Abstract
Eczema resulting from external and internal factors accounts for the biggest global burden of disability owing to skin disease. This study aimed to determine an association between environmental factors and outpatient clinic visits for eczema. We collected data on dermatology clinic outpatient visits for eczema between January 2013 and July 2019. Data concerning environmental factors during this period were collated using national air quality network and air monitoring measurement parameters, namely barometric pressure, relative humidity, air temperature, and air pollutant concentrations, such as sulfur dioxide (SO2) and particulate matter (PM10). A distributed lag nonlinear model was used to investigate the relationship among eczema, environmental factors, and lagged effects. In total, 27,549 outpatient visits for eczema were recorded. In both single-factor and multiple-factor lag models, the effects of a 10-µg/m3 increase in PM10 and SO2 values had significantly positive effects on the number of daily outpatient visits over a total 5 days of lag after adjusting for temperature, the number of daily outpatient visits increased with 0.87%, 7.65% and 0.69%, 5.34%, respectively. Relative humidity (RR = 1.3870, 95% CI 1.3117–1.4665) and pressure (RR = 1.0394, 95% CI 1.0071–1.0727) had significantly positive effects on the number of daily outpatients in single-factor lag models. However temperature had a significantly negative effect on them in the number of daily outpatients (RR = 0.9686, 95% CI 0.9556–0.9819). Exposure to air pollution exacerbated eczema. Outpatient visits for eczema were found to have strong positive associations with changes in PM10 levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Air pollution is a mixture of solid particulate pollutants and gases in ambient air [27]. Among air pollutants, particulate matter (PM10), nitrogen dioxide (NO2), sulfur dioxide (SO2), and ozone (O3) are the most commonly monitored pollutants [22]. Air pollution consistently ranks high among risk factors for death and disability worldwide, with almost 5 million deaths globally, i.e., nearly one in every ten deaths in 2017 according to the World Health Organization data [11]. Exposure to PM in long-term environmental air pollution causes ischemic heart disease, cerebrovascular disease, lung cancer, chronic obstructive pulmonary disease, lower respiratory infections, and, more recently, diabetes mellitus [11, 24]. Increasing amounts of air pollutants have major effects on the skin. The skin has a protective role against physical air pollutants and pro-oxidative chemicals. However, if exposure to high-level detrimental pollutants is prolonged or repetitive, negative effects on the skin can be observed [23]. Eczema generally presents as atopic dermatitis, irritant contact dermatitis, and allergic contact dermatitis [18]. Previous studies have investigated the effects of internal and external factors on eczematous lesions, demonstrating that infections, food intake, genetic predisposition, stress, and inhalant allergens play a role in exacerbating eczematous lesions [2, 18]. Many studies investigating the effects of air pollutants and environmental factors, including relative humidity, wind speed, and temperature, on the exacerbation of eczematous rashes have shown the important role these factors play [1, 8, 10, 18]. Düzce is a province in Turkey where has a warm-temperate humid climate and intensive rainfall [12]. In addition, PM10 pollution is problematic owing to the local topography, types of heating, and industrial infrastructure [28].
This study aimed to investigate relative humidity, barometric pressure, air temperature, and air pollutant concentrations such as SO2 and PM10 to determine a relationship between these factors and the number of eczema-related outpatient clinic visits in Düzce.
Materials and methods
Air pollution and meteorological data
Meteorological data between January 1, 2013 and July 11, 2019 were collated. In the same period, air monitoring measurement parameters of the Turkish national air quality network (PM10, SO2, air temperature, air pressure, and relative humidity) were obtained from the network’s website (https://laboratory.cevre.gov.tr/Default.ltr.aspx).
Patient selection
Patients visiting dermatology weekday outpatient clinics between January 1, 2013 and July 11, 2019 were included in the study. Patient information located in the registration data system was accessed using the following ICD codes: L-20, L-25, and L-30. Patients who resided outside the province of Düzce were excluded from the study. Some residential areas in Düzce province use stoves for domestic heating; therefore, in the address registration information, patients living in these areas were excluded. Patients whose etiology had been determined during an examination and recorded in the patient information data set were excluded from the study.
