Abstract
Previous studies have explored the relationship of PTPN22 and TLR9 polymorphisms with systemic lupus erythematosus (SLE). In consideration of the population stratification, conflicting results and updating data, we conducted a comprehensive meta-analysis, which consists of a total of 17 research articles (9120 cases and 11,724 controls) for PTPN22 and 20 articles (including up to 2808 cases and 3386 controls) for TLR9. Significant association was verified between PTPN22 rs2476601 and SLE in the overall population (OR = 1.511 per T allele, 95% CI 1.338–1.706, P = 2.931 × 10−11) and under dominant model of T allele (TT+CT vs. CC: OR = 1.531, 95% CI 1.346–1.742, P = 9.17 × 10−11). Analysis after stratification by ethnicity indicated that PTPN22 rs2476601 was related to SLE in Americans (OR = 2.566, 95% CI 1.796–3.665, P = 2.219 × 10−7), Europeans (OR = 1.399, 95% CI 1.261–1.552, P = 2.153 × 10−10), and Africans (OR = 4.14, 95% CI 1.753–9.775, P = 1.0 × 10−3). We did not observe any association between TLR9 polymorphisms (rs187084, rs352140, rs5743836 and rs352139) and SLE under any model, after excluding the data that were inconsistent with Hardy–Weinberg equilibrium (HWE). In summary, PTPN22 rs2476601 was significantly interrelated with SLE and contributed to susceptibility and development of SLE in Americans, Europeans and Africans in this analysis, while their relationship needs to be validated in Africans by future research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is an autoimmune disease typically characterized by the generation of multiple autoantibodies to nuclear antigens, and by complement activation and immune complex deposition, which results in diverse clinical manifestation and the involvement of multisystem [85]. It has been confirmed that genetic and environmental factors play important role in the development of SLE [27, 34, 85]. The morbidity rate of SLE is diversiform in different populations [39], with 31–70/100,000 in Chinese [88], and 7–71/100,000 in European [12] and up to 200/100,000 in African populations [12]. Although, abundant studies have been carried out, the etiology and pathogenesis of SLE have not been clearly illustrated. Genome-wide linkage studies have evidenced susceptibility area in SLE, such as 1q23 [80], 4p16-15.2 [24], 11p13 [53], 11q14 [73], 12q24 [54], 16p13 [90] and 16q12 [80], and dozens of valuable susceptible genes have been found, such as IKBKE [72], IL8 [72], MAMDC1 [28], PTPN22 [78], STAT4 [62], FCGR2B [95], FCGR3B [95] and TLR5 [70]. Recently, genome-wide association studies (GWAS) have provided more clues for the studies of complex diseases, which assisted us in discovering the susceptibility genes and SNPs for SLE [26, 49, 56, 86].
PTPN22 (protein tyrosine phosphatase non-receptor 22) gene locates on chromosome 1p13.3-p13.1 and encodes lymphoid-specific phosphatase (Lyp) [67]. Lyp is known to participate in antigen receptor signaling and its impact on the immune response and role in the development of autoimmunity have been a focus of current research [67]. Lyp inhibits T cell activation by binding to C-terminal Src tyrosine kinase (Csk). PTPN22 participates in the inhibition of T cell activation, inactivates kinase of T cell receptor and limits to the reaction to the antigen [10]. The mutation of PTPN22 rs2476601 single-nucleotide polymorphism (SNP) could disrupt the physiological interaction between Lyp gene and Csk kinase, and cause signal transduction disorder and reduce the threshold for T cell receptor signaling, leading to the occurrence of autoimmune diseases [11, 82], including SLE, rheumatoid arthritis, type 1 diabetes and autoimmune thyroid disease [9]. To date, the GWAS have reported the association between PTPN22 rs2476601 and autoimmune diseases, such as type 1 diabetes, rheumatoid arthritis, myasthenia gravis and Crohn’s disease [3, 22, 25, 58]. The GWAS have also confirmed the significant association between PTPN22 rs2476601 and SLE in Europeans [6, 49]. Although results from GWAS were sometimes taken as the golden criterion for the association study, conflicting findings still existed in different studies, which might have resulted from greater variability of allele frequencies in different populations.
Toll-like receptor (TLR) family is a transmembrane pattern recognition receptor, which plays an important part in the activation and regulation of both innate and adaptive immune response. TLR9 is a kind of specific receptor, which can recognize cytosine phosphate guanosine (CpG) located in bacterial DNA [29]. The aberrant activation of TLR9 may lead to the production of type 1 interferon, which has been closely related to SLE pathophysiology [27]. Study has confirmed that TLR9 plays an important role in the generation and development of SLE by combining with the CpG motif [37].
Migita et al. [47] showed that TLR9 expression in lymphocytes was increased in patients with SLE. However, Hur et al. [33] observed that four polymorphisms within a 4334-bp segment of the TLR9 gene demonstrated no significant association with susceptibility to SLE in a Korean population. De Jager et al. [13] examined a much larger 68,742-bp segment that contains the entire TLR9 gene and 60 kb of flanking sequence, and no evidence of association was found.
Although a large number of studies have investigated the associations between PTPN22 SNPs (rs2476601), TLR9 SNPs (rs187084, rs352140, rs5743836, rs352139) and SLE risk, the results were inadequate or discordant. To check the association in different ethnics, we performed a comprehensive ethnicity-specific meta-analysis to illuminate the association of PTPN22 and TLR9 with SLE susceptibility by enhancing statistical power. We also tried to find the best-fit association model among the dominant, recessive and additive models for the polymorphisms.
Methods
Identification of eligible studies
A comprehensive literature research was conducted by the PubMed databases (National Center for Biotechnology, National Library of Medicine), CNKI (Chinese National Knowledge Infrastructure) and Wanfang databases (Wanfang Data Knowledge Service Platform) for the association between PTPN22 or TLR9 polymorphisms with SLE before December 2016, with the following key words: ‘The protein tyrosine phosphatase non-receptor 22’, ‘PTPN22’, ‘Toll-like receptor 9’, ‘TLR9’, ‘polymorphism’, ‘Systemic lupus erythematosus’ and ‘SLE’.
Inclusion and exclusion criteria
The included study should satisfy the following criteria: (1) case–control study; (2) providing raw data, from which the odds ratio (OR) and 95% confidence interval (CI) could be calculated; (3) all patients should fulfil the American College of Rheumatology (ACR) criteria [31]. Exclusion criteria were as follows: (1) data from conference or meeting abstracts; (2) family-based study; (3) study without genotype distributions.
Data extraction
The following information is extracted from each study: journal, first author, year of publication, ethnicity, the sample size, genotype distributions and the allele frequency of cases and controls. We calculated the number of genotype by allele frequency with Hardy–Weinberg equilibrium (HWE) law, when the data was insufficient in the articles.
