systematic review. BJU Int 83(9):1015–1016
Acknowledgements
We want to thank Mrs. Denise Dannecker for critically proof-reading the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dannecker, C., Wolf, V., Raab, R. et al. EMG-biofeedback assisted pelvic floor muscle training is an effective therapy of stress urinary or mixed incontinence: a 7-year experience with 390 patients. Arch Gynecol Obstet 273, 93–97 (2005). https://doi.org/10.1007/s00404-005-0011-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-005-0011-4