All study participants provided informed consent, and the study design was approved by the Düzce University ethics review board (2019/132).
Statistical analysis
Appropriate descriptive statistics for all variables in the study were calculated. The proportion of missing data was 0.13% for SO2 air pollutant values. A moving average method was used to replace the missing data. First, a mixed-effects model (Poisson log linear link function and post hoc: sequential Bonferroni method) was created to examine the interaction effect of year and season on the number of daily outpatients with eczema without considering the effects of environmental factors. The relationships between air pollution and meteorological factors were analyzed using Spearman’s correlation coefficients. The effects of environmental stressors on health can occur several days post-exposure to a stressor, and the exposure to high levels of air pollution or extreme temperatures can affect health over a period of several days post-exposure [6]. Therefore, lag effects of air pollution and meteorological factors were evaluated using a distributed lag nonlinear model (DLNM) [5], and the relationship between the daily number of patients and environmental factors was estimated as daily lag and up to 5 days lag. Each air pollution factor was modeled both individually and in combination, and several models were created using different combinations, including the effects of meteorological factors. Given that the number of daily outpatients with eczema as a dependent variable in the model was very small, the predictions of the model were obtained by assuming that this variable had Poisson distribution. Distributed lag nonlinear models were created to cover both a single air pollution factor and two air pollution factors. The basic model was determined as follows:
where \({Y}_{t}\) represents the number of outpatients with eczema on day t, α is the intercept, β is the estimated parameter vector showing the effects of environmental factors, and \({X}_{t}\) shows the daily average air pollution (PM10 and SO2) concentration values accumulated from the current day (lag 0) to the five previous days (lag 5), or it shows the values of meteorological factors (relative humidity and pressure). In the basic model, temperature was considered a covariate, and the single and double effects of each meteorological factor were also included in the model. The effects of air pollution factors on the number of daily outpatient visits owing to eczema were examined. The “day” was included in the model as a categorical variable indicating the day of the week. The daily number of eczema-related outpatient visits was generally small; therefore, no additional statistical evaluations could be made according to gender. However, to test model stability, different degree of freedom (df) values (df 5–7) were considered, and sensitivity analysis was performed. Residual autocorrelation of the models was also undertaken. Akaike information criteria and null deviance and residual deviance criteria were used to determine the best fitting models. Relative risk (RR) test results showed the effect of each of these environmental factors on the daily number of patients in cases where air pollution factors had a 10 µg/m3 increase in the DLNM, a temperature increase of 1 °C, a 10% relative humidity increase, and a 1-hbar increase in pressure. The RR and 95% confidence interval (CI) values were calculated. SPSS 22 (IBM Corp., Armonk, NY, USA) and R CRAN programming language were used for statistical analysis. A p value < 0.05 was considered statistically significant.
Results
Between January 1, 2013 and July 11, 2019, 27,549 patients with eczema who attended the dermatology outpatient clinic of Düzce University Faculty of Medicine were included in this study. Of these, 15,879 (57.6%) patients were female and 11,670 (42.4%) were male. The average daily number of eczema-related dermatology outpatient visits was 17.6 ± 7.2 (2–41).
Descriptive statistics concerning the number of daily outpatients with eczema, daily air pollution, and meteorological factors recorded between January 1, 2013 and July 11, 2019 are presented in Table 1.
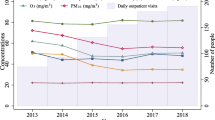
The effect of year and season on the daily number of patients
When the number of daily outpatients with eczema according to years and seasons was examined using a mixed-effects model (LR-χ2 = 866.17, df = 26, p < 0.001), the interaction effect (year × season) showing the effect of both year and season combined was significant in relation to the number of daily outpatients with eczema (p < 0.001).
Distributed lag nonlinear models for the daily number of patients
When controlling the temperature factor included in the model as a covariate, i.e., after adjusting for the effects of temperature on air pollution factors, a 5-day lag (lag 0–lag 5) model showing the effect of each air pollution factor on the number of patients per day was used. Lag 0 represents the current day, and lag 5 represents the five previous days. Tables 2 and 3 show the RR and 95% CI values that indicated the effect of a 10-µg/m3 increase in air pollution factors and climate factors on the number of patients per day.