Statistical analyses
We calculated the Hardy–Weinberg equilibrium (HWE) of control group separately in each of the study, and we considered that the study population did not conform to HWE when the P value for HWE <0.05. Allele frequencies of PTPN22 and TLR9 polymorphisms from each study were determined by allele counting. OR and 95% CIs were calculated to evaluate the association between PTPN22 SNP or TLR9 SNPs and SLE; meanwhile, Cochran’s Q-statistic was used to estimate the effect of variations and heterogeneities [30]. If a significant Q-statistic indicated heterogeneity across studies (P < 0.10), then the random effect model was applied to the meta-analysis; otherwise, the fixed effect model was used [15, 30]. The effect of heterogeneity was quantified with the following formula: I 2 = 100% × (Q − df)/Q [30]. The I 2 value represented the proportion of between-study variability attributable to heterogeneity, and I 2 values of 25, 50 and 75% were considered to be of low, moderate and high heterogeneity, respectively. If study groups showed no heterogeneity, fixed and random effects models produced similar results and, if not, the random effects model usually produced wider CIs than the fixed effects model. Thus, random effects model was applied to this analysis of significant between-study heterogeneity.
The potential publication bias was evaluated using Begg’s linear regression test [4], which measured the funnel plot asymmetry using a natural logarithm scale of ORs. A sensitivity analysis was performed to assess the influence of each study on the total effect. The statistical analysis was carried out using STATA 12.0 (Stata Corporation, College Station, TX, USA).
Results
Studies included in the meta-analysis
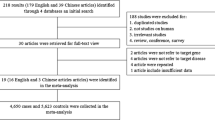
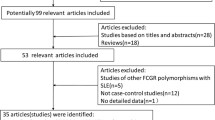
In this meta-analysis, totally 221 relevant articles (68 for PTPN22 and 153 for TLR9) were found. After reading titles and abstracts, we selected 66 articles (36 for PTPN22 and 30 for TLR9) for further reading. Then, we excluded 29 articles (19 for PTPN22 and 10 for TLR9), because of no data, insufficient data, repeated date, family-based studies, not referring to SLE or reviews. Thus, 37 articles (17 for PTPN22 and 20 for TLR9) met the study inclusion criteria [1, 2, 14, 16, 18,19,20,21, 23, 32, 33, 35, 38, 45, 46, 48, 52, 55, 57, 59,60,61, 63,64,65,66, 68, 69, 74, 76, 77, 79, 82, 84, 89, 93, 94]. The flowchart of selecting article process is presented in Fig. 1. Totally, there were 9349 cases and 12,390 controls to evaluate the relationship between PTPN22 rs2476601 and SLE. For TLR9, there were 2927 cases and 3509 controls for rs187084, 2834 cases and 3398 controls for rs352140, 2317 cases and 3291 controls for rs5743836 and 2090 cases and 2390 controls for rs352139, respectively. The basic information of these included studies is shown in Table 1a, b.
Lastly, after excluding two groups of data in which the control populations deviated from HWE, 17 publications providing 9120 cases and 11,724 controls were pooled to evaluate the relationship between PTPN22 rs2476601 and SLE in the meta-analysis (Table 1a) [35]. Similarly, for TLR9 rs187084, rs352140, rs5743836 and rs352139, after exclusion of the studies of nonconformity with HWE, there were 2760 cases and 3298 controls, 2808 cases and 3386 controls, 1640 cases and 2282 controls and 1978 cases and 2290 controls (Table 1b), respectively.
Meta-analysis results
PTPN22 rs2476601 polymorphism and SLE risk
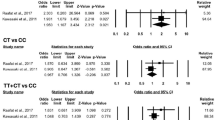
17 relevant studies including 9120 cases and 11,724 controls were analyzed in this meta-analysis after excluding two separate comparisons [35] of nonconformity with HWE. An outstanding association was found in the overall population, under the random effect model (T vs. C: OR = 1.511, 95% CI 1.338–1.706, P = 2.931 × 10−11, Table 2; Fig. 2a). Ethnicity-specific meta-analysis indicated significant association between rs2476601 and SLE in American and European populations (T vs. C: OR = 2.566, 95% CI 1.796–3.665, P = 2.219 × 10−7; OR = 1.399, 95% CI 1.261–1.552, P = 2.153 × 10−10, Table 2; Fig. 2d). We also identified an association between this polymorphism and SLE in Africans (T vs. C: OR = 4.14, 95% CI 1.753–9.775, P = 0.001, Table 2; Fig. 2d). However, no significant association was found between rs2476601 and SLE in Asians (T vs. C: OR = 1.323, 95% CI 0.550–3.181, P = 0.532, Table 2; Fig. 2d).
Accordingly, we used the dominant and recessive models to estimate the relationship between PTPN22 rs2476601 and SLE risk. We observed the association between this polymorphism and SLE in the dominant and recessive model of T allele in the overall population (TT+CT vs. CC: OR = 1.531, 95% CI 1.346–1.742, P = 9.172 × 10−11; TT vs. CT + CC: OR = 2.03, 95% CI 1.519–2.712, P = 1.753 × 10−6, Table 2; Fig. 2b, c). We also performed the stratification analysis by ethnicity of dominant and recessive models; similarly, there was a significant association between rs2476601 and SLE in the dominant model in the American, European and African populations. However, we found no association in the dominant and recessive models in Asians (Table 2; Supplementary Fig S1a, b).
TLR9 polymorphisms and SLE risk
The association between TLR9 rs187084 polymorphism and SLE was conducted in ten independent studies after the exclusion of one study [32] on the discrepancy of HWE. The test of heterogeneity in the overall population was not significant (P = 0.732, I 2 = 0%), suggesting that the fixed effect model could be used. No association between the allele of TLR9 rs187084 and SLE was identified (C vs. T: OR = 0.929, 95% CI 0.860–1.003, P = 0.061, Table 3; Fig. 3a). We tested the dominant and recessive models of C allele in the overall population, but found no significant association in the two models (CC + CT vs. TT: OR = 0.913, 95% CI 0.817–1.019, P = 0.104; CC vs. CT+TT: OR = 0.899, 95% CI 0.776–1.042, P = 0.158, Table 3; Supplementary Fig S2a, b).
Similarly, we analyzed the cases and controls of TLR9 rs352140, rs5743836 and rs352139 to assess their association with SLE, after performing the HWE test and heterogeneity test. However, no association was found between rs352140, rs5743836, rs352139 and SLE susceptibility (Table 3; Fig. 3b–d). Furthermore, we analyzed the dominant and recessive models, respectively, which indicated that no statistically significant association was discovered in all of the dominant and recessive models (Table 3; Supplementary Figs S3a, b, S4a, b, S5a, b).
