Abstract
Physicians’ and patients’ perspectives can vary significantly. For a long time, physicians considered psoriasis a non-pruritic dermatosis until a survey found pruritus to be the most bothersome symptom among psoriasis patients. In our study, we wanted to get an insight into the factors that affect patients and evaluate whether gender differences exist. A link of an anonymous online survey (www.fightpsoriasis.ch) with 24 questions was placed on the website of the Swiss Psoriasis and Vitiligo Patient Association (www.spvg.ch) from May 2016 until June 2017. 3164 persons participated in this online survey, of which 1979 were diagnosed with psoriasis. Significantly more females than males were affected by psoriatic pruritus [713 (36%) vs. 500 (25.3%), p ≤ 0.001] and 756 (39.7%) of all patients identified pruritus as the most life quality-limiting factor. Fewer women reported high satisfaction with their therapy compared to men [96 (4.9%) vs. 110 (5.6%), p ≤ 0.015]. Pruritus remains the most bothersome symptom and women were more often affected by it, leading to a lower treatment satisfaction among female patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psoriasis is a chronic inflammatory disease with a significant negative impact on the physical and psychological well-being of patients [2, 5].
Physicians’ and patients’ perspectives can vary significantly. For instance, pruritus in psoriasis has been traditionally neglected by physicians, but more than 60% of patients report pruritus, especially females [3]. Even though for physicians, the visible appearance of psoriasis plaques may seem to be the single most quality of life (QoL)-limiting factor, large surveys revealed this to be incorrect. In fact, patients reported that pruritus was the most bothersome symptom [9].
Another assumption, namely that women and men are affected by psoriasis in the same way, has also been proven wrong. In recent years, gender differences have become an increasingly relevant topic in health care. It has been shown that they exist not only in the perception of the disease and its symptoms, but also in treatment outcomes [11, 13]. Although the prevalence and incidence of psoriasis seem to be identical between men and women, some differences have been reported in psoriasis with regard to response and satisfaction with biological treatment [7, 8, 14].
We felt that an anonymous online survey would be the best method for patients to feel comfortable, open up, share their insights and take part in this survey. Using an online questionnaire is, in our opinion, also the most efficient way to reach patients in all of Switzerland and beyond.
The aim of our study was to gain more information about the quality of medical care, patients’ perspective regarding quality of life (QoL) as well as factors that contribute to it with a special focus on gender differences.
Methods
Patient recruitment and survey
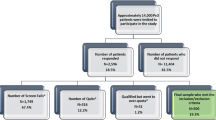
A link of an anonymous online survey (www.fightpsoriasis.ch) was placed on the website of the Swiss Psoriasis and Vitiligo Patient Association (www.spvg.ch) from May 2016 until June 2017. Adult psoriasis patients (≥ 18 years of age) were targeted and their personal experiences were shared anonymously without the involvement of health-care professionals. Due to the anonymity of the online survey, the study was exempt from ethical review according to Swiss law. The survey included a set of 24 questions (Table 1). 3164 patients participated in the study. Those who were not diagnosed with psoriasis were excluded and the data of 1979 participants were analyzed (Fig. 1).
Statistical data analysis
Descriptive analyses were performed using standard statistical parameters. For calculation of relative frequencies, only data sets of participants with answers to the specific questions were evaluated. Specific results were stratified by sex. For comparisons, the Chi-squared test and the Fisher’s exact test were used. Statistical analysis was performed using R software.
Results
A total of 3164 persons participated in this online survey, of which 1979 were diagnosed with psoriasis. 1067 (53.9%) women and 910 (46.0%) men were included. Most patients were between 50 and 75 years of age. Participants above 75 years made up the smallest age group, including only 85 (4.3%) patients (Table 2).
The majority of all patients (960, 48.5%) reported that their disease covered an area of less than three palms in size. Many patients (741, 37.4%) stated that psoriatic skin involvement accounted for an area of three to ten palms. In only 192 (9.7%), the body surface area involved more than ten palms. No gender differences were found.
The scalp was involved in 1305 (65.9%), the nails in 765 (38.7%), the palms and/or soles in 712 (36.0%) and the intertriginous regions (genitals and/or arm pits) in 714 (36.1%) of all survey participants. Nail involvement (20.9% in male vs. 17.7% in female, p ≤ 0.001) and involvement of the intertriginous regions (19.2% in male vs. 16.8% in female, p ≤ 0.001) were significantly more prominent in male respondents. There were no significant gender differences regarding scalp involvement and psoriatic manifestation on palms and/or soles (Table 3).