After adjusting for temperature, with an increase in PM10 values of 10 µg/m3, the numbers of daily outpatients on the previous day (lag 1) and on the five previous days (lag 5) increased 0.19% and 0.27%, respectively. A 10-µg/m3 increase in SO2 values did not have a statistically significant effect on the daily number of patients. With a 10% increase in relative humidity, the numbers of outpatients on the previous day and two days lag increased by 10.29% and 8.38%, respectively. With a 1-hbar increase in pressure values, the numbers of outpatients on the previous day and five previous days increased by 1.71% and 3.44%, respectively, but the number of outpatients on the three previous days decreased by 1.63%. Moreover, when the effect of temperature factors on the number of patients was examined without correction according to any environmental factors, a 1 °C increase in temperature showed a 4.04% decrease in the number of outpatients on the previous day; however, the number of outpatients increased by 3.59%.
Models created with each air pollution factor after adjusting for all meteorological factors over the total 5 days lag
Table 4 presents the RR and 95% CI values showing the effects of each air pollution factor on the number of daily outpatient visits for a total of five days lag, after adjusting for temperature or all meteorological factors. After adjusting for temperature, increases in PM10 levels and SO2 values of 10-µg/m3 resulted in 0.87% and 7.65% increases in the number of daily outpatient visits, respectively. After adjusting for all meteorological factors, a 10-µg/m3 increase in PM10 and SO2 values resulted in 0.93% and 3.97% increases in the number of outpatient visits, respectively.
In Fig. 1, a three-dimensional plot illustrates the effects of temperature and PM10 on the RR of eczema with a maximum 30 lag days (lag 30). A nonlinear polynomial relationship was observed between PM10 and RR, as was a polynomial increase in the RR value with increasing PM10.
After adjusting for temperature and SO2 values, the effect of a 10-µg/m3 increase in PM10 values on the number of daily outpatient visits was statistically significant over a total delay of five days. Moreover, after adjusting for temperature and PM10 values, the effect of a 10-µg/m3 increase in SO2 values on the daily number of outpatient visits was statistically significant, with a 5.34% increase in outpatient visits.
Models with two air pollution factors after adjusting for all meteorological factors over a total delay of 5 days
After adjusting for all meteorological factors and SO2 values, it was determined that a 10-µg/m3 increase in PM10 resulted in a 0.91% increase in the number of eczema-related outpatient visits over a total delay of five days. However, after adjusting for all meteorological factors and PM10 values, a 10-µg/m3 increase in SO2 values did not have a significant effect on the number of daily outpatient visits.
Discussion
In this study, relationships between environmental factors such as air pollutants, relative humidity, temperature, barometric pressure, and eczema-related outpatient visits were investigated using a DLNM. The skin is the outermost barrier in direct contact with various air pollutants. Prolonged and recurrent exposure to environmental stressors causes the development of various skin diseases and skin barrier function disruption when the normal defense potential of skin is exceeded [23].
Data from our study showed a 10% increase in the relative humidity value. Moreover, a 1-hbar increase in the pressure value was found to increase the daily number of outpatient visits when the temperature factor was controlled according to meteorological values. Our results showed that a 1 °C increase in temperature without correction for any environmental factors resulted in a decrease in the number of daily outpatient visits. There have been conflicting reports concerning the effect of relative humidity on eczema lesions. Suárez‐Varela et al. reported that as relative humidity levels increased, eczema lesions increased [26]. Silverberg et al. [25] and Li et al. [18] reported that as relative humidity levels increased, the frequency of visits decreased. Kantor et al. reported that indoor humidity reduced the prevalence of atopic dermatitis; however, the effect of outdoor humidity on the prevalence of atopic eczema remains controversial [13]. The results of our study support those of Suárez‐Varela et al. [26] Li et al. [18] and Goad et al. [7], showing that increased relative humidity and increased temperatures reduced the density of PM in the air. As air pressure values increase, PM concentrations in the air may increase, leading to an increase in hospital admissions owing to skin dryness, which is a characteristic clinical finding of eczema [7, 18]. The results of our study are consistent with those of previous studies that have shown that an increase in air pressure increased the frequency of hospital admissions. Furthermore, low air temperature negatively affects skin barrier functions and increases the risk of dermatitis [4]. In Northern European countries during late autumn–winter and early spring periods when temperature values are low, two studies have reported an increase in the frequency of patients with atopic eczema attending the outpatient clinic [9, 20]. In a study conducted involving 91,642 patients aged 0–17 years in the United States, an inverse relationship between air temperature and the number of patients presenting to the outpatient clinic for atopic eczema was reported [25]. A higher prevalence of irritant and allergic contact dermatitis was found in northern parts of Norway than that reported in a similar survey from southern Sweden. The high incidence of hand eczema was thought to be related to cold climatic conditions [14].