Allele frequency of the five SNPs and comparison to the 1000 Genomes Phase 3 population
We displayed the allele frequencies in different ethnicities in our meta-analysis and 1000 genomes of the five SNPs in Table 4. In view of the sample size and population, the allele frequencies of PTPN22 rs2476601, TLR9 rs187084 and TLR9 rs352139 in this meta-analysis were consistent with the allele frequencies in the 1000 Genome Project AMR (Admixed American), EUR (European ancestry), AFR (African ancestry), EAS (East Asian ancestry), respectively, however, there was distinction between the allele frequencies of TLR9 rs352140, TLR9 rs5743836 and 1000 Genomes Project (Table 4).
Publication bias and sensitivity analysis
Begg’s funnel plot was used to evaluate the publication bias. There was no obvious evidence of symmetry from the shapes of the funnel plots (Fig. 4a–e) and no evidence of publication bias of all study subjects (P > 0.05). Accordingly, we performed sensitivity analysis to assess the influence of individual study on the pooled OR. The analysis showed that no individual study significantly affected the pooled OR; therefore, no study was deleted (Fig. 5a–e).
Begg’s funnel plot of publication bias in the meta-analysis of the association of PTPN22 and TLR9 polymorphisms with SLE risk under allele genetic model. a PTPN22 rs2476601 and SLE (T vs. C), b TLR9 rs187084 and SLE (C vs.T), c TLR9 rs352140 and SLE (T vs. C), d TLR9 rs5743836 and SLE (C vs. T) and e TLR9 rs352139 and SLE (G vs. A)
Discussion
In this study, we conducted a meta-analysis of the association between PTPN22 rs2476601 and TLR9 polymorphisms with SLE susceptibility. We validated that the T allele of PTPN22 rs2476601 apparently increased the risk of SLE, but its effect was diverse in different ethnics. Although we found no significant association between TLR9 polymorphisms and SLE, we summed up and verified previous studies.
SNP rs2476601 is a missense mutation in the PTPN22 gene on chromosome 1p13.3-13.1, which was identified to be associated with multiple autoimmune diseases [10]. In 2004, PTPN22 rs2476601 was first indicated to be associated with type 1 diabetes [7] and rheumatoid arthritis [5]; afterward, studies showed the relevance between PTPN22 and other diseases, such as SLE, myasthenia gravis and Crohn’s disease [17, 38, 81]. Recently, GWAS have discovered significant association between PTPN22 rs2476601 and SLE in Europeans [49]. To check this association in different ethnicities, we carried out a comprehensive ethnicity-specific meta-analysis involving 9120 cases and 11,724 controls with 19 separate comparisons, and found that the association between PTPN22 rs2476601 and SLE achieved genome-wide significance in the overall population and reached significant correlation in the American and European, and a certain relevance in the African, but not in the Asian population. Zheng et al. [92] previously carried out a meta-analysis with 14 case–control studies and testified a significant association between PTPN22 rs2476601 and SLE, acquiring a more significant result than those in our meta-analysis. However, after careful reading, we found that Zheng et al. included a study of rheumatoid arthritis [20] and a study with data deviated from HWE [35]. Papers of this kind were not supposed to pass the inclusion criteria of meta-analysis; we therefore excluded these two studies and included an additional seven newly published studies after Zheng’s meta-analysis. Meta-analysis by Lee et al. [43], Shi et al. [75] and Lea et al. [40] included only 6, 4 and 11 studies, mainly in European, respectively. Our meta-analysis was more comprehensive and more diverse in population.
There were only three studies [19, 35, 48] for the African population included in this meta-analysis (one paper was excluded because of HWE deviation [35]), including only 210 effective cases and 261 controls. However, the effect of the T allele in the African population is in the same direction as that in the overall population. It was easy for us to see that rs2476601 T allele frequency was low in all the populations, and it was monomorphic in the African and Asian populations in the 1000 Genomes Phase 3 (Table 4). We could notice that the T allele was not monomorphic in the two African studies, and the T allele frequency of SLE case from Moez et al. [48] was much higher than that from Elghzaly et al. [19] (0.263 vs 0.029) (Table 1a). Because only 40 SLE cases were included in the study from Moez et al., the frequency was not reliable. Additionally, Sanchez et al. [71] have reported that no association was found between PTPN22 rs2476601 and SLE in African-Americans. These phenomenon and discrepancy needed further investigation on the basis of large sample size.
Previous studies have showed that genotype TT was not detected in the Chinese population [8, 91], similarly, no rs2476601 T allele and structural variant R620W of the PTPN22 protein were found in the Asian population [36, 41]. As shown in the 1000 Genomes Phase 3, the T allele was also not existent in the East Asian population (Table 4). Therefore, theoretically speaking, no association should be detected between rs2476601 and SLE in Asians. Although our result is consistent with the theory, more studies need to evaluate their association.
TLR9 could modulate autoimmunity by inducing inflammatory cells and by the production of cytokines or antibodies [79]. The expression and mRNA level of TLR9 on B cell were up-regulated in SLE patients, and SLE activity index was significantly associated with TLR9 expression [51]. Some studies indicated that TLR9 expression was obviously higher in SLE cases than in healthy controls. Wang et al. [83] performed a meta-analysis of TLR9 polymorphisms and SLE risk, and 21 studies from 19 articles with 10,273 subjects were included in that meta-analysis. The results indicated that TLR9 rs187084 could increase the risk of SLE (T vs. C: OR = 1.15, 95% CI 1.02–1.30, P = 0.020) in Asians with marginal significance and no evidence was found for the association between TLR9 rs352140, rs5743836, rs352139 and SLE risk. Similarly, Lee et al. [42] carried out a meta-analysis and the results showed that only TLR9 rs187084 was associated with SLE risk (OR = 0.869, 95% CI 0.762–0.992, P = 0.038). Although they verified the relativity of SLE and TLR9 rs187084, under the circumstances of P = 0.02 and P = 0.038, we considered the relevance was marginal rather than significant. However, Li et al. and Yang et al. indicated that none of these three polymorphisms (rs187084, rs352139, rs352140) showed any significant association with SLE risk in Asian populations [44, 87].