Significantly more women were affected from joint pain [609 (30.8%) vs. 408 (20.6%), p ≤ 0.001], swollen joints [374 (18.9%) vs. 224 (11.3%), p ≤ 0.01], morning stiffness [275 (13.9%) vs. 156 (7.9%), p ≤ 0.01] and heel pain [275 (13.9%) vs. 156 (7.9%), p ≤ 0.01]. There was no significant gender difference regarding swelling of fingers or toes (Table 4).
1453 (73.4%) participants had received the diagnosis “psoriasis” by a dermatologist, 568 (28.7%) by a general practitioner and 158 (8%) by a rheumatologist.
1157 (58.5%) reported to have a reduced quality of life due to psoriasis. 1213 (61.3%) of all participants indicated pruritus due to their psoriatic lesions, independent of age. Significantly more females than males were affected by psoriatic pruritus [713 (36%) vs. 500 (25.3%), p ≤ 0.001] Overall, 756 (39.7%) of all patients identified pruritus as the most life quality-limiting factor. A significant negative association was found between pruritus and reported quality of life (p ≤ 0.001).
918 (46.4%) reported that they do not undergo treatment and significantly less women reported high satisfaction with their therapy compared to men [96 (4.9%) vs. 110 (5.6%), p ≤ 0.015]. 414 (20.9%) female and 310 (15.7%) male patients were not or not entirely satisfied with their treatments. 627 (31.7%) patients reported that they were “not always” or “not at all” satisfied with the handling of their therapy. 538 (27.2%) patients were “not always” or “not at all” satisfied with the time effort for their therapy. 806 (40.7%) stated that they “always” or “mostly” applied their treatment as recommended by their physician.
Of all participants, 392 (19.8%) stated that they had seen their treating physician within the last month, 275 (13.9%) within the last 3 months, 200 (10.1%) within the last 6 months, 176 (8.9%) within the last 12 months, and 564 (28.5%) had not seen their doctor for over a year. 16 (0.8%) had not seen their physician since they received the diagnosis of psoriasis and no data were obtained in 356 (18%) patients.
Discussion
Before this study, we assumed that in the majority of cases, general practitioners would make the diagnosis of psoriasis due to the high amount of dermatologic patients they see [4]. Yet, most patients reported that their psoriasis was diagnosed by a dermatologist. This underlines the importance of dermatologists identifying psoriasis patients. A possible reason for the low rate of rheumatologists making the first diagnosis might be that they see patients only after skin symptoms have developed already, as psoriatic arthritis is not usually the first manifestation of psoriasis. Also, in many cases psoriatic skin lesions are significantly easier to detect and diagnose than psoriatic arthritis (even with proper rheumatologic examination and sonography or X-ray).
A German study has shown higher prevalence of nail psoriasis in men than in women [1], which corresponds with our findings. Due to the higher proportion of men having a job where they use their hands, the phenomenon of Koebner could trigger nail psoriasis. Unfortunately, we do not have an explanation for this. On the other hand, this data comes as a surprise, even more so since nail involvement can be associated with psoriatic arthritis. While current epidemiological data report no differences in incidence and prevalence of psoriasis arthritis between women and men [12], in our study women had significantly more often symptoms like joint pain, swollen joints, morning stiffness and heel pain.
It is of interest that fewer women showed high treatment satisfaction compared to men. Van der Schoot et al. have shown that female psoriasis patients under biological treatment had a lower treatment satisfaction and more side effects compared to men [14]. A possible explanation for this might be the difference in gender-specific treatment goals, as reported by Maul et al. [10]. Another explanation is the fact that women are reported to suffer more prominently from pruritus [3]. While itchiness as a symptom of psoriasis has been underrecognized and psoriasis has even been considered a non-pruritic dermatosis, growing evidence has shown that pruritus is one of the most prevalent and burdensome symptoms of psoriasis [6]. In our study, around two-thirds of respondents reported to suffer from pruritus due to their psoriasis and pruritus was found to be the most frequently reported limitation in daily life. Lebwohl et al. [9] found that about 40% of all patients indicated that pruritus was the most limiting factor in their lives. This number corresponds very well with the data we have obtained (39.7%). Due to this high number, an important measure of therapeutic success should be the reduction of pruritus.
Despite many new, and highly effective treatment options, the number of patients who stated that they continued to suffer from psoriasis was surprisingly high. More than half of all patients reported to have a reduced quality of life, leading to the assumption that many patients might be undertreated. Even though doctors, pharmaceutical companies and patient organizations have made a great effort to inform patients about new treatment options, we assume that a large number of patients are not sufficiently well informed about treatment modalities and possibilities.
The most important limitations of our study include that patients younger than 18 years were excluded and that the validity of statements could not be verified. The exact age has not been obtained, which would have added interesting information.