After adjusting for all meteorological factors, and when there was a 10-µg/m3 increase in PM10 and SO2 values in each model, relative humidity, air pressure, and temperature factors were found to change the frequency rate of hospital admissions, with positive effects on the number of daily outpatient visits noted. These results showed that PM10 and SO2 levels, which constitute air pollution components, exacerbate eczema lesions and lead to an increase in the number of hospital admissions. PM10 and SO2 components that cause air pollution differ from each other. SO2 is a highly reactive compound derived from the processing of sulfur-containing substances such as coal and crude oil. PM is a complex mixture of solid and/or liquid droplets suspended in gas. Large PM10 are between 2.5 and 10 µm in diameter, comprising components of soil, dust, and dusty emission from various industries [19]. In recent years, epidemiological studies have reported that environmental air pollution exacerbates many dermatological diseases, especially inflammatory skin diseases such as PM10-related acne [17], dermatitis [15, 16, 21, 29], and psoriasis [22]. High levels of PM10, defined as 20 µq/m3 per year and 50 µq/m3 per day according to the WHO criteria, will increase mortality and morbidity in terms of human health [17]. In this study, a daily increase of 10 µq/m3 led to an increase in PM10 values when all meteorological factors and SO2 were controlled, leading to an increase in the frequency of attendance at the dermatology outpatient clinic due to eczema. Neither meteorological factors nor 10 µq/m3 daily increases in SO2 values when PM10 was controlled for were associated with the frequency of attendance to the outpatient clinic. These results indicated that PM10 values were more important in the development of skin diseases. In different studies, effects of air pollution and climate factors on outpatient visits for eczema in single-factor lag models are shown in Table 5.
One of the most common components of air pollution is PM. One study reported that metals in PM increase the risk of protein and DNA damage and damage in relation to mitochondria-regulated death pathways through apoptosis induction [3]. The skin is an important defense organ that acts as a barrier to the outside world, providing both physical and immunological protection against a variety of microbial, chemical, and physical factors. Therefore, various theories have been proposed to understand the passage of air pollution components through the epidermal barrier. Types of skin penetration include mechanical delivery, an intracellular pathway, a transcellular pathway, and a transfollicular pathway. The skin has numerous pores that are larger than PM in size; however, there is no direct evidence to show that PM can penetrate the skin regardless of its smaller size [15]. Exposure to air pollution-causing particles has an adverse effect on the skin through increasing the level of free radicals, inducing cutaneous inflammation, activating mechanisms linked to the aryl hydrocarbon receptor (causing toxic effects due to air pollution), and altering the skin microflora. All these mechanisms result in increased levels of TNF-α, IL-8, IL-1β, IL-6, and IL-1α in the skin. Increased inflammatory skin diseases have been observed at the end of this entire process [8, 19]. Exposure to environmental air pollution poses health challenges and increases the economic burden in relation to health expenditure.
This study had some limitations. Air pollution exposure was based on estimates. Due to a lack of certainty in terms of geographical addresses, home-specific exposure assessments could not be made. No data were available concerning socioeconomic factors and individual hobbies. The monitoring was restricted due to the number of observations made by the National Air Quality Monitoring Network stations.