To precisely explore the association between TLR9 polymorphisms (rs187084, rs352140, rs5743836, rs352139) and SLE, we analyzed the data that were consistent with HWE and used the random effect model to deal with the heterogeneity. Ultimately, 18 articles with 10,690 subjects were analyzed comprehensively. Although TLR9 has been evidenced to be responsible for the maturation of dendritic cells (DCs) and the production of pro-inflammatory cytokines in knockout mice [29], we have no sufficient information to identify the significant relationship between TLR9 and SLE in the study population. Then, we compared our study with the meta-analysis from Wang et al. [83] and found that they included two groups of repeated data [76, 77], which could lead to imprecise results. On comparing our data with that of Lee et al. [42], we found that a study with data deviating from HWE (P < 0.05) was included in Lee et al., and we included one additional newly published study [93] which led to the diversity of results. Simultaneously, we realized that marginal significance was reached under the allele model and dominant model for TLR9 rs187084 if we included the data of nonconformity with HWE in the population (C vs. T: OR = 0.877, 95% CI 0.783–0.982, P = 0.022;CC + CT vs. TT: OR = 0.875, 95% CI 0.787–0.974, P = 0.014, Supplementary Fig S6a and Fig S6b) and in Asians (C vs. T: OR = 0.881 95% CI 0.780–0.996, P = 0.043; CC + CT vs. TT: OR = 0.883, 95% CI 0.791–0.986, P = 0.027, Supplementary Fig S7a, b), which indicated that the association between rs187084 and SLE was suggestive.
Although there were new discoveries revealed by this study, several potential limitations existed. Firstly, we need a large number of data to validate the relationship between PTPN22 and SLE for further study in the African and other populations. For TLR9, most studies included in this meta-analysis were carried out in Asian populations, so we had insufficient data to conduct subgroup meta-analysis. In other words, available data could not confirm the significant association between TLR9 and SLE. Secondly, we had to point out that significant between-study heterogeneity that was detected. We used the random effect model to deal with the heterogeneity, but this might introduce an insensible statistical illusion because fixed effect model and random effect model address different research questions [50]. Despite these deficiencies, we had searched for information and analyzed data as comprehensively as possible.
In conclusion, our meta-analysis indicated that the missense SNP rs2476601 in PTPN22 was significantly associated with SLE susceptibility in the overall population, and the association had reached genome-wide significance. However, the relationship between Africans and Asians needs further investigation. TLR9 polymorphisms rs187084, rs352140, rs5743836 and rs352139 may not be associated with SLE.
References
Aksoy R, Duman T, Keskin O, Duzgun N (2011) No association of PTPN22 R620 W gene polymorphism with rheumatic heart disease and systemic lupus erythematosus. Mol Biol Rep 38:5393–5396
Baca V, Velazquez-Cruz R, Salas-Martinez G, Espinosa-Rosales F, Saldana-Alvarez Y, Orozco L (2006) Association analysis of the PTPN22 gene in childhood-onset systemic lupus erythematosus in Mexican population. Genes Immun 7:693–695
Barrett JC, Clayton DG, Concannon P, Akolkar B, Cooper JD, Erlich HA, Julier C, Morahan G, Nerup J, Nierras C, Plagnol V, Pociot F, Schuilenburg H, Smyth DJ, Stevens H, Todd JA, Walker NM, Rich SS, Type 1 Diabetes Genetics C (2009) Genome-wide association study and meta-analysis find that over 40 loci affect risk of type 1 diabetes. Nat Genet 41:703–707
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Begovich AB, Carlton VE, Honigberg LA, Schrodi SJ, Chokkalingam AP, Alexander HC, Ardlie KG, Huang Q, Smith AM, Spoerke JM, Conn MT, Chang M, Chang SY, Saiki RK, Catanese JJ, Leong DU, Garcia VE, McAllister LB, Jeffery DA, Lee AT, Batliwalla F, Remmers E, Criswell LA, Seldin MF, Kastner DL, Amos CI, Sninsky JJ, Gregersen PK (2004) A missense single-nucleotide polymorphism in a gene encoding a protein tyrosine phosphatase (PTPN22) is associated with rheumatoid arthritis. Am J Hum Genet 75:330–337
Bentham J, Morris DL, Cunninghame Graham DS, Pinder CL, Tombleson P, Behrens TW, Martin J, Fairfax BP, Knight JC, Chen L, Replogle J, Syvanen AC, Ronnblom L, Graham RR, Wither JE, Rioux JD, Alarcon-Riquelme ME, Vyse TJ (2015) Genetic association analyses implicate aberrant regulation of innate and adaptive immunity genes in the pathogenesis of systemic lupus erythematosus. Nat Genet 47:1457–1464
Bottini N, Musumeci L, Alonso A, Rahmouni S, Nika K, Rostamkhani M, MacMurray J, Meloni GF, Lucarelli P, Pellecchia M, Eisenbarth GS, Comings D, Mustelin T (2004) A functional variant of lymphoid tyrosine phosphatase is associated with type I diabetes. Nat Genet 36:337–338
Cheng YL, Song JQ, Maji M, Yu XP, Gao TT (2010) Correlation analysis on PTPN22 gene polymorphism between SLE susceptibility of Chinese Han population in Hubei. Chin J Lepr Skin Disease 26:774–777 (article in Chinese)
Chung SA, Criswell LA (2007) PTPN22: its role in SLE and autoimmunity. Autoimmunity 40:582–590
Cohen S, Dadi H, Shaoul E, Sharfe N, Roifman CM (1999) Cloning and characterization of a lymphoid-specific, inducible human protein tyrosine phosphatase, Lyp. Blood 93:2013–2024
Cui Y, Sheng Y, Zhang X (2013) Genetic susceptibility to SLE: recent progress from GWAS. J Autoimmun 41:25–33