Our study gives physicians an insight, where the current shortcomings in our patient management may exist. Taken together, our study has found significant differences in psoriasis features and disease burden between men and women. It has confirmed pruritus as the most important quality of life-limiting factor that needs a special focus. Overall, many psoriasis patients have not seen their physician within the last year (possibly even longer) and, though effective treatment options exist, patients might not have been adequately advised about them and might benefit from more information.
References:s
Augustin M, Reich K, Blome C, Schafer I, Laass A, Radtke MA (2010) Nail psoriasis in Germany: epidemiology and burden of disease. Br J Dermatol 163(3):580–585
Augustin M, Reich K, Glaeske G, Schaefer I, Radtke M (2010) Co-morbidity and age-related prevalence of psoriasis: analysis of health insurance data in Germany. Acta Derm Venereol 90(2):147–151
Bahali AG, Onsun N, Su O, Ozkaya DB, Dizman D, Topukcu B et al (2017) The relationship between pruritus and clinical variables in patients with psoriasis. An Bras Dermatol 92(4):470–473
Basarab T, Munn SE, Jones RR (1996) Diagnostic accuracy and appropriateness of general practitioner referrals to a dermatology out-patient clinic. Br J Dermatol 135(1):70–73
Drach M, Papageorgiou K, Maul JT, Djamei V, Yawalkar N, Hausermann P et al (2019) Effectiveness of methotrexate in moderate to severe psoriasis patients: real-world registry data from the Swiss Dermatology Network for Targeted Therapies (SDNTT). Arch Dermatol Res 311(10):753–760
Elewski B, Alexis AF, Lebwohl M, Stein Gold L, Pariser D, Del Rosso J et al (2019) Itch: an under-recognized problem in psoriasis. J Eur Acad Dermatol Venereol 33(8):1465–1476
Hagg D, Eriksson M, Sundstrom A, Schmitt-Egenolf M (2013) The higher proportion of men with psoriasis treated with biologics may be explained by more severe disease in men. PLoS ONE 8(5):e63619
Hotard RS, Feldman SR, Fleischer AB Jr (2000) Sex-specific differences in the treatment of severe psoriasis. J Am Acad Dermatol 42(4):620–623
Lebwohl MG, Bachelez H, Barker J, Girolomoni G, Kavanaugh A, Langley RG et al (2014) Patient perspectives in the management of psoriasis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis Survey. J Am Acad Dermatol. 70(5):871–881e1-30
Maul JT, Navarini AA, Sommer R, Anzengruber F, Sorbe C, Mrowietz U et al (2019) Gender and age significantly determine patient needs and treatment goals in psoriasis—a lesson for practice. J Eur Acad Dermatol Venereol 33(4):700–708
Regitz-Zagrosek V (2012) Sex and gender differences in health. Science & Society series on sex and science. EMBO Rep 13(7):596–603
Ritchlin CT, Colbert RA, Gladman DD (2017) Psoriatic Arthritis. N Engl J Med 376(21):2095–2096
Teunissen TAM, Rotink ME, Lagro-Janssen ALM (2016) Gender differences in quality of care experiences during hospital stay: a contribution to patient-centered healthcare for both men and women. Patient Educ Couns 99(4):631–637
van der Schoot LS, van den Reek J, Groenewoud JMM, Otero ME, Njoo MD, Ossenkoppele PM et al (2019) Female patients are less satisfied with biological treatment for psoriasis and experience more side-effects than male patients: results from the prospective BioCAPTURE registry. J Eur Acad Dermatol Venereol 33(10):1913–1920
Funding
The survey and the statistical analysis were funded by Celgene Inc. (now Amgen). The company did not have any influence on the content of the manuscript. No writing assistance was used for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C.M. reports no conflict of interest. D.S. is a former employee of Celgene Inc., but has no conflict of interest. S.M has no conflict of interest. C.G has no conflicts of interest. J-T. M. is an employee of USZ and received a “filling the GAP” stipend. V.D. has honoraria from AbbVie, Celgene, Eli Lilly, Leo Pharma, Novartis and Sanofi. A. A. N was funded by the Promedica and Bruno-Bloch Foundation, as well as Hochspezialisierte Medizin 2 of the Kanton Zürich, Switzerland. He is also on the advisory board of AbbVie, Pfizer, Novartis, Celgene, MSD and Galderma and has received grants from AbbVie, Novartis, Celgene and others. F.A. has received honoraria from Abbvie, Celgene, Leo Pharma, Galderma, Eli Lilly, Janssen-Cilag, Novartis, Galderma and Almirall, but has no financial interest, nor holds any shares of any pharmaceutical company.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Murer, C., Sgier, D., Mettler, S.K. et al. Gender differences in psoriasis: a Swiss online psoriasis survey. Arch Dermatol Res 313, 89–94 (2021). https://doi.org/10.1007/s00403-020-02066-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-020-02066-1