Conclusions
The skin is the largest organ of the human body, and any factor affecting the health of the skin can affect the entire body. Our study findings showed that air pollution affects the incidence and prevalence of eczema. An increase in PM10 values was found to be significantly related to the number of outpatient clinic visits, and a temperature increase was found to have a protective effect on patients with eczema. Currently, knowledge concerning the effects of air pollution on skin remains limited. Future cohort studies are required to examine the short- and long-term effects of environmental air pollution on the skin.
References
Ahn K (2014) The role of air pollutants in atopic dermatitis. J Allergy Clin Immunol 134:993–999. https://doi.org/10.1016/j.jaci.2014.09.023
Cai J, Liu W, Hu Y, Shen L, Huang C (2017) Household environment, lifestyle behaviors, and dietary habits in relation to childhood atopic eczema in Shanghai, China. Int Arch Occup Environ Health 90:141–159. https://doi.org/10.1007/s00420-016-1177-8
Choi JH, Kim JS, Kim YC, Kim YS, Chung NH, Cho MH (2004) Comparative study of PM2.5—and PM10—induced oxidative stress in rat lung epithelial cells. J Vet Sci 5:11–18
Engebretsen KA, Johansen JD, Kezic S, Linneberg A, Thyssen JP (2016) The effect of environmental humidity and temperature on skin barrier function and dermatitis. J Eur Acad Dermatol Venereol 30:223–249. https://doi.org/10.1111/jdv.13301
Gasparrini A (2011) Distributed lag linear and non-linear models in R: the package dlnm. J Stat Softw 43:1–20
Gasparrini A (2014) Modeling exposure-lag-response associations with distributed lag non-linear models. Stat Med 33:881–899
Goad N, Gawkrodger DJ (2016) Ambient humidity and the skin: the impact of air humidity in healthy and diseased states. J Eur Acad Dermatol Venereol. 30:1285–1294. https://doi.org/10.1111/jdv.13707
Guo Q, Liang F, Tian L, Schikowski T, Liu W, Pan X (2019) Ambient air pollution and the hospital outpatient visits for eczema and dermatitis in Beijing: a time-stratified case-crossover analysis. Environ Sci Process Impacts 21:163–173. https://doi.org/10.1039/c8em00494c
Hamann CR, Andersen YMF, Engebretsen KA, Skov L, Silverberg JI, Egeberg A, Thyssen JP (2018) The effects of season and weather on healthcare utilization among patients with atopic dermatitis. J Eur Acad Dermatol Venereol 32:1745–1753. https://doi.org/10.1111/jdv.15023
Hassoun Y, James C, Bernstein DI (2019) The effects of air pollution on the development of atopic disease. Clin Rev Allergy Immunol. 57:403–414. https://doi.org/10.1007/s12016-019-08730-3
https://www.stateofglobalair.org/sites/default/files/soga_2019_report.pdf. Accessed 2019
https://www.mgm.gov.tr/iklim=DUZCE. Accessed 2020
Kantor R, Silverberg JI (2017) Environmental risk factors and their role in the management of atopic dermatitis. Expert Rev Clin Immunol 13:15–26. https://doi.org/10.1080/1744666X.2016.1212660
Kavli G, Førde OH (1984) Hand dermatoses in Tromsø. Contact Dermatitis 10:174–177. https://doi.org/10.1111/j.1600-0536.1984.tb00027.x
Kim KE, Cho D, Park HJ (2016) Air pollution and skin diseases: adverse effects of airborne particulate matter on various skin diseases. Life Sci 152:126–134. https://doi.org/10.1016/j.lfs.2016.03.039
Krämer U, Sugiri D, Ranft U, Krutmann J, von Berg A, Berdel D, Behrendt H, Kuhlbusch T, Hochadel M, Wichmann HE, Heinrich J GINIplus, and LISA plus study groups (2009) Eczema, respiratory allergies, and traffic-related air pollution in birth cohorts from small-town areas. J Dermatol Sci 56:99–105. https://doi.org/10.1016/j.jdermsci.2009.07.014