Danchenko N, Satia JA, Anthony MS (2006) Epidemiology of systemic lupus erythematosus: a comparison of worldwide disease burden. Lupus 15:308–318
De Jager PL, Richardson A, Vyse TJ, Rioux JD (2006) Genetic variation in toll-like receptor 9 and susceptibility to systemic lupus erythematosus. Arthritis Rheum 54:1279–1282
Demirci FY, Manzi S, Ramsey-Goldman R, Kenney M, Shaw PS, Dunlop-Thomas CM, Kao AH, Rhew EY, Bontempo F, Kammerer C, Kamboh MI (2007) Association study of toll-like receptor 5 (TLR5) and toll-like receptor 9 (TLR9) polymorphisms in systemic lupus erythematosus. J Rheumatol 34(8):1708–1711
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Devaraju P, Gulati R, Antony PT, Mithun CB, Negi VS (2015) Susceptibility to SLE in South Indian Tamils may be influenced by genetic selection pressure on TLR2 and TLR9 genes. Mol Immunol 64:123–126
Diaz-Gallo LM, Espino-Paisan L, Fransen K, Gomez-Garcia M, van Sommeren S, Cardena C, Rodrigo L, Mendoza JL, Taxonera C, Nieto A, Alcain G, Cueto I, Lopez-Nevot MA, Bottini N, Barclay ML, Crusius JB, van Bodegraven AA, Wijmenga C, Ponsioen CY, Gearry RB, Roberts RL, Weersma RK, Urcelay E, Merriman TR, Alizadeh BZ, Martin J (2011) Differential association of two PTPN22 coding variants with Crohn’s disease and ulcerative colitis. Inflamm Bowel Dis 17:2287–2294
dos Santos BP, Valverde JV, Rohr P, Monticielo OA, Brenol JC, Xavier RM, Chies JA (2012) TLR789 polymorphisms and their associations in systemic lupus erythematosus patients from Southern Brazil. Lupus 21:302–309
Elghzaly AA, Metwally SS, El-Chennawi FA, Elgayaar MA, Mosaad YM, El-Toraby EE, Hegab MM, Ibrahim SM (2015) IRF5, PTPN22, CD28, IL2RA, KIF5A, BLK and TNFAIP3 genes polymorphisms and lupus susceptibility in a cohort from the Egypt Delta; relation to other ethnic groups. Hum Immunol 76:525–531
Eliopoulos E, Zervou MI, Andreou A, Dimopoulou K, Cosmidis N, Voloudakis G, Mysirlaki H, Vazgiourakis V, Sidiropoulos P, Niewold TB, Boumpas DT, Goulielmos GN (2011) Association of the PTPN22 R620W polymorphism with increased risk for SLE in the genetically homogeneous population of Crete. Lupus 20:501–506
Enevold C, Nielsen CH, Jacobsen RS, Hermansen ML, Molbo D, Avlund K, Bendtzen K, Jacobsen S (2014) Single nucleotide polymorphisms in genes encoding toll-like receptors 7, 8 and 9 in Danish patients with systemic lupus erythematosus. Mol Biol Rep 41:5755–5763
Franke A, McGovern DP, Barrett JC, Wang K, Radford-Smith GL, Ahmad T, Lees CW, Balschun T, Lee J, Roberts R, Anderson CA, Bis JC, Bumpstead S, Ellinghaus D, Festen EM et al (2010) Genome-wide meta-analysis increases to 71 the number of confirmed Crohn’s disease susceptibility loci. Nat Genet 42:1118–1125
Gomez LM, Anaya JM, Gonzalez CI, Pineda-Tamayo R, Otero W, Arango A, Martin J (2005) PTPN22 C1858T polymorphism in Colombian patients with autoimmune diseases. Genes Immun 6:628–631
Gray-McGuire C, Moser KL, Gaffney PM, Kelly J, Yu H, Olson JM, Jedrey CM, Jacobs KB, Kimberly RP, Neas BR, Rich SS, Behrens TW, Harley JB (2000) Genome scan of human systemic lupus erythematosus by regression modeling: evidence of linkage and epistasis at 4p16-15.2. Am J Hum Genet 67:1460–1469
Gregersen PK, Kosoy R, Lee AT, Lamb J, Sussman J, McKee D, Simpfendorfer KR, Pirskanen-Matell R, Piehl F, Pan-Hammarstrom Q, Verschuuren JJ, Titulaer MJ, Niks EH, Marx A, Strobel P, Tackenberg B, Pütz M, Maniaol A, Elsais A, Tallaksen C, Harbo HF, Lie BA, Raychaudhuri S, de Bakker PI, Melms A, Garchon HJ, Willcox N, Hammarstrom L, Seldin MF (2012) Risk for myasthenia gravis maps to a (151) Pro–>Ala change in TNIP1 and to human leukocyte antigen-B*08. Ann Neurol 72:927–935
Han JW, Zheng HF, Cui Y, Sun LD, Ye DQ, Hu Z, Xu JH, Cai ZM, Huang W, Zhao GP, Xie HF, Fang H, Lu QJ, Xu JH, Li XP et al (2009) Genome-wide association study in a Chinese Han population identifies nine new susceptibility loci for systemic lupus erythematosus. Nat Genet 41:1234–1237
Harley IT, Kaufman KM, Langefeld CD, Harley JB, Kelly JA (2009) Genetic susceptibility to SLE: new insights from fine mapping and genome-wide association studies. Nat Rev Genet 10:285–290
Hellquist A, Zucchelli M, Lindgren CM, Saarialho-Kere U, Järvinen TM, Koskenmies S, Julkunen H, Onkamo P, Skoog T, Panelius J, Räisänen-Sokolowski A, Hasan T, Widen E, Gunnarson I, Svenungsson E, Padyukov L, Assadi G, Berglind L, Mäkelä V-V, Kivinen K, Wong A, Cunningham Graham DS, Vyse TJ, D’Amato M, Kere J, Idnurm A (2009) Identification of MAMDC1 as a candidate susceptibility gene for systemic lupus erythematosus (SLE). PLoS One 4(12):e8037
Hemmi H, Takeuchi O, Kawai T, Kaisho T, Sato S, Sanjo H, Matsumoto M, Hoshino K, Wagner H, Takeda K, Akira S (2000) A toll-like receptor recognizes bacterial DNA. Nature 408:740–745
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Huang CM, Huang PH, Chen CL, Lin YJ, Tsai CH, Huang WL, Tsai FJ (2012) Association of toll-like receptor 9 gene polymorphism in Chinese patients with systemic lupus erythematosus in Taiwan. Rheumatol Int 32:2105–2109
Hur JW, Shin HD, Park BL, Kim LH, Kim SY, Bae SC (2005) Association study of toll-like receptor 9 gene polymorphism in Korean patients with systemic lupus erythematosus. Tissue Antigens 65:266–270
Jonsen A, Bengtsson AA, Nived O, Truedsson L, Sturfelt G (2007) Gene-environment interactions in the aetiology of systemic lupus erythematosus. Autoimmunity 40:613–617
Kaufman KM, Kelly JA, Herring BJ, Adler AJ, Glenn SB, Namjou B, Frank SG, Dawson SL, Bruner GR, James JA, Harley JB (2006) Evaluation of the genetic association of thePTPN22 R620W polymorphism in familial and sporadic systemic lupus erythematosus. Arthritis Rheum 54:2533–2540
Kawasaki E, Awata T, Ikegami H, Kobayashi T, Maruyama T, Nakanishi K, Shimada A, Uga M, Kurihara S, Kawabata Y, Tanaka S, Kanazawa Y, Lee I, Eguchi K (2006) Systematic search for single nucleotide polymorphisms in a lymphoid tyrosine phosphatase gene (PTPN22): association between a promoter polymorphism and type 1 diabetes in Asian populations. Am J Med Genet A 140:586–593
Krieg AM (1995) CpG DNA: a pathogenic factor in systemic lupus erythematosus? J Clin Immunol 15:284–292
Kyogoku C, Langefeld CD, Ortmann WA, Lee A, Selby S, Carlton VE, Chang M, Ramos P, Baechler EC, Batliwalla FM, Novitzke J, Williams AH, Gillett C, Rodine P, Graham RR, Ardlie KG, Gaffney PM, Moser KL, Petri M, Begovich AB, Gregersen PK, Behrens TW (2004) Genetic Association of the R620W polymorphism of protein tyrosine phosphatase PTPN22 with human SLE. Am J Hum Genet 75:504–507
Lau CS, Yin G, Mok MY (2006) Ethnic and geographical differences in systemic lupus erythematosus: an overview. Lupus 15:715–719
Lea WW, Lee YH (2011) The association between the PTPN22 C1858T polymorphism and systemic lupus erythematosus: a meta-analysis update. Lupus 20:51–57
Lee HS, Korman BD, Le JM, Kastner DL, Remmers EF, Gregersen PK, Bae SC (2009) Genetic risk factors for rheumatoid arthritis differ in Caucasian and Korean populations. Arthritis Rheum 60:364–371
Lee YH, Choi SJ, Ji JD, Song GG (2016) Association between toll-like receptor polymorphisms and systemic lupus erythematosus: a meta-analysis update. Lupus 25:593–601
Lee YH, Rho YH, Choi SJ, Ji JD, Song GG, Nath SK, Harley JB (2007) The PTPN22 C1858T functional polymorphism and autoimmune diseases—a meta-analysis. Rheumatology (Oxford) 46:49–56
Li J, Tao JH, Gao W, Fan Y, Lu MM, Li R, Li XP, Ye DQ (2012) Lack of association of Toll-like receptor 9 polymorphisms with susceptibility to systemic lupus erythematosus in an Asian population: a meta-analysis. Mod Rheumatol 22:550–556
Lu ZY, Jin LW, Niu ZM, Yuan WT, Shen XY, Xue F, Zheng J (2007) Preliminary study on polymorphism of toll-like receptor 9 gene in patients with systemic lupus erythematosus. J Shanghai Jiao Tong University 27:1448–1450 (article in Chinese)
Machado-Contreras JR, Munoz-Valle JF, Cruz A, Salazar-Camarena DC, Marin-Rosales M, Palafox-Sanchez CA (2016) Distribution of PTPN22 polymorphisms in SLE from western Mexico: correlation with mRNA expression and disease activity. Clin Exp Med 16:399–406
Migita K, Miyashita T, Maeda Y, Nakamura M, Yatsuhashi H, Kimura H, Ishibashi H, Eguchi K (2007) Toll-like receptor expression in lupus peripheral blood mononuclear cells. J Rheumatol 34:493–500
Moez P, Soliman E (2012) Association of PTPN22 gene polymorphism and systemic lupus erythematosus in a cohort of Egyptian patients: impact on clinical and laboratory results. Rheumatol Int 32:2753–2758
Morris DL, Sheng Y, Zhang Y, Wang YF, Zhu Z, Tombleson P, Chen L, Cunninghame Graham DS, Bentham J, Roberts AL, Chen R, Zuo X, Wang T, Wen L, Yang C, Liu L, Yang L, Li F, Huang Y, Yin X, Yang S, Rönnblom L, Fürnrohr BG, Voll RE, Schett G, Costedoat-Chalumeau N, Gaffney PM, Lau YL, Zhang X, Yang W, Cui Y, Vyse TJ (2016) Genome-wide association meta-analysis in Chinese and European individuals identifies ten new loci associated with systemic lupus erythematosus. Nat Genet 48:940–946
Munafo MR, Flint J (2004) Meta-analysis of genetic association studies. Trends Genet 20:439–444
Nakano S, Morimoto S, Suzuki J, Nozawa K, Amano H, Tokano Y, Takasaki Y (2008) Role of pathogenic auto-antibody production by Toll-like receptor 9 of B cells in active systemic lupus erythematosus. Rheumatology (Oxford) 47:145–149
Namjou B, Kim-Howard X, Sun C, Adler A, Chung Sharon A, Kaufman Kenneth M, Kelly JA, Glenn Stuart B, Guthridge JM, Scofield Robert H, Kimberly RP, Brown Elizabeth E, Alarcón GS, Edberg Jeffrey C, Kim J-H, Choi J, Ramsey-Goldman R, Petri Michelle A, Reveille JD, Vilá LM, Boackle SA, Freedman BI, Tsao BP, Langefeld CD, Vyse TJ, Jacob CO, Pons-Estel B, Niewold TB, Moser Sivils KL, Merrill JT, Anaya J-M, Gilkeson GS, Gaffney PM, Bae S-C, Alarcón-Riquelme ME, Harley JB, Criswell LA, James JA, Nath SK, Liossis S-N (2013) PTPN22 association in systemic lupus erythematosus (SLE) with respect to individual ancestry and clinical sub-phenotypes. PLoS One 8(8):e69404
Nath SK, Namjou B, Kilpatrick J, Garriott CP, Bruner GR, Scofield RH, Harley JB (2004) A candidate region on 11p13 for systemic lupus erythematosus: a linkage identified in African-American families. J Investig Dermatol Symp Proc 9:64–67
Nath SK, Quintero-Del-Rio AI, Kilpatrick J, Feo L, Ballesteros M, Harley JB (2004) Linkage at 12q24 with systemic lupus erythematosus (SLE) is established and confirmed in hispanic and European American Families. Am J Hum Genet 74:73–82
Ng MW, Lau CS, Chan TM, Wong WH, Lau YL (2005) Polymorphisms of the toll-like receptor 9 (TLR9) gene with systemic lupus erythematosus in Chinese. Rheumatology (Oxford) 44:1456–1457
Okada Y, Shimane K, Kochi Y, Tahira T, Suzuki A, Higasa K, Takahashi A, Horita T, Atsumi T, Ishii T, Okamoto A, Fujio K, Hirakata M, Amano H, Kondo Y, Ito S, Takada K, Mimori A, Saito K, Kamachi M, Kawaguchi Y, Ikari K, Mohammed OW, Matsuda K, Terao C, Ohmura K, Myouzen K, Hosono N, Tsunoda T, Nishimoto N, Mimori T, Matsuda F, Tanaka Y, Sumida T, Yamanaka H, Takasaki Y, Koike T, Horiuchi T, Hayashi K, Kubo M, Kamatani N, Yamada R, Nakamura Y, Yamamoto K (2012) A genome-wide association study identified AFF1 as a susceptibility locus for systemic lupus eyrthematosus in Japanese. PLoS Genet 8:e1002455