Krutmann J, Moyal D, Liu W, Kandahari S, Lee GS, Nopadon N, Xiang LF, Seité S (2017) Pollution and acne: is there a link? Clin Cosmet Investig Dermatol 10:199–204. https://doi.org/10.2147/CCID.S131323
Li A, Fan L, Xie L, Ren Y, Li L (2018) Associations between air pollution, climate factors and outpatient visits for eczema in West China Hospital, Chengdu, south-western China: a time series analysis. J Eur Acad Dermatol Venereol 32:486–494. https://doi.org/10.1111/jdv.14730
Mancebo SE, Wang SQ (2015) Recognizing the impact of ambient air pollution on skin health. J Eur Acad Dermatology Venereol 29:2326–2332. https://doi.org/10.1111/jdv.13250
Mohn CH, Blix HS, Halvorsen JA, Nafstad P, Valberg M, Lagerløv P (2018) Incidence trends of atopic dermatitis in infancy and early childhood in a Nationwide Prescription Registry Study in Norway. JAMA Netw Open 1:e184145. https://doi.org/10.1001/jamanetworkopen.2018.4145
Morgenstern V, Zutavern CJ, Brockow I, Koletzko S, Krämer U, Behrendt H, Herbarth O, von Berg A, Bauer CP, Wichmann HE, Heinrich J, GINI Study Group; LISA Study Group (2008) Atopic diseases, allergic sensitization, and exposure to traffic-related air pollution in children. Am J Respir Crit Care Med 177:1331–1337. https://doi.org/10.1164/rccm.200701-036OC
Ngoc LTN, Park D, Lee Y, Lee YC (2017) Systematic review and meta-analysis of human skin diseases due to particulate matter. Int J Environ Res Public Health 14:1458. https://doi.org/10.3390/ijerph14121458
Puri P, Nandar SK, Kathuria S, Ramesh V (2017) Effects of air pollution on the skin: a review. Indian J Dermatol Venereol Leprol 83:415–423. https://doi.org/10.4103/0378-6323.199579
Raaschou-Nielsen O et al (2013) Air pollution and lung cancer incidence in 17 European cohorts: prospective analyses from the European Study of Cohorts for Air Pollution Effects (ESCAPE). Lancet Oncol 14:813–822. https://doi.org/10.1016/S1470-2045(13)70279-1
Silverberg JI, Hanifin J, Simpson EL (2013) Climatic factors are associated with childhood eczema prevalence in the United States. J Invest Dermatol 133:1752–1759. https://doi.org/10.1038/jid.2013.19
Suárez-Varela MM, García-Marcos Alvarez L, Kogan MD, González AL, Gimeno AM, Aguinaga Ontoso I, Díaz CG, Pena AA, Aurrecoechea BD, Monge RM, Quiros AB, Garrido JB, Canflanca IM, Varela AL (2008) Climate and prevalence of atopic eczema in 6- to 7-year-old school children in Spain. ISAAC phase III. Int J Biometeorol 52:833–840. https://doi.org/10.1007/s00484-008-0177-0
Yıldız GP, Güleç BE, Elverişli MF, Erçelik M, Arbak P (2019) Do the levels of particulate matters less than 10 μm and seasons affect sleep? Aging Male 23:1–6. https://doi.org/10.1080/13685538.2019.1655637
Yıldız GP, Güleç BE, Annakkaya AN, Balbay OA (2019) The effect of natural gas warming on emergency applications due to respiratory tract diseases in children in Düzce Province. Fresenius Environ Bull 28:6153–6160
Zhou C, Baïz N, Banerjee S, Charpin DA, Caillaud D, de Blay F, Raherison C, Lavaud F, Annesi-Maesano I (2013) The relationships between ambient air pollutants and childhood asthma and eczema are modified by emotion and conduct problems. Ann Epidemiol 23:773–788. https://doi.org/10.1016/j.annepidem.2013.09.004
Funding
None declared.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interests pertinent to this study. There are no conflict of interests to be declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Karagün, E., Yıldız, P. & Cangür, Ş. Effects of climate and air pollution factors on outpatient visits for eczema: a time series analysis. Arch Dermatol Res 313, 49–55 (2021). https://doi.org/10.1007/s00403-020-02115-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-020-02115-9