Orozco G, Sanchez E, Gonzalez-Gay MA, Lopez-Nevot MA, Torres B, Caliz R, Ortego-Centeno N, Jimenez-Alonso J, Pascual-Salcedo D, Balsa A, de Pablo R, Nunez-Roldan A, Gonzalez-Escribano MF, Martin J (2005) Association of a functional single-nucleotide polymorphism of PTPN22, encoding lymphoid protein phosphatase, with rheumatoid arthritis and systemic lupus erythematosus. Arthritis Rheum 52:219–224
Orozco G, Viatte S, Bowes J, Martin P, Wilson AG, Morgan AW, Steer S, Wordsworth P, Hocking LJ, Barton A, Worthington J, Eyre S, Consortium UKRAG, Wellcome Trust Case Control C, Biologics in Rheumatoid Arthritis G, Genomics Study Syndicate C (2014) Novel rheumatoid arthritis susceptibility locus at 22q12 identified in an extended UK genome-wide association study. Arthritis Rheumatol 66:24–30
Ostanek L, Ostanek-Panka M, Bobrowska-Snarska D, Binczak-Kuleta A, Fischer K, Kaczmarczyk M, Ciechanowicz A, Brzosko M (2014) PTPN22 1858C>T gene polymorphism in patients with SLE: association with serological and clinical results. Mol Biol Rep 41:6195–6200
Panda AK, Pattanaik SS, Tripathy R, Das BK (2013) TLR-9 promoter polymorphisms (T-1237C and T-1486C) are not associated with systemic lupus erythematosus: a case control study and meta-analysis. Hum Immunol 74:1672–1678
Peng XB, Ou LN (2010) Correlation between PTPN22 gene polymorphism and systemic lupus erythematosus in Chinese Han patients. Nan Fang Yi Ke Da Xue Xue Bao 30:2390–2391 (article in Chinese)
Piotrowski P, Lianeri M, Wudarski M, Olesinska M, Jagodzinski PP (2012) Contribution of STAT4 gene single-nucleotide polymorphism to systemic lupus erythematosus in the Polish population. Mol Biol Rep 39:8861–8866
Piotrowski P, Lianeri M, Wudarski M, Olesinska M, Jagodzinski PP (2013) Contribution of toll-like receptor 9 gene single-nucleotide polymorphism to systemic lupus erythematosus. Rheumatol Int 33:1121–1125
Piotrowski P, Lianeri M, Wudarski M, Lacki JK, Jagodziński PP (2008) Contribution of the R620W polymorphism of protein tyrosine phosphatase non-receptor 22 to systemic lupus erythematosus in Poland. Clin Exp Rheumatol 26:1099–1102
Ramachandran R, Sharma V, Rathi M, Yadav AK, Sharma A, Kohli HS, Sakhuja V, Jha V (2012) Association between −1486 T>C and +1174 G>A single nucleotide polymorphisms in TLR9 gene and severity of lupus nephritis. Indian J Nephrol 22:125–129
Ramirez M, Quintana G, Diaz-Gallo LM, Caminos J, Garces M, Cepeda L, Rondon F, Restrepo JF, Egea E, Garavito G, Robledo G, Martin J, Iglesias-Gamarra A (2012) The PTPN22 C1858T variant as a risk factor for rheumatoid arthritis and systemic lupus erythematosus but not for systemic sclerosis in the Colombian population. Clin Exp Rheumatol 30:520–524
Rawlings DJ, Dai X, Buckner JH (2015) The role of PTPN22 risk variant in the development of autoimmunity: finding common ground between mouse and human. J Immunol 194:2977–2984
Reddy MV, Johansson M, Sturfelt G, Jonsen A, Gunnarsson I, Svenungsson E, Rantapaa-Dahlqvist S, Alarcon-Riquelme ME (2005) The R620W C/T polymorphism of the gene PTPN22 is associated with SLE independently of the association of PDCD1. Genes Immun 6:658–662
Rupasree Y, Naushad SM, Rajasekhar L, Uma A, Kutala VK (2015) Association of TLR4 D299G, T399I TLR9 1486TC TIRAP S180L and TNF-a promoter (1031, 863, 857) polymorphisms with risk for systemic lupus erythematosus among South Indians. Lupus 24:50–57
Sánchez E, Callejas-Rubio JL, Sabio JM, Gónzalez-Gay MA, Jimenez-Alonso J, Micó L, de Ramón E, Camps M, Suarez A, Gutierrez C, Garcia-Portales R, Tolosa C, Ortego-Centeno N, Sánchez-Román J, Garcia-Hernández FJ, Gónzalez-Escribano MF, Martin J (2009) Investigation of TLR5 and TLR7 as candidate genes for susceptibility to systemic lupus erythematosus. Clin Exp Rheumatol 27:267–271
Sanchez E, Comeau ME, Freedman BI, Kelly JA, Kaufman KM, Langefeld CD, Brown EE, Alarcon GS, Kimberly RP, Edberg JC, Ramsey-Goldman R, Petri M, Reveille JD, Vila LM, Merrill JT, Tsao BP, Kamen DL, Gilkeson GS, James JA, Vyse TJ, Gaffney PM, Jacob CO, Niewold TB, Richardson BC, Harley JB, Alarcón-Riquelme ME, Sawalha AH, International Consortium on the Genetics of Systemic Lupus Erythematosus (2011) Identification of novel genetic susceptibility loci in African American lupus patients in a candidate gene association study. Arthritis Rheum 63:3493–3501
Sandling JK, Garnier S, Sigurdsson S, Wang C, Nordmark G, Gunnarsson I, Svenungsson E, Padyukov L, Sturfelt G, Jonsen A, Bengtsson AA, Truedsson L, Eriksson C, Rantapaa-Dahlqvist S, Malarstig A, Strawbridge RJ, Hamsten A, Criswell LA, Graham RR, Behrens TW, Eloranta ML, Alm G, Rönnblom L, Syvänen AC (2011) A candidate gene study of the type I interferon pathway implicates IKBKE and IL8 as risk loci for SLE. Eur J Hum Genet 19:479–484
Sawalha AH, Namjou B, Nath SK, Kilpatrick J, Germundson A, Kelly JA, Hutchings D, James J, Harley J (2002) Genetic linkage of systemic lupus erythematosus with chromosome 11q14 (SLEH1) in African-American families stratified by a nucleolar antinuclear antibody pattern. Genes Immun 3(Suppl 1):S31–S34
Shahin RM, El Khateeb E, Khalifa RH, El Refai RM (2016) Contribution of toll-like receptor 9 gene single-nucleotide polymorphism to systemic lupus erythematosus in Egyptian Patients. Immunol Invest 45:235–242
Shi L, Wei Y, Xun W, Han D (2013) Meta-analysis of the correlation between PTPN22 gene polymorphisms and susceptibility to systemic lupus erythematosus. Asia Pac J Public Health 25:22S–29S
Song WQ, Li HH, Chen HB, Yuan JS, Yin XJ (2009) Relationship between polymorphism sites of IRF5, TLR-9 and SLE patients in Shandong Han population. Zhonghua Yi Xue Za Zhi 13:1210–1212 (article in Chinese)
Song X, Song WQ (2011) Relativity study between TLR-9 gene polymorphism and SLE. Med Labor Sci Clin 22:19–21 (article in Chinese)
Tang L, Wang Y, Zheng S, Bao M, Zhang Q, Li J (2016) PTPN22 polymorphisms, but not R620 W, were associated with the genetic susceptibility of systemic lupus erythematosus and rheumatoid arthritis in a Chinese Han population. Hum Immunol 77:692–698
Tao K, Fujii M, Tsukumo S, Maekawa Y, Kishihara K, Kimoto Y, Horiuchi T, Hisaeda H, Akira S, Kagami S, Yasutomo K (2007) Genetic variations of Toll-like receptor 9 predispose to systemic lupus erythematosus in Japanese population. Ann Rheum Dis 66:905–909
Tsao BP, Cantor RM, Grossman JM, Kim SK, Strong N, Lau CS, Chen CJ, Shen N, Ginzler EM, Goldstein R, Kalunian KC, Arnett FC, Wallace DJ, Hahn BH (2002) Linkage and interaction of loci on 1q23 and 16q12 may contribute to susceptibility to systemic lupus erythematosus. Arthritis Rheum 46:2928–2936
Vandiedonck C, Capdevielle C, Giraud M, Krumeich S, Jais JP, Eymard B, Tranchant C, Gajdos P, Garchon HJ (2006) Association of the PTPN22*R620W polymorphism with autoimmune myasthenia gravis. Ann Neurol 59:404–407
Viken MK, Amundsen SS, Kvien TK, Boberg KM, Gilboe IM, Lilleby V, Sollid LM, Forre OT, Thorsby E, Smerdel A, Lie BA (2005) Association analysis of the 1858C>T polymorphism in the PTPN22 gene in juvenile idiopathic arthritis and other autoimmune diseases. Genes Immun 6:271–273
Wang D, Zhang C, Zhou Z, Pei F (2016) TLR9 polymorphisms and systemic lupus erythematosus risk: an update meta-analysis study. Rheumatol Int 36:585–595
Wen SJ, Wu FY, Fang L, Liu H, Zheng WJ, Lin YK (2015) Associations of genetic polymorphisms of TLR5, TLR9 and transduction molecules in MyD88 signaling pathway with systemic lupus erythematosus in Zhuang and Han ethnics of Guangxi province, China. Int J Clin Exp Med 8(5):7872–7880
Wong M, Tsao BP (2006) Current topics in human SLE genetics. Springer Semin Immunopathol 28:97–107
Yang W, Shen N, Ye DQ, Liu Q, Zhang Y, Qian XX, Hirankarn N, Ying D, Pan HF, Mok CC, Chan TM, Wong RW, Lee KW, Mok MY, Wong SN, Leung AM, Li XP, Avihingsanon Y, Wong CM, Lee TL, Ho MH, Lee PP, Chang YK, Li PH, Li RJ, Zhang L, Wong WH, Ng IO, Lau CS, Sham PC, Lau YL (2010) Genome-wide association study in asian populations identifies variants in ETS1 and WDFY4 associated with systemic lupus erythematosus. PLoS Genet 6:1–11
Yang Z, Liang Y, Qin B, Li C, Zhong R (2012) TLR9 polymorphisms and systemic lupus erythematosus risk in Asians: a meta-analysis study. Cytokine 57:282–289
Zeng QY, Chen R, Darmawan J, Xiao ZY, Chen SB, Wigley R, Le Chen S, Zhang NZ (2008) Rheumatic diseases in China. Arthritis Res Ther 10:R17
Zhang J, Zhu Q, Meng F, Lei H, Zhao Y (2014) Association study of TLR-9 polymorphisms and systemic lupus erythematosus in northern Chinese Han population. Gene 533:385–388
Zhang Z, Cheng Y, Zhou X, Li Y, Gao J, Han J, Quan C, He S, Lv Y, Hu D, Zhu K, Sun L, Yang S, Zhang X (2011) Polymorphisms at 16p13 are associated with systemic lupus erythematosus in the Chinese population. J Med Genet 48:69–72
Zhang ZH, Chen F, Zhang XL, Jin Y, Bai J, Fu SB (2008) PTPN22 allele polymorphisms in 15 Chinese populations. Int J Immunogenet 35:433–437
Zheng J, Ibrahim S, Petersen F, Yu X (2012) Meta-analysis reveals an association of PTPN22 C1858T with autoimmune diseases, which depends on the localization of the affected tissue. Genes Immun 13:641–652
Zhong H, Li XL, Li M, Hao LX, Chen RW, Xiang K, Qi XB, Ma RZ, Su B (2011) Replicated associations of TNFAIP3, TNIP1 and ETS1 with systemic lupus erythematosus in a southwestern Chinese population. Arthritis Res Ther 13:R186
Zhou XJLJ, Cheng WR, Yu L, Zhao MH, Zhang H (2010) Association of TLR9 gene polymorphisms with lupus nephritis in a Chinese Han. Clin Exp Rheumatol 28:397–400
Zhu XW, Wang Y, Wei YH, Zhao PP, Wang XB, Rong JJ, Zhong WY, Zhang XW, Wang L, Zheng HF (2016) Comprehensive Assessment of the Association between FCGRs polymorphisms and the risk of systemic lupus erythematosus: evidence from a Meta-Analysis. Sci Rep 6:31617
Acknowledgements
This study was supported by the National Natural Science Foundation of China (81501145), the Zhejiang Provincial Natural Science Foundation for Distinguished Young Scholars of China (LR17H070001), the State Key Development Program for Basic Research of China (973 Program, 2014CB541701), the HZNUARI-Pilot Research Grant. The funding agencies had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript. We thank the peer reviewers for their thorough and helpful review of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests that might be perceived to influence the results and/or discussion reported in this paper. This study re-analyzed the previous published data; therefore, this study did not involve original human participants.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hu, LY., Cheng, Z., Zhang, B. et al. Associations between PTPN22 and TLR9 polymorphisms and systemic lupus erythematosus: a comprehensive meta-analysis. Arch Dermatol Res 309, 461–477 (2017). https://doi.org/10.1007/s00403-017-1745-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-017-1